Abstract
Purpose
To investigate the refractive and biometrical developments of children with retinopathy of prematurity (ROP) who received laser photocoagulation (LP) or intravitreal ranibizumab injection as treatment.
Methods
This case–control study involved cases with Zone II Stage 3 ROP. Fourteen children (28 eyes) who received single LP were included in the laser group, and 14 children (27 eyes) who received single intravitreal ranibizumab injection were included in the injection group. The mean age at operation was 37.00±1.72 and 36.36±1.66 weeks for the laser and injection groups, respectively (P=0.161), and refraction measurements and biometry were performed at the mean age of 5.00±1.63 and 5.00±0.94 years for the laser and injection groups, respectively (P=1.000). Spherical equivalent (SE) after mydriatic refraction and best corrected visual acuity (BCVA) were measured by refraction test. Central corneal thickness (CCT), anterior corneal surface curvature and curvature radius, anterior chamber depth (ACD), lens thickness (LT) and axial length (AL) were measured by biometry using the IOL Master700 biometric instrument (Carl Zeiss Meditec AG). The biometrical images were reanalysed using a self-developed program in MATLAB (R2016a, MathWorks, Inc.) to obtain additional eye parameters, including the curvatures of the posterior cornea and the anterior and posterior surfaces of the lens. SPSS (V.23.0) was used for statistical analysis. Independent sample t test was used to compare the eyeball biological and refractive state measures of the two groups, and Pearson correlation coefficient was used to evaluate the correlation between SE and the biological parameters.
Results
-
1.
-
(1)
Cornea-related parameters: CCT (0.54±0.04mm vs 0.55±0.02mm, P>0.05), anterior corneal surface curvature radius (7.56±0.26 mm vs 7.67±0.43mm, P>0.05) and posterior corneal surface curvature radius (6.82±0.27mm vs 6.79±0.42mm, P>0.05).
-
(2)
ACD (3.21 ± 0.25mm vs 3.22 ± 0.19mm, P>0.05).
-
(3)
Lens-related parameters: anterior lens surface curvature radius (10.04±0.89mm vs 9.82±1.08mm, P>0.05), posterior lens surface curvature radius (5.49±0.55mm vs 5.92±0.73mm, P<0.05) and LT (3.80±0.14mm vs 3.59±0.16mm, P<0.05).
-
(4)
AL (21.82±1.07 vs 22.68±1.61, P<0.05).
-
(5)
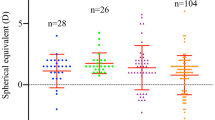
Parameters related to refractive state: SE (−2.43±3.56 vs −0.53±3.12, P<0.05) and BCVA (log MAR, 0.17±0.14 vs 0.21±0.18, P>0.05).
-
(1)
-
2.
-
(1)
The SE of children in the laser group was positively correlated with LT (r=0.438, P<0.05), negatively correlated with ACD (r=−0.437, P<0.05) and had no significant correlation with other eyeball biological indicators (P>0.05).
-
(2)
The SE of children in the injection group was negatively correlated with AL (r=−0.537, P<0.05), positively correlated with CCT (r=0.455, P<0.05) and had no significant correlation with other eyeball biological indicators (P>0.05).
-
(1)
Conclusion
LP and intravitreal ranibizumab injection as ROP treatments produce myopic refraction with increased degree of myopia in children who received LP than in children who received ranibizumab injection. The increased myopia after LP is due to the increases in LT and posterior lens curvature and a shallow ACD.
Similar content being viewed by others
References
Higgins RD (2019) Oxygen saturation and retinopathy of prematurity. Clin Perinatol 46:593–599
Broxterman EC, Hug DA (2016) Retinopathy of prematurity: a review of current screening guidelines and treatment options. Missouri Med 113:187–190
Hartnett ME (2017) Advances in understanding and management of retinopathy of prematurity. Surv Ophthalmol 62:257–276
Chew EY (2015) There is level 1 evidence for intensive glycemic control for reducing the progression of diabetic retinopathy in persons with type 2 diabetes. Endocrine 49:1–3
Mintz-Hittner HA, Geloneck MM (2016) Review of effects of anti-VEGF treatment on refractive error. Eye Brain 8:135–140
Dhawan A, Dogra M, Vinekar A, Gupta A, Dutta S (2008) Structural sequelae and refractive outcome after successful laser treatment for threshold retinopathy of prematurity. J Pediatr Ophthalmol Strabismus 45:356–361
Yang CS, Wang AG, Sung CS, Hsu WM, Lee FL, Lee SM (2010) Long-term visual outcomes of laser-treated threshold retinopathy of prematurity: a study of refractive status at 7 years. Eye (London, England) 24:14–20
Harder BC, Schlichtenbrede FC, von Baltz S, Jendritza W, Jendritza B, Jonas JB (2013) Intravitreal bevacizumab for retinopathy of prematurity: refractive error results. Am J Ophthalmol 155:1119-1124.e1111
Kuo HK, Sun IT, Chung MY, Chen YH (2015) Refractive error in patients with retinopathy of prematurity after laser photocoagulation or bevacizumab monotherapy. Ophthalmol Int J Ophthalmol Z Augenheilkd 234:211–217
Mutlu FM, Küçükevcilioğlu M, Ceylan OM, Altınsoy HI, Sarıcı SU (2013) Risk factor analysis for long-term unfavorable ocular outcomes in children treated for retinopathy of prematurity. Turk J Pediatr 55:35–41
Chiang MF, Quinn GE, Fielder AR, Ostmo SR, Paul Chan RV, Berrocal A, Binenbaum G, Blair M, Peter Campbell J, Capone A Jr, et al. (2021) International classification of retinopathy of prematurity, third edition. Ophthalmology 128:e51–e68.
Ophthalmology Group, P.S.O.C.M.A (2022) Expert consensus on the treatment of retinopathy of prematurity. Chin J Ocular Fundus Dis 38:10–13
Mahroo OA, Williams C, Hysi PG, Williams KM, Kailani O, Thompson J, Cumberland PM, Guggenheim JA, Rahi JS, Harrad RA et al (2015) Interocular asymmetries in axial length and refractive error in 4 cohorts. Ophthalmology 122:648–649
Wang Y, Zhao R, Pi L (2020) Analysis of the correlation between refractive state and refractive parameters in children aged 3–12 years. Health Med Res Pract 17:22–26
Bueno-Gimeno I, España-Gregori E, Gene-Sampedro A, Lanzagorta-Aresti A, Piñero-Llorens DP (2014) Relationship among corneal biomechanics, refractive error, and axial length. Optom Vis Sci 91:507–513
Touzeau O, Allouch C, Borderie V, Kopito R, Laroche L (2003) Correlation between refraction and ocular biometry. J Fr Ophtalmol 26:355–363
Fam HB, How AC, Baskaran M, Lim KL, Chan YH, Aung T (2006) Central corneal thickness and its relationship to myopia in Chinese adults. Br J Ophthalmol 90:1451–1453
Jonas JB, Xu L (2014) Histological changes of high axial myopia. Eye (London, England) 28:113–117
Geloneck MM, Chuang AZ, Clark WL, Hunt MG, Norman AA, Packwood EA, Tawansy KA, Mintz-Hittner HA, Group, F.T.B.-R.C. (2014) Refractive outcomes following bevacizumab monotherapy compared with conventional laser treatment: a randomized clinical trial. JAMA Ophthalmol 132:1327–1333
Shah PK, Narendran V, Tawansy KA, Raghuram A, Narendran K (2007) Intravitreal bevacizumab (Avastin) for post laser anterior segment ischemia in aggressive posterior retinopathy of prematurity. Indian J Ophthalmol 55:75–76
Sangtam T, Vinekar A, Maheshwar B, Dogra MR, Eong KG (2007) Intravitreal bevacizumab (Avastin) for post-laser photocoagulation anterior segment ischemia in aggressive posterior retinopathy of prematurity. Indian J Ophthalmol 55:317; author reply 317-318
Acar DE, Acar U, Tunay ZO, Arman A, Barak A (2021) Effects of diode laser photocoagulation treatment on ocular biometric parameters in premature infants with retinopathy of prematurity. Int J Ophthalmol 14:277–282
Bashinsky AL (2017) Retinopathy of prematurity. N C Med J 78:124–128
Stahl A, Göpel W (2015) Screening and treatment in retinopathy of prematurity. Deutsches Arzteblatt Int 112:730–735
Mintz-Hittner HA, Kennedy KA, Chuang AZ (2011) Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. New Engl J Med 364:603–615
Mintz-Hittner HA, Kuffel RR Jr. (2008) Intravitreal injection of bevacizumab (avastin) for treatment of stage 3 retinopathy of prematurity in zone I or posterior zone II. Retina (Philadelphia, Pa.) 28:831–838
Mueller B, Salchow DJ, Waffenschmidt E, Joussen AM, Schmalisch G, Czernik C, Bührer C, Schunk KU, Girschick HJ, Winterhalter S (2017) Treatment of type I ROP with intravitreal bevacizumab or laser photocoagulation according to retinal zone. Br J Ophthalmol 101:365–370
Zhang G, Yang M, Zeng J, Vakros G, Su K, Chen M, Li H, Tian R, Li N, Tang S et al. (2017) Comparison of intravitreal injection of ranibizumab versus laser therapy for zone II treatment-requiring retinopathy OF prematurity. Retina (Philadelphia, Pa.), 37:710–717.
Huang J, Wang Z, Wu Z, Li Z, Lai K, Ge J (2015) Comparison of ocular biometry between eyes with chronic primary angle-closure glaucoma and their fellow eyes with primary angle-closure or primary angle-closure suspect. J Glaucoma 24:323–327
Zhang W, Cheng Y, Huang H, Wang G, Wang Z (2019) Effect of intraocular lens displacement on diopter after cataract surgery in high myopia eyes. Rec Adv Ophthalmol 39:376–378
Qi M, Chen Q, Zeng Q (2017) Changes of lens thickness, position and influence factors in high myopia. Chin J Pract Ophthalmol 35:256–260
Yang CS, Wang AG, Shih YF, Hsu WM (2013) Long-term biometric optic components of diode laser-treated threshold retinopathy of prematurity at 9 years of age. Acta Ophthalmol 91:e276-282
McLoone EM, O’Keefe M, McLoone SF, Lanigan BM (2006) Long-term refractive and biometric outcomes following diode laser therapy for retinopathy of prematurity. J AAPOS 10:454–459
Wang J, Ren X, Shen L, Yanni SE, Leffler JN, Birch EE (2013) Development of refractive error in individual children with regressed retinopathy of prematurity. Investig Ophthalmol Vis Sci 54:6018–6024
Smith EL 3rd, Kee CS, Ramamirtham R, Qiao-Grider Y, Hung LF (2005) Peripheral vision can influence eye growth and refractive development in infant monkeys. Investig Ophthalmol Vis Sci 46:3965–3972
Lue CL, Hansen RM, Reisner DS, Findl O, Petersen RA, Fulton AB (1995) The course of myopia in children with mild retinopathy of prematurity. Vis Res 35:1329–1335
Funding
This work was supported by Shenzhen Key Medical Discipline Construction Fund (No. SZXK038), Shenzhen Fund for Guangdong Provincial High-level Clinical Key Specialties (No. SZGSP014) and Shenzhen-Hong Kong Co-financing Project (SGDX20190920110403741).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Consent to participate
This study followed the spirit of the Declaration of Helsinki, and the legal guardians of the children voluntarily signed the informed consent.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiaofeng Lu and Xianlu Zeng are co-first authors.
Rights and permissions
About this article
Cite this article
Lu, X., Zeng, X., Chen, M. et al. Refractive and biometrical characteristics of children with retinopathy of prematurity who received laser photocoagulation or intravitreal ranibizumab injection. Graefes Arch Clin Exp Ophthalmol 260, 3213–3219 (2022). https://doi.org/10.1007/s00417-022-05663-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05663-0