Abstract
Purpose
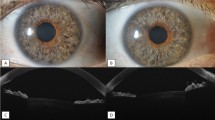
Our purpose was to investigate the impact of lens status of corneal donors on the two-year course and clinical outcome of Descemet membrane endothelial keratoplasty (DMEK).
Methods
In 181 DMEK surgeries, 136 phakic and 45 pseudophakic donor corneas were grafted. In this retrospective audit we compared the lens status of corneal donors regarding the outcome measures best spectacle-corrected visual acuity (BSCVA), central corneal thickness (CCT), and endothelial cell density (ECD) at 1, 3, 6, 12, and 24 months, as well as intra- and postoperative complication rates and graft detachment rates requiring re-bubbling.
Results
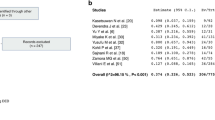
Comparing the use of phakic and pseudophakic donor tissue in DMEK surgery, BSCVA results revealed no significant differences during the two-year course (p ≥ 0.087). CCT showed significantly lower values at 1 month (553.8 ± 56 vs. 625.2 ± 119 μm; p < 0.001) and 6 months follow-up (530.6 ± 49.9 vs. 557.3 ± 47 μm; p = 0.026) for phakic donor tissue recipients, but were comparable later (p ≥ 0.173). ECD values were statistically higher 6 (1915 ± 390 vs. 1565 ± 420 cells/mm2; p < 0.001) and 24 months postoperatively (1772 ± 384 vs. 1375 ± 377 cells/mm2; p = 0.030) in phakic donor tissue recipients. Mixed regression analyses demonstrated a significant association between ECD results and donor lens status (p = 0.029) and donor ECD (p = 0.028), but donor age did not show significant influence (p = 0.241).
Conclusion
ECD is higher in phakic corneal donors and appears to remain at a higher level during the course resulting in initially faster reduction of corneal edema compared to pseudophakic DMEK grafts. Nevertheless, pseudophakic transplants with high ECD seem to produce comparable functional results in recipients after a two year course.

Similar content being viewed by others
References
Melles GR, Ong TS, Ververs B, der WJ V (2006) Descemet membrane endothelial keratoplasty (DMEK). Cornea 25:987–990
Melles GR (2006) Posterior lamellar keratoplasty: DLEK to DSEK to DMEK. Cornea. 25:879–881
Maier P, Reinhard T, Cursiefen C (2013) Descemet stripping endothelial keratoplasty--rapid recovery of visual acuity. Dtsch Arztebl Int. 110:365–371
Cursiefen C (2013) Descemet membrane endothelial keratoplasty: the taming of the shrew. JAMA Ophthalmol. 131:88–89
Schaub F, Enders P, Zachewicz J, Heindl LM, Stanzel TP, Cursiefen C, Bachmann BO (2016) Impact of Donor Age on Descemet Membrane Endothelial Keratoplasty Outcome: Evaluation of Donors Aged 17-55 Years. Am J Ophthalmol. 170:119–127
Gorovoy IR, Cui QN, Gorovoy MS (2014) Donor tissue characteristics in preparation of DMEK grafts. Cornea 33:683–685
Weller JM, Tourtas T, Kruse FE, Schlotzer-Schrehardt U, Fuchsluger T, Bachmann BO (2015) Descemet membrane endothelial keratoplasty as treatment for graft failure after descemet stripping automated endothelial keratoplasty. Am J Ophthalmol. 159:1050–1057
Heindl LM, Riss S, Bachmann BO, Laaser K, Kruse FE, Cursiefen C (2011) Split cornea transplantation for 2 recipients: a new strategy to reduce corneal tissue cost and shortage. Ophthalmology. 118:294–301
Maier AK, Gundlach E, Schroeter J, Klamann MK, Gonnermann J, Riechardt AI, Bertelmann E, Joussen AM, Torun N (2015) Influence of the difficulty of graft unfolding and attachment on the outcome in Descemet membrane endothelial keratoplasty. Graefes Arch Clin Exp Ophthalmol. 253:895–900
Kruse FE, Schrehardt US, Tourtas T (2014) Optimizing outcomes with Descemet's membrane endothelial keratoplasty. Curr Opin Ophthalmol. 25:325–334
Steven P, Le Blanc C, Velten K, Lankenau E, Krug M, Oelckers S, Heindl LM, Gehlsen U, Huttmann G, Cursiefen C (2013) Optimizing descemet membrane endothelial keratoplasty using intraoperative optical coherence tomography. JAMA Ophthalmol. 131:1135–1142
Kruse FE, Laaser K, Cursiefen C, Heindl LM, Schlotzer-Schrehardt U, Riss S, Bachmann BO (2011) A stepwise approach to donor preparation and insertion increases safety and outcome of Descemet membrane endothelial keratoplasty. Cornea. 30:580–587
Heindl LM, Bucher F, Caramoy A, Hos D, Matthaei M, Cursiefen C (2014) Safety of donor tissue preparation and use of descemetoschisis and torn tissue in descemet membrane endothelial keratoplasty. Cornea. 33:e7–e9
Heinzelmann S, Huther S, Bohringer D, Eberwein P, Reinhard T, Maier P (2014) Influence of donor characteristics on descemet membrane endothelial keratoplasty. Cornea. 33:644–648
Rodriguez-Calvo de Mora M, Groeneveld-van Beek EA, Frank LE, Van der WJ OS, Bruinsma M, Melles GR (2016) Association Between Graft Storage Time and Donor Age With Endothelial Cell Density and Graft Adherence After Descemet Membrane Endothelial Keratoplasty. JAMA Ophthalmol. 134:91–94
Ang M, Wilkins MR, Mehta JS, Tan D (2016) Descemet membrane endothelial keratoplasty. Br J Ophthalmol. 100:15–21
Guerra FP, Anshu A, Price MO, Giebel AW, Price FW (2011) Descemet’s membrane endothelial keratoplasty: prospective study of 1-year visual outcomes, graft survival, and endothelial cell loss. Ophthalmology. 118:2368–2373
Melles GR, Ong TS, Ververs B, der WJ V (2008) Preliminary clinical results of Descemet membrane endothelial keratoplasty. Am J Ophthalmol. 145:222–227
Price MO, Giebel AW, Fairchild KM, Price FW Jr (2009) Descemet's membrane endothelial keratoplasty: prospective multicenter study of visual and refractive outcomes and endothelial survival. Ophthalmology. 116:2361–2368
Schaub F, Enders P, Snijders K, Schrittenlocher S, Siebelmann S, Heindl LM, Bachmann BO, Cursiefen C (2017) One-year outcome after Descemet membrane endothelial keratoplasty (DMEK) comparing sulfur hexafluoride (SF6) 20% versus 100% air for anterior chamber tamponade. Br J Ophthalmol. 101:902–908
Sales CS, Terry MA, Veldman PB, Mayko ZM, Straiko MD (2016) Relationship Between Tissue Unscrolling Time and Endothelial Cell Loss. Cornea. 35:471–476
Funding
This research was supported by German Research Foundation FOR 2240 “(Lymph) Angiogenesis And Cellular Immunity In Inflammatory Diseases Of The Eye” to CC and LMH (www.for2240.de) and EU COST BM 1302 “Joining Forces in Corneal Regeneration” to BOB and CC (www.biocornea.eu). The sponsor had no role in the design or implementation of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Schaub, F., Pohl, L., Enders, P. et al. Impact of corneal donor lens status on two-year course and outcome of Descemet membrane endothelial keratoplasty (DMEK). Graefes Arch Clin Exp Ophthalmol 255, 2407–2414 (2017). https://doi.org/10.1007/s00417-017-3827-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3827-2