Abstract
Purpose
Ocular discomfort is a common symptom in central sensitization syndromes. The aim of this study was to evaluate ocular surface discomfort and related corneal changes in patients with irritable bowel syndrome.
Methods
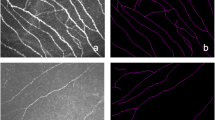
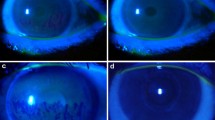
Twenty-nine patients with IBS (20 female, 9 male, mean age: 45.3 ± 10.1 years) and 37 healthy control subjects (25 female, 12 male, mean age: 44.95 ± 9.76 years) were included. A detailed ophthalmological examination was performed to all participants including tear break-up time (TBUT) and Schirmer test I with anesthetic (SIT). Ocular discomfort was evaluated using the ocular surface disease index (OSDI) questionnaire and corneal sensation was evaluated with Cochet-Bonnet esthesiometer. Corneal subbasal nerve plexus was evaluated with in vivo corneal confocal microscopy (IVCM).
Results
There was no significant difference between the groups for age, gender distribution, and visual acuity. OSDI scores were significantly higher (p = 0.008) and TBUT was significantly reduced in patients with IBS compared to controls (p = 0.001 for right eye, p = 0.014 for left eye). However, there was no significant difference in corneal touch sensation and SIT results between the groups. IVCM revealed that corneal nerve fiber density, corneal nerve branch density, and corneal nerve fiber length were significantly reduced in patients with IBS (p < 0.001, p < 0.001, and p = 0.023, respectively).
Conclusion
Patients with IBS have increased dry eye-associated ocular surface complaints and nerve fiber loss in corneal subbasal nerve plexus. IBS should be remembered in the differential diagnosis, when there is discordance between the level of ocular surface discomfort and dry eye disease associated corneal findings.



Similar content being viewed by others
Data availability
The data is available from the corresponding author upon reasonable request.
References
Sayegh RR, Yu Y, Farrar JT, Kuklinski EJ, Shtein RM, Asbell PA, Maguire MG, Dry Eye A, Management Study Research G (2020) Ocular discomfort and quality of life among patients in the dry eye assessment and management study. Cornea.https://doi.org/10.1097/ICO.0000000000002580
Erkan Turan K, Kocabeyoglu S, Unal-Cevik I, Bezci F, Akinci A, Irkec M (2018) Ocular surface alterations in the context of corneal in vivo confocal microscopic characteristics in patients with fibromyalgia. Cornea 37:205–210. https://doi.org/10.1097/ICO.0000000000001447
Asproudis I, Tsoumani AT, Katsanos KH, Katsanos AH, Theopistos V, Paschidis KA, Tsianos EV, Christodoulou D (2016) Irritable bowel syndrome might be associated with dry eye disease. Ann Gastroenterol 29:487–491
Aykut V, Elbay A, Çigdem Uçar I, Esen F, Durmus A, Karadag R, Oguz H (2018) Corneal sensitivity and subjective complaints of ocular pain in patients with fibromyalgia. Eye (Lond) 32:763–767. https://doi.org/10.1038/eye.2017.275
Aykut V, Elbay A, Esen F, Kocaman G, Savran Elibol E, Oguz H (2018) Patterns of altered corneal sensation in patients with chronic migraine. Eye Contact Lens 44(Suppl 2):S400–S403. https://doi.org/10.1097/ICL.0000000000000553
Farhangi M, Diel RJ, Buse DC, Huang AM, Levitt RC, Sarantopoulos CD, Felix ER, Galor A (2020) Individuals with migraine have a different dry eye symptom profile than individuals without migraine. Br J Ophthalmol 104:260–264. https://doi.org/10.1136/bjophthalmol-2018-313471
Rosenthal P, Baran I, Jacobs DS (2009) Corneal pain without stain: is it real? Ocul Surf 7:28–40. https://doi.org/10.1016/s1542-0124(12)70290-2
Vehof J, Zavos HM, Lachance G, Hammond CJ, Williams FM (2014) Shared genetic factors underlie chronic pain syndromes. Pain 155:1562–1568. https://doi.org/10.1016/j.pain.2014.05.002
Kindler LL, Bennett RM, Jones KD (2011) Central sensitivity syndromes: mounting pathophysiologic evidence to link fibromyalgia with other common chronic pain disorders. Pain Manag Nurs 12:15–24. https://doi.org/10.1016/j.pmn.2009.10.003
Spierer O, Felix ER, McClellan AL, Parel JM, Gonzalez A, Feuer WJ, Sarantopoulos CD, Levitt RC, Ehrmann K, Galor A (2016) Corneal mechanical thresholds negatively associate with dry eye and ocular pain symptoms. Invest Ophthalmol Vis Sci 57:617–625. https://doi.org/10.1167/iovs.15-18133
Neblett R, Cohen H, Choi Y, Hartzell MM, Williams M, Mayer TG, Gatchel RJ (2013) The Central Sensitization Inventory (CSI): establishing clinically significant values for identifying central sensitivity syndromes in an outpatient chronic pain sample. J Pain 14:438–445. https://doi.org/10.1016/j.jpain.2012.11.012
Vehof J, Sillevis Smitt-Kamminga N, Kozareva D, Nibourg SA, Hammond CJ (2016) Clinical characteristics of dry eye patients with chronic pain syndromes. Am J Ophthalmol 162(59–65):e52. https://doi.org/10.1016/j.ajo.2015.11.017
Longstreth GF (2005) Definition and classification of irritable bowel syndrome: current consensus and controversies. Gastroenterol Clin North Am 34:173–187. https://doi.org/10.1016/j.gtc.2005.02.011
Saito YA, Schoenfeld P, Locke GR 3rd (2002) The epidemiology of irritable bowel syndrome in North America: a systematic review. Am J Gastroenterol 97:1910–1915. https://doi.org/10.1111/j.1572-0241.2002.05913.x
Gwee KA (2005) Irritable bowel syndrome in developing countries–a disorder of civilization or colonization? Neurogastroenterol Motil 17:317–324. https://doi.org/10.1111/j.1365-2982.2005.00627.x
Holtmann GJ, Ford AC, Talley NJ (2016) Pathophysiology of irritable bowel syndrome. Lancet Gastroenterol Hepatol 1:133–146. https://doi.org/10.1016/s2468-1253(16)30023-1
Ballou SK, Keefer L (2013) Multicultural considerations in the diagnosis and management of irritable bowel syndrome: a selective summary. Eur J Gastroenterol Hepatol 25:1127–1133. https://doi.org/10.1097/MEG.0b013e3283632bf2
Simren M, Palsson OS, Whitehead WE (2017) Update on Rome IV criteria for colorectal disorders: implications for clinical practice. Curr Gastroenterol Rep 19:15. https://doi.org/10.1007/s11894-017-0554-0
Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL (2000) Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol 118:615–621. https://doi.org/10.1001/archopht.118.5.615
Dabbah MA, Graham J, Petropoulos IN, Tavakoli M, Malik RA (2011) Automatic analysis of diabetic peripheral neuropathy using multi-scale quantitative morphology of nerve fibres in corneal confocal microscopy imaging. Med Image Anal 15:738–747. https://doi.org/10.1016/j.media.2011.05.016
Shetty R, Deshmukh R, Shroff R, Dedhiya C, Jayadev C (2018) Subbasal Nerve plexus changes in chronic migraine. Cornea 37:72–75. https://doi.org/10.1097/ICO.0000000000001403
Galor A, Felix ER, Feuer W, Shalabi N, Martin ER, Margolis TP, Sarantopoulos CD, Levitt RC (2015) Dry eye symptoms align more closely to non-ocular conditions than to tear film parameters. Br J Ophthalmol 99:1126–1129. https://doi.org/10.1136/bjophthalmol-2014-306481
Belmonte C, Nichols JJ, Cox SM, Brock JA, Begley CG, Bereiter DA, Dartt DA, Galor A, Hamrah P, Ivanusic JJ, Jacobs DS, McNamara NA, Rosenblatt MI, Stapleton F, Wolffsohn JS (2017) TFOS DEWS II pain and sensation report. Ocul Surf 15:404–437. https://doi.org/10.1016/j.jtos.2017.05.002
Hoeijmakers JG, Faber CG, Lauria G, Merkies IS, Waxman SG (2012) Small-fibre neuropathies–advances in diagnosis, pathophysiology and management. Nat Rev Neurol 8:369–379. https://doi.org/10.1038/nrneurol.2012.97
Kinard KI, Smith AG, Singleton JR, Lessard MK, Katz BJ, Warner JE, Crum AV, Mifflin MD, Brennan KC, Digre KB (2015) Chronic migraine is associated with reduced corneal nerve fiber density and symptoms of dry eye. Headache 55:543–549. https://doi.org/10.1111/head.12547
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Istanbul Medeniyet University Goztepe Education and Research Hospital Ethics Committee (document no: 2018/0056).
Consent to participate
Written informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Uçar, I.Ç., Esen, F., Turhan, S.A. et al. Corneal neuropathic pain in irritable bowel syndrome: clinical findings and in vivo corneal confocal microscopy. Graefes Arch Clin Exp Ophthalmol 259, 3011–3017 (2021). https://doi.org/10.1007/s00417-021-05269-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05269-y