Abstract
Introduction
The purpose of this study was to describe the anatomical and functional outcome of vascular endothelial growth factor inhibitor (anti-VEGF) treatment in symptomatic peripheral exudative hemorrhagic chorioretinopathy (PEHCR) involving the macula.
Methods
Clinical records from patients seen between 2012 and 2013 at a single academic center were reviewed to identify PEHCR patients receiving anti-VEGF therapy due to disease-associated changes involving the macula. Affected eyes were either treated with consecutive intravitreal injections of anti-VEGF or vitrectomy combined with anti-VEGF followed by pro re nata injections.
Results
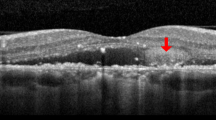
The mean age of the patients was 76 years (range 70–89 years). In all nine eyes, visual acuity was reduced due to central subretinal fluid. On average, three anti-VEGF injections (range 2–5 injections) were required initially to achieve complete resolution of macular subretinal fluid. In three eyes, subretinal fluid reappeared after an average of 10 months (range 5–16 months), and an average of 2.5 anti-VEGF injections (range 2–3 injections) were necessary to attain complete resolution of macular subretinal fluid a second time. Median visual acuity at the visit before the first injection was 1.0 logMAR (range 2.1-0.4 logMAR) and increased to 0.8 logMAR (range 2-0.1 logMAR) at the last visit.
Conclusion
Results of this study show that for cases in which PEHCR becomes symptomatic due to macular involvement, anti-VEGF treatment may have drying potential. Although vision was improved in some patients, it remained limited in cases with long-term macular involvement, precluding any definitive functional conclusion. However, we believe that the use of anti-VEGF agents should be recommended in PEHCR that threatens the macula. Due to its often self-limiting course, peripheral lesions should be closely observed. Larger studies are needed in order to provide clear evidence of the efficacy of anti-VEGF therapy in PEHCR.

Similar content being viewed by others
References
Annesley WH Jr (1980) Peripheral exudative hemorrhagic chorioretinopathy. Trans Am Ophthalmol Soc 78:321–364
Shields JA, Mashayekhi A, Ra S, Shields CL (2005) Pseudomelanomas of the posterior uveal tract: the 2006 Taylor R Smith Lecture. Retina 25:767–771
Shields CL, Salazar P, Mashayekhi A et al (2009) Peripheral exudative hemorrhagic chorioretinopathy (PEHCR) simulating choroidal melanoma in 173 eyes. Ophthalmology 116:529–535
Barkmeier AJ, Kadikoy H, Holz ER et al (2011) Regression of serous macular detachment due to peripheral exudative hemorrhagic chorioretinopathy following intravitreal bevacizumab. Eur J Ophthalmol 21(4):506–508
Pinarci EY, Kilic I, Bayar SA et al (2013) Clinical characteristics of peripheral exudative hemorrhagic chorioretinopathy and its response to bevacizumab therapy. Eye (Lond) 27(1):111–112
Mantel I, Uffer S, Zografos L (2009) Peripheral exudative hemorrhagic chorioretinopathy: a clinical, angiographic, and histologic study. Am J Ophthalmol 148(6):932–938
Goldman DR, Freund KB, McCannel CA et al (2013) Peripheral polypoidal choroidal vasculopathy as a cause of peripheral exudative hemorrhagic chorioretinopathy: a report of 10 eyes. Retina 33(1):48–55
Bach M, Guntram K (1998) Sehschärfenbestimmung nach europäischer Norm: wissenschaftliche Grundlagen und Möglichkeiten der automatischen Messung. KlinMonbl Augenheilkunde 212(4):190–195
Agarwal A (2012) Gass’ atlas of macular diseases fifth edition, Elsevier, 1(3):122
Mirshahi A, Höhn F, Baatz H et al (2009) Peripheral exudative haemorrhagic chorioretinopathy: clinical and angiographic findings. Klin Monbl Augenheilkd 226(8):659–663
Xu Y, You Y, Du W et al (2012) Ocular pharmacokinetics of bevacizumab in vitrectomized eyes with silicone oil tamponade. Invest Ophthalmol Vis Sci 53(9):5221–5226
Falavarjani KG, Modarres M, Nazari H (2010) Therapeutic effect of bevacizumab injected into the silicone oil in eyes with neovascular glaucoma after vitrectomy for advanced diabetic retinopathy. Eye (Lond) 24(4):717–719
Manzano RP, Peyman GA, Khan P et al (2006) Testing intravitreal toxicity of bevacizumab (Avastin). Retina 26:257–261
Mantel I, Schalenbourg A, Zografos L (2012) Peripheral exudative hemorrhagic chorioretinopathy: polypoidal choroidal vasculopathy and hemodynamic modifications. Am J Ophthalmol 153(5):910–922
Mashayekhi A, Shields CL, Shields JA (2013) Peripheral exudative hemorrhagic chorioretinopathy: a variant of polypoidal choroidal vasculopathy? J Ophthalmic Vis Res 8(3):264–267
Tong JP, Chan WM, Liu DT et al (2006) Aqueous humor levels of vascular endothelial growth factor and pigment epithelium derived factor in polypoidal choroidal vasculopathy and choroidal neovascularization. Am J Ophthalmol 141:456–462
Matsuoka M, Ogata N, Otsuji T et al (2004) Expression of pigment epithelium derived factor and vascular endothelial growth factor in choroidal neovascular membranes and polypoidal choroidal vasculopathy. Br J Ophthalmol 88:809–815
Acknowledgments
Statistical analysis was performed by Dr. Ulrich Gauger, medical statistician.
Conflict of interest
M. Rehak: payment for lectures including service on speakers bureaus, payment for manuscript preparation, travel/accommodations/meeting expenses. A.M. Joussen: payment for development of educational presentations and travel/accommodations/meeting expenses. All other authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements). All authors have non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seibel, I., Hager, A., Duncker, T. et al. Anti-VEGF therapy in symptomatic peripheral exudative hemorrhagic chorioretinopathy (PEHCR) involving the macula. Graefes Arch Clin Exp Ophthalmol 254, 653–659 (2016). https://doi.org/10.1007/s00417-015-3096-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3096-x