Abstract
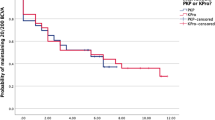
Penetrating keratoplasty (PKP) yields excellent results for restoring vision in end-stage corneal diseases. However, its success is limited to high-risk diseases such as aniridia, chemical burns, autoimmune corneal diseases, and herpetic eye disease. Boston type 1 keratoprosthesis (BKPro) offers another option to these patients. Since 1992, improvements in perioperative management and device construction have significantly increased the use of BKPro worldwide and challenged the therapeutic role of PKP in these patients. This review aims to evaluate BKPro’s place in the treatment algorithm of these high-risk patients to assist surgeons’ decision-making. PKP and BKPro are compared in three outcome categories: visual acuity, graft retention and failure, and complications profile. Special attention is given to comparing secondary BKPro versus repeated PKP as well as primary BKPro versus primary PKP. We conclude that secondary BKPro bears a better prognosis than repeated PKP in most high-risk patients. Similarly, primary BKPro likely confers improved outcomes over primary PKP in most high-risk recipients. However, current evidence is based on retrospective designs, and controlled prospective randomized trials are required to validate these conclusions.

Similar content being viewed by others
References
Zirm E (1906) Eine erfolgreiche totale Keratoplastik. Albrecht Von Graefes Arch Ophthalmol 64:580–593. https://doi.org/10.1007/BF01949227
Singh R, Gupta N, Vanathi M, Tandon R (2019) Corneal transplantation in the modern era. Indian J Med Res 150:7–22. https://doi.org/10.4103/ijmr.IJMR_141_19
Driver TH, Aravena C, Duong HNV, Christenbury JG, Yu F, Basak SK, Aldave AJ (2018) Outcomes of the Boston type I keratoprosthesis as the primary penetrating corneal procedure. Cornea 37:1400–1407. https://doi.org/10.1097/ico.0000000000001735
Fadous R, Levallois-Gignac S, Vaillancourt L, Robert MC, Harissi-Dagher M (2015) The Boston keratoprosthesis type 1 as primary penetrating corneal procedure. Br J Ophthalmol 99:1664–1668. https://doi.org/10.1136/bjophthalmol-2014-306161
Kang KB, Karas FI, Rai R, Hallak JA, Kang JJ, de la Cruz J, Cortina MS (2018) Five year outcomes of Boston type I keratoprosthesis as primary versus secondary penetrating corneal procedure in a matched case control study. PLoS ONE 13:e0192381. https://doi.org/10.1371/journal.pone.0192381
Chen M, Ng SM, Akpek EK, Ahmad S (2020) Artificial corneas versus donor corneas for repeat corneal transplants. Cochrane Database Syst Rev 5:Cd009561. https://doi.org/10.1002/14651858.CD009561.pub3
Park CY, Lee JK, Gore PK, Lim CY, Chuck RS (2015) Keratoplasty in the United States: A 10-Year Review from 2005 through 2014. Ophthalmology 122:2432–2442. https://doi.org/10.1016/j.ophtha.2015.08.017
Williams KA, Lowe M, Bartlett C, Kelly T-L, Coster DJ, Contributors oBoA, (2008) risk factors for human corneal graft failure within the Australian corneal graft registry. Transplantation 86:1720–1724. https://doi.org/10.1097/TP.0b013e3181903b0a
Barraquer RI, Pareja-Arico L, Gomez-Benlloch A, Michael R (2019) Risk factors for graft failure after penetrating keratoplasty. Medicine (Baltimore) 98:e15274. https://doi.org/10.1097/MD.0000000000015274
Harissi-Dagher M, Slim E (2019) Boston keratoprosthesis type 1. J Fr Ophtalmol 42:295–302. https://doi.org/10.1016/j.jfo.2018.08.010
Lee R, Khoueir Z, Tsikata E, Chodosh J, Dohlman CH, Chen TC (2017) Long-term visual outcomes and complications of Boston keratoprosthesis type II implantation. Ophthalmology 124:27–35. https://doi.org/10.1016/j.ophtha.2016.07.011
Fu L, Hollick EJ (2021) Artificial cornea transplantation. StatPearls. StatPearls Publishing Copyright © 2021, StatPearls Publishing LLC., Treasure Island (FL)
Ahmad S, Mathews PM, Lindsley K, Alkharashi M, Hwang FS, Ng SM, Aldave AJ, Akpek EK (2016) Boston type 1 keratoprosthesis versus repeat donor keratoplasty for corneal graft failure: a systematic review and meta-analysis. Ophthalmology 123:165–177. https://doi.org/10.1016/j.ophtha.2015.09.028
Chen Y, Wang C, Liu Q, Wang Z, Gao M (2020) Comparison of the clinical efficacy of Boston keratoprosthesis type i and repetitive penetrating keratoplasty for refractory keratopathy. J Craniofac Surg 31:e194–e199. https://doi.org/10.1097/SCS.0000000000006164
Milad D, Harissi-Dagher M (2020) Comparison of the clinical efficacy of Boston keratoprosthesis type i and repetitive penetrating keratoplasty for refractory keratopathy: comment. J Craniofac Surg 31:1495. https://doi.org/10.1097/SCS.0000000000006554
Sutton G, Hodge C, McGhee CN (2008) Rapid visual recovery after penetrating keratoplasty for keratoconus. Clin Exp Ophthalmol 36:725–730. https://doi.org/10.1111/j.1442-9071.2008.01900.x
Silbiger JS, Cohen EJ, Laibson PR (1996) The rate of visual recovery after penetrating keratoplasty for keratoconus. CLAO J 22:266–269
Dunlap K, Chak G, Aquavella JV, Myrowitz E, Utine CA, Akpek E (2010) Short-term visual outcomes of Boston type 1 keratoprosthesis implantation. Ophthalmology 117:687–692. https://doi.org/10.1016/j.ophtha.2009.09.024
El-Khoury J, Mustafa M, Daoud R, Harissi-Dagher M (2021) Time to achieve best postoperative visual acuity following Boston keratoprosthesis surgery. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2020-317483
Szigiato AA, Bostan C, Nayman T, Harissi-Dagher M (2020) Long-term visual outcomes of the Boston type I keratoprosthesis in Canada. Br J Ophthalmol 104:1601–1607. https://doi.org/10.1136/bjophthalmol-2019-315345
Nayman T, Bostan C, Szigiato AA, Harissi-Dagher M (2021) Long-term outcomes following primary versus secondary Boston keratoprosthesis type 1 implantation. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2020-317606
Shah KJ, Cheung AY, Holland EJ (2018) Intermediate-term and long-term outcomes with the Boston type 1 keratoprosthesis in Aniridia. Cornea 37:11–14. https://doi.org/10.1097/ICO.0000000000001412
Hassanaly SI, Talajic JC, Harissi-Dagher M (2014) Outcomes following Boston type 1 keratoprosthesis implantation in aniridia patients at the University of Montreal. Am J Ophthalmol 158(270–276):e271. https://doi.org/10.1016/j.ajo.2014.05.009
Akpek EK, Harissi-Dagher M, Petrarca R, Butrus SI, Pineda R 2nd, Aquavella JV, Dohlman CH (2007) Outcomes of Boston keratoprosthesis in aniridia: a retrospective multicenter study. Am J Ophthalmol 144:227–231. https://doi.org/10.1016/j.ajo.2007.04.036
Rixen JJ, Cohen AW, Kitzmann AS, Wagoner MD, Goins KM (2013) Treatment of aniridia with Boston type I keratoprosthesis. Cornea 32:947–950. https://doi.org/10.1097/ICO.0b013e318281724a
Kremer I, Rajpal RK, Rapuano CJ, Cohen EJ, Laibson PR (1993) Results of penetrating keratoplasty in aniridia. Am J Ophthalmol 115:317–320. https://doi.org/10.1016/s0002-9394(14)73581-0
Tiller AM, Odenthal MT, Verbraak FD, Gortzak-Moorstein N (2003) The influence of keratoplasty on visual prognosis in aniridia: a historical review of one large family. Cornea 22:105–110. https://doi.org/10.1097/00003226-200303000-00004
Shanbhag SS, Saeed HN, Paschalis EI, Chodosh J (2018) Boston keratoprosthesis type 1 for limbal stem cell deficiency after severe chemical corneal injury: a systematic review. Ocul Surf 16:272–281. https://doi.org/10.1016/j.jtos.2018.03.007
Shimazaki J, Shimmura S, Tsubota K (2004) Donor source affects the outcome of ocular surface reconstruction in chemical or thermal burns of the cornea. Ophthalmology 111:38–44. https://doi.org/10.1016/j.ophtha.2003.02.003
Kuckelkorn R, Keller G, Redbrake C (2001) Long-term results of large diameter keratoplasties in the treatment of severe chemical and thermal eye burns. Klin Monbl Augenheilkd 218:542–552. https://doi.org/10.1055/s-2001-17136
Alexander JK, Basak SK, Padilla MD, Yu F, Aldave AJ (2015) International outcomes of the Boston type I keratoprosthesis in Stevens-Johnson syndrome. Cornea 34:1387–1394. https://doi.org/10.1097/ICO.0000000000000619
Sayegh RR, Ang LP, Foster CS, Dohlman CH (2008) The Boston keratoprosthesis in Stevens-Johnson syndrome. Am J Ophthalmol 145:438–444. https://doi.org/10.1016/j.ajo.2007.11.002
Yaghouti F, Nouri M, Abad JC, Power WJ, Doane MG, Dohlman CH (2001) Keratoprosthesis: preoperative prognostic categories. Cornea 20:19–23. https://doi.org/10.1097/00003226-200101000-00003
Tugal-Tutkun I, Akova YA, Foster CS (1995) Penetrating keratoplasty in cicatrizing conjunctival diseases. Ophthalmology 102:576–585. https://doi.org/10.1016/s0161-6420(95)30980-3
Brown CR, Wagoner MD, Welder JD, Cohen AW, Goins KM, Greiner MA, Kitzmann AS (2014) Boston keratoprosthesis type 1 for herpes simplex and herpes zoster keratopathy. Cornea 33:801–805. https://doi.org/10.1097/ICO.0000000000000164
Limaiem R, Mnasri H, Merdassi A, El Maazi A, El Euch K, Mghaieth F, El Matri L (2009) Therapeutic penetrating keratoplasty in herpes infected eye. Bull Soc Belge Ophtalmol 311:37–41
Kosker M, Duman F, Suri K, Hammersmith KM, Nagra PK, Rapuano CJ (2013) Long-term results of keratoplasty in patients with herpes zoster ophthalmicus. Cornea 32:982–986. https://doi.org/10.1097/ICO.0b013e318289897e
Khan BF, Harissi-Dagher M, Pavan-Langston D, Aquavella JV, Dohlman CH (2007) The Boston keratoprosthesis in herpetic keratitis. Arch Ophthalmol 125:745–749. https://doi.org/10.1001/archopht.125.6.745
Fry M, Aravena C, Yu F, Kattan J, Aldave AJ (2018) Long-term outcomes of the Boston type I keratoprosthesis in eyes with previous herpes simplex virus keratitis. Br J Ophthalmol 102:48–53. https://doi.org/10.1136/bjophthalmol-2017-310186
Inoue K, Amano S, Oshika T, Tsuru T (2001) Risk factors for corneal graft failure and rejection in penetrating keratoplasty. Acta Ophthalmol Scand 79:251–255. https://doi.org/10.1034/j.1600-0420.2001.790308.x
Marsh RJ, Cooper M (1989) Ocular surgery in ophthalmic zoster. Eye (Lond) 3(Pt 3):313–317. https://doi.org/10.1038/eye.1989.45
Muzychuk AK, Durr GM, Shine JJ, Robert MC, Harissi-Dagher M (2017) No light perception outcomes following Boston keratoprosthesis type 1 surgery. Am J Ophthalmol 181:46–54. https://doi.org/10.1016/j.ajo.2017.06.012
Ahmad S, Mathews PM, Srikumaran D, Aldave AJ, Lenis T, Aquavella JV, Hannush SB, Belin M, Akpek EK (2016) Outcomes of repeat Boston type 1 keratoprosthesis implantation. Am J Ophthalmol 161(181–187):e181. https://doi.org/10.1016/j.ajo.2015.10.012
Talajic JC, Agoumi Y, Gagne S, Moussally K, Harissi-Dagher M (2012) Prevalence, progression, and impact of glaucoma on vision after Boston type 1 keratoprosthesis surgery. Am J Ophthalmol 153(267–274):e261. https://doi.org/10.1016/j.ajo.2011.07.022
Netland PA, Terada H, Dohlman CH (1998) Glaucoma associated with keratoprosthesis. Ophthalmology 105:751–757. https://doi.org/10.1016/S0161-6420(98)94034-9
Aldave AJ, Kamal KM, Vo RC, Yu F (2009) The Boston type I keratoprosthesis: improving outcomes and expanding indications. Ophthalmology 116:640–651. https://doi.org/10.1016/j.ophtha.2008.12.058
Stolowy N, Callet M, Beylerian M, Hoffart L, Yin GHW (2018) The Boston keratoprosthesis in the management of corneal blindness: indications and limitations. J Fr Ophtalmol 41:642–649. https://doi.org/10.1016/j.jfo.2017.11.039
Robert MC, Pomerleau V, Harissi-Dagher M (2013) Complications associated with Boston keratoprosthesis type 1 and glaucoma drainage devices. Br J Ophthalmol 97:573–577. https://doi.org/10.1136/bjophthalmol-2012-302770
Crnej A, Paschalis EI, Salvador-Culla B, Tauber A, Drnovsek-Olup B, Shen LQ, Dohlman CH (2014) Glaucoma progression and role of glaucoma surgery in patients with Boston keratoprosthesis. Cornea 33:349–354. https://doi.org/10.1097/ICO.0000000000000067
Geoffrion D, Harissi-Dagher M (2021) Glaucoma risk factors and outcomes following Boston keratoprosthesis type 1 surgery. Am J Ophthalmol 226:56–67. https://doi.org/10.1016/j.ajo.2021.01.006
Geoffrion D, Robert MC, Chodosh J, Di Polo A, Harissi-Dagher M (2021) Perspectives for preclinical mouse models of glaucoma after Boston keratoprosthesis type 1. Exp Eye Res 208:108615. https://doi.org/10.1016/j.exer.2021.108615
Akpek EK, Karakus S, Yohannan J, Jabbour S, Sotimehin AE, Li G, Ramulu PY (2021) Reliability of several glaucoma tests in patients with Boston type 1 keratoprosthesis. Cornea. https://doi.org/10.1097/ico.0000000000002800
Hong SW, Koenigsman H, Ren R, Yang H, Gardiner SK, Reynaud J, Kinast RM, Mansberger SL, Fortune B, Demirel S, Burgoyne CF (2018) Glaucoma specialist optic disc margin, rim margin, and rim width discordance in glaucoma and glaucoma suspect eyes. Am J Ophthalmol 192:65–76. https://doi.org/10.1016/j.ajo.2018.04.022
Harissi-Dagher M, Dohlman CH (2008) The Boston keratoprosthesis in severe ocular trauma. Can J Ophthalmol 43:165–169. https://doi.org/10.3129/i08-009
Tanure MA, Cohen EJ, Grewal S, Rapuano CJ, Laibson PR (2000) Penetrating keratoplasty for varicella-zoster virus keratopathy. Cornea 19:135–139. https://doi.org/10.1097/00003226-200003000-00003
Tanaka TS, Hood CT, Kriegel MF, Niziol L, Soong HK (2019) Long-term outcomes of penetrating keratoplasty for corneal complications of herpes zoster ophthalmicus. Br J Ophthalmol 103:1710–1715. https://doi.org/10.1136/bjophthalmol-2018-313602
Zheng C, Yu F, Tseng VL, Lum F, Coleman AL (2018) Risk of glaucoma surgery after corneal transplant surgery in Medicare patients. Am J Ophthalmol 192:104–112. https://doi.org/10.1016/j.ajo.2018.05.004
Khan BF, Harissi-Dagher M, Khan DM, Dohlman CH (2007) Advances in Boston keratoprosthesis: enhancing retention and prevention of infection and inflammation. Int Ophthalmol Clin 47:61–71. https://doi.org/10.1097/IIO.0b013e318036bd8b
Davies E, Chodosh J (2016) Infections after keratoprosthesis. Curr Opin Ophthalmol 27:373–377. https://doi.org/10.1097/ICU.0000000000000270
Lee WB, Shtein RM, Kaufman SC, Deng SX, Rosenblatt MI (2015) Boston keratoprosthesis: outcomes and complications: a report by the American Academy of Ophthalmology. Ophthalmology 122:1504–1511. https://doi.org/10.1016/j.ophtha.2015.03.025
Kim MJ, Yu F, Aldave AJ (2013) Microbial keratitis after Boston type I keratoprosthesis implantation: incidence, organisms, risk factors, and outcomes. Ophthalmology 120:2209–2216. https://doi.org/10.1016/j.ophtha.2013.05.001
Lee T, Robbins CB, Wisely CE, Grewal DS, Daluvoy MB, Fekrat S (2021) Clinical characteristics and visual outcomes in endophthalmitis after keratoprosthesis implantation. Retina. https://doi.org/10.1097/IAE.0000000000003300
Bostan C, Nayman T, Szigiato AA, Morfeq H, Harissi-Dagher M (2021) Endophthalmitis in eyes with the Boston type i keratoprosthesis: incidence, recurrence, risk factors, and outcomes. Cornea 40:1258–1266. https://doi.org/10.1097/ICO.0000000000002641
Khair D, Salimi A, Harissi-Dagher M (2021) Vitreoretinal complications in Boston keratoprosthesis type 1. Am J Ophthalmol 231:101–108. https://doi.org/10.1016/j.ajo.2021.06.002
Chhablani J, Panchal B, Das T, Pathegay A, Motukupally SR, Pappuru RR, Basu S, Sangwan V (2015) Endophthalmitis in Boston keratoprosthesis: case series and review of literature. Int Ophthalmol 35:673–678. https://doi.org/10.1007/s10792-014-9994-9
Nonpassopon M, Niparugs M, Cortina MS (2020) Boston type 1 keratoprosthesis: updated perspectives. Clin Ophthalmol 14:1189–1200. https://doi.org/10.2147/OPTH.S219270
Liu J, Harissi-Dagher M (2021) Comparison of outcomes in patients with and without soft contact lens wear following Boston keratoprosthesis type 1. Can J Ophthalmol. https://doi.org/10.1016/j.jcjo.2021.04.017
Akpek EK, Cassard SD, Dunlap K, Hahn S, Ramulu PY (2015) Donor corneal transplantation vs Boston type 1 keratoprosthesis in patients with previous graft failures: a retrospective single center study (An American Ophthalmological Society Thesis). Trans Am Ophthalmol Soc 113:T3
Davila JR, Mian SI (2016) Infectious keratitis after keratoplasty. Curr Opin Ophthalmol 27:358–366. https://doi.org/10.1097/ICU.0000000000000269
Chen JY, Jones MN, Srinivasan S, Neal TJ, Armitage WJ, Kaye SB, Group NOTA, Contributing O (2015) endophthalmitis after penetrating keratoplasty. Ophthalmology 122:25–30. https://doi.org/10.1016/j.ophtha.2014.07.038
Soong HK, Schwartz AE, Meyer RF, Sugar A (1989) Penetrating keratoplasty for corneal scarring due to herpes zoster ophthalmicus. Br J Ophthalmol 73:19–21. https://doi.org/10.1136/bjo.73.1.19
Daoud R, Sabeti S, Harissi-Dagher M (2020) Management of corneal melt in patients with Boston keratoprosthesis type 1: repair versus repeat. Ocul Surf 18:713–717. https://doi.org/10.1016/j.jtos.2020.07.005
Harissi-Dagher M, Khan BF, Schaumberg DA, Dohlman CH (2007) Importance of nutrition to corneal grafts when used as a carrier of the Boston keratoprosthesis. Cornea 26:564–568. https://doi.org/10.1097/ICO.0b013e318041f0a6
Jardeleza MS, Rheaume MA, Chodosh J, Lane AM, Dohlman CH (2015) Retinal detachments after Boston keratoprosthesis: incidence, predisposing factors, and visual outcomes. Digit J Ophthalmol 21:1–15. https://doi.org/10.5693/djo.01.2015.10.001
Modjtahedi BS, Eliott D (2014) Vitreoretinal complications of the Boston keratoprosthesis. Semin Ophthalmol 29:338–348. https://doi.org/10.3109/08820538.2014.959204
Park J, Phrueksaudomchai P, Cortina MS (2020) Retroprosthetic membrane: a complication of keratoprosthesis with broad consequences. Ocul Surf 18:893–900. https://doi.org/10.1016/j.jtos.2020.09.004
Somavilla C, Karas FI, Cortina MS (2019) Association between retroprosthetic membrane formation and post-operative angle closure after Boston type 1 keratoprosthesis surgery. Invest Ophthalmol Vis Sci 60:6319–6319
Dokey A, Ramulu PY, Utine CA, Tzu JH, Eberhart CG, Shan S, Gelhbach PL, Akpek EK (2012) Chronic hypotony associated with the Boston type 1 keratoprosthesis. Am J Ophthalmol 154(266–271):e261. https://doi.org/10.1016/j.ajo.2012.03.001
Sivaraman KR, Hou JH, Allemann N, de la Cruz J, Cortina MS (2013) Retroprosthetic membrane and risk of sterile keratolysis in patients with type I Boston keratoprosthesis. Am J Ophthalmol 155:814–822. https://doi.org/10.1016/j.ajo.2012.11.019
Rudnisky CJ, Belin MW, Todani A, Al-Arfaj K, Ament JD, Zerbe BJ, Ciolino JB, Boston Type 1 Keratoprosthesis Study G (2012) Risk factors for the development of retroprosthetic membranes with Boston keratoprosthesis type 1: multicenter study results. Ophthalmology 119:951–955. https://doi.org/10.1016/j.ophtha.2011.11.030
Utine CA, Tzu J, Dunlap K, Akpek EK (2011) Visual and clinical outcomes of explantation versus preservation of the intraocular lens during keratoprosthesis implantation. J Cataract Refract Surg 37:1615–1622. https://doi.org/10.1016/j.jcrs.2011.03.045
Bonnet C, Chehaibou I, Chen A, Bourges JL, Markovic D, Hubschman JP, Aldave AJ (2021) Postoperative posterior segment complications after Boston type 1 keratoprosthesis: incidence, risk factors, and intermediate-term outcomes. Retina. https://doi.org/10.1097/IAE.0000000000003233
Ho Wang Yin G, Hoffart L (2017) Post-keratoplasty astigmatism management by relaxing incisions: a systematic review. Eye Vis (Lond) 4:29. https://doi.org/10.1186/s40662-017-0093-7
Touma S, Harissi-Dagher M (2021) Outcomes and complications of Boston keratoprosthesis type I implantation in unilateral versus bilateral corneal blindness. Can J Ophthalmol 56:130–136. https://doi.org/10.1016/j.jcjo.2020.08.011
Sabeti S, Daoud R, Robert MC, Harissi-Dagher M (2021) Frozen versus fresh corneal graft carriers in Boston keratoprosthesis surgery: 10-year outcomes. Can J Ophthalmol. https://doi.org/10.1016/j.jcjo.2021.02.033
Ament JD, Stryjewski TP, Ciolino JB, Todani A, Chodosh J, Dohlman CH (2010) Cost-effectiveness of the Boston keratoprosthesis. Am J Ophthalmol 149(221–228):e222. https://doi.org/10.1016/j.ajo.2009.08.027
Canadian Agency for Drugs and Technologies in Healt (2016) Boston keratoprosthesis for the treatment of corneal blindness: clinical effectiveness and cost-effectiveness. Canadian Agency for Drugs and Technologies in Health. https://www.ncbi.nlm.nih.gov/books/NBK362173/. Accessed 18 Nov 2021
Author information
Authors and Affiliations
Contributions
SB performed literature research and manuscript redaction. MT and YY assisted SB in literature research and provided clinical insights, and they helped with manuscript redaction. MHD is the PI of this review and the principal supervisor of SB, MT, and YY. MHD also provided clinical insights and helped with manuscript redaction. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Competing interests
M. Harissi-Dagher and C. Maya Tong are advisors for Dompe regarding cenegermin in the treatment of neurotrophic keratitis.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bonneau, S., Tong, C.M., Yang, Y. et al. The treatment of end-stage corneal disease: penetrating keratoplasty compared with Boston type 1 keratoprosthesis. Graefes Arch Clin Exp Ophthalmol 260, 2781–2790 (2022). https://doi.org/10.1007/s00417-022-05646-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05646-1