Abstract
Purpose
To evaluate the efficacy of intraoperative slow-release dexamethasone implant (DEX) combined with removal of idiopathic epiretinal membrane (ERM).
Methods
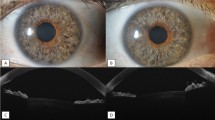
In this observational retrospective study, data of 40 patients with phakic eyes affected by idiopathic ERM were analysed. All patients underwent cataract phacoemulsification, 25-gauge (G) pars plana vitrectomy (PPV), ERM removal with DEX implant (“DEX YES” group, #20) or without DEX implant (“DEX NO” group, #20). We collected data on best-corrected visual acuity (BCVA) < 20/40 Snellen charts, central macular thickness (CMT) ≤ 400 μm (measured by SD-OCT) and integrity of sub-foveal ellipsoid/myoid zone. BCVA, CMT and intraocular pressure (IOP) were evaluated at baseline as well as 15, 30 and 90 days after surgery.
Results
In the “DEX YES” group, statistically significant BCVA improvement was observed at 15, 30 and 90 days (p < 0.001), while in the “DEX NO” group, improvements were observed only at 30 and 90 days (p < 0.001). In both groups, CMT significantly decreased at each follow-up visit (p < 0.001), and no statistically significant increase of IOP was detected at each follow-up visit.
Conclusions
In this study, DEX accelerated the improvement of BCVA at 15 days after surgery. However, no evidence of further anatomical (CMT) and functional (BCVA) DEX effectiveness combined with removal of idiopathic ERM by 25-G PPV at 30 and 90 days follow-up was observed.


Similar content being viewed by others
References
Joshi M, Agrawal S, Christoforidis JB (2013) Inflammatory mechanisms of idiopathic epiretinal membrane formation. Mediat Inflamm 192582. https://doi.org/10.1155/2013/192582
Cheung N, Tan SP, Lee SY, Cheung GCM, Tan G, Kumar N et al (2017) Prevalence and risk factors for epiretinal membrane: the Singapore Epidemiology of Eye Disease study. Br J Ophthalmol 101:371–376. https://doi.org/10.1136/bjophthalmol-2016-308563
Iwanoff A (1865) Beiträge zur normalen und pathologischen anatomie des auges. Graefes Arch Clin Exp Ophthalmol 11:135
Koizumi H, Spaide RF, Fisher YL, Freund KB, Klancnik JM Jr, Yannuzzi LA (2008) Three-dimensional evaluation of vitreomacular traction and epiretinal membrane using spectral-domain optical coherence tomography. Am J Ophthalmol 145:509–517. https://doi.org/10.1016/j.ajo.2007.10.014
Gass JDM (1997) Macular dysfunction caused by epiretinal membrane contraction. In: Stereoscopic Atlas of Macular Diseases: Diagnosis and Treatment, vol 2, 4th edn. Mosby, St Louis, pp 938–590
Stevenson W, Prospero Ponce C, Agarwal D, Gelman R, Christoforidis J (2016) Epiretinal membrane: optical coherence tomography-based diagnosis and classification. Clin Ophthalmol 10:527–534. https://doi.org/10.2147/OPTH.S97722
Duker JS, Kaiser PK, Binder S et al (2013) The international vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120:2611–2619. https://doi.org/10.1016/j.ophtha.2013.07.042
Kritzenberg M, Jungas B, Framme C, Helbig H, Gabel VP, Fuchshofer R et al (2011) Different collagen types define two types of idiopathic epiretinal membranes. Histopathology 58:953–965. https://doi.org/10.1111/j.1365-2559.2011.03820
Kampik A (2012) Pathology of epiretinal membrane, idiopathic macular hole, and vitreomacular traction syndrome. Retina 32(Suppl 2):S194–S198;discussion S198–9. https://doi.org/10.1097/IAE.0b013e31825bc20a
Sebag J, Gupta P, Rosen RR et al (2007) Macular holes and macular pucker: the role of vitreoschisis as imaged by optical coherence tomography/scanning laser ophthalmoscopy. Trans Am Ophthalmol Soc 105:121–129
Romano MR, Comune C, Ferrara M, Cennamo G, De Cillà S, Toto L et al (2015) Retinal changes induced by epiretinal tangential forces. J Ophthalmol 2015:372564. https://doi.org/10.1155/2015/372564
Miyazaki M, Nakamura H, Kubo M, Kiyohara Y, Iida M, Ishibashi T et al (2003) Prevalence and risk factors for epiretinal membranes in a Japanese population: the Hisayama study. Graefes Arch Clin Exp Ophthalmol 241:642–646. https://doi.org/10.1007/s00417-003-0723-8
Katira RC, Zamani M, Berinstein DM, Garfinkel RA (2008) Incidence and characteristics of macular pucker formation after primary retinal detachment repair by pars plana vitrectomy alone. Retina 28:744–748. https://doi.org/10.1097/IAE
Bu S, Kuijer R, Li X, Hooymans J, Los L (2014) Idiopathic epiretinal membrane. Retina 34:2317–2335. https://doi.org/10.1097/IAE.0000000000000349
Suh MH, Seo JM, Park KH, Yu HG (2009) Associations between macular findings by optical coherence tomography and visual outcomes after epiretinal membrane removal. Am J Ophthalmol 147:473–480. https://doi.org/10.1016/j.ajo.2008.09.020
Miguel AI, Legris A (2017) Prognostic factors of epiretinal membranes: a systematic review. J Fr Ophtalmol 40:61–79. https://doi.org/10.1016/j.jfo.2016.12.001
Carpentier C, Zanolli M, Wu L et al (2013) Residual internal limiting membrane after epiretinal membrane peeling: results of the pan-American collaborative retina study group. Retina 33:2026–2031. https://doi.org/10.1097/IAE.0b013e31828e69c2
Ripandelli G, Scarinci F, Piaggi P et al (2015) Macular pucker: to peel or not to peel the internal limiting membrane? A microperimetric response. Retina 35:498–507. https://doi.org/10.1097/IAE.0000000000000330
Boyer D, Yoon Y, Belfort R, Bandello F, Ozurdex MEAD Study Group et al (2014) Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology 121:1904–1914. https://doi.org/10.1016/j.ophtha.2014.04.024
Massa H, Georgoudis P, Panos G (2019) Dexamethasone intravitreal implant (OZURDEX®) for macular edema secondary to noninfectious uveitis: a review of the literature. Ther Deliv 10:343–351. https://doi.org/10.4155/tde-2019-0024
Chang Y, Liu P, Kao T, Wu H et al (2018) Dexamethasone intravitreal implant (Ozurdex) for long-term macular edema after epiretinal membrane peeling surgery. Ophthalmol 2018:5832186. https://doi.org/10.1155/2018/5832186
Furino C, Boscia F, Recchimurzo N, Sborgia C, Alessio G (2014) Intravitreal dexamethasone implant for refractory macular edema secondary to vitrectomy for macular pucker. Retina 34:1612–1616. https://doi.org/10.1097/IAE.0000000000000105
Rizzo S, Pacini B, De Angelis L, Barca F et al (2020) Intrascleral hydration for 23-gauge pars plana vitrectomy sclerotomy closure. Retina. https://doi.org/10.1097/IAE.0000000000002703
Chang-Lin E, Burke JA, Peng Q et al (2011) Pharmacokinetics of a sustained-release dexamethasone intravitreal implant in vitrectomized and nonvitrectomized eyes. Invest Ophthalmol Vis Sci 52:4605–4609. https://doi.org/10.1167/iovs.10-6387
Hattenbach L, Springer-Wanner C, Hoerauf H, Callizo J et al (2017) Intravitreal sustained-release steroid implants for the treatment of macular edema following surgical removal of epiretinal membranes. Ophthalmologica 237:232–237. https://doi.org/10.1159/000464259
Chatziralli I, Dimitriou E, Theodossiadis G, Chatzirallis A, Kazantzis D, Theodossiadis P (2019) Treatment of macular edema after pars plana vitrectomy for idiopathic epiretinal membrane using intravitreal dexamethasone implant: long-term outcomes. Ophthalmologica 242:16–21. https://doi.org/10.1159/000496705
Taney LS, Baumal CR, Duker JS (2015) Sustained-release dexamethasone intravitreal implant for persistent macular edema after vitrectomy for epiretinal membrane. Ophthalmic Surg Lasers Imaging Retina 46:224–228. https://doi.org/10.3928/23258160-20150213-01
Guidi G, Casini G, Ripandelli G, Piaggi P et al (2018) Intraretinal edema after 25-gauge vitrectomy and macular pucker removal: is intraoperative sustained-release dexamethasone a real treatment option? Retina 38:993–999. https://doi.org/10.1097/IAE.0000000000001627
Iovino C, Giannaccare G, Pellegrini M, Bernabei F (2019) Efficacy and safety of combined vitrectomy with intravitreal dexamethasone implant for advanced stage epiretinal membrane. Drug Des Devel Ther 13:4107–4114. https://doi.org/10.2147/DDDT.S229031
Giansanti F, Bitossi A, Giacomelli G, Virgili G et al (2013) Evaluation of macular thickness after uncomplicated cataract surgery using optical coherence tomography. Eur J Ophthalmol 23:751–756. https://doi.org/10.5301/ejo.5000280
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Azienda Ospedaliero Universitaria Careggi, Florence, Italy, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Savastano, A., Bitossi, A., Giansanti, F. et al. Evaluation of intraoperative slow-release dexamethasone implant combined with idiopathic epiretinal membrane removal. Graefes Arch Clin Exp Ophthalmol 259, 379–385 (2021). https://doi.org/10.1007/s00417-020-04911-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04911-5