Abstract
Purpose
To examine and quantify any change in the dark adaptation (DA) function of normal subjects due to learning effect on test–retest.
Methods
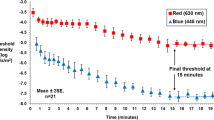
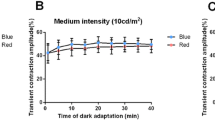
Sixteen normal subjects (12 women, four men) whose ages ranged between 24 and 52 years (mean 34.6 ± 6.7 years) were studied. The interval period between test and retest ranged between 0.92 and 2.37 months (mean 1.38 ± 0.40 months). DA was measured with a Goldmann–Weekers (GW) dark adaptometer, and subjects were pre-adapted using a light intensity of 2,700 cd/m2 Ganzfeld background for 5 minutes. Exponential non-linear regression analysis was used to determine seven parameters of DA function. These were time of cone–rod break, cone and rod final thresholds, and magnitude of change and time constant of the cone and rod limbs.
Results
The mean cone–rod break time with 95% confidence intervals (CI) was 0.098 (CI: −0.527, 0.330) minutes faster on retest (p = 0.630)). Fourteen of the 16 subjects demonstrated an increase or 'worsening' of their final cone and rod thresholds on the second visit. The mean final threshold differences on retest for the cone limb was 0.105 (CI: 0.032, 0.179) log cd/m2 (p = 0.008) and 0.093 (CI: −0.039, 0.225,) log cd/m2 (p = 0.155) for the rod limb. The magnitude of change for the cone limb was 0.016 (CI: −0.122, 0.155) log cd/m2 (p = 0.805) and −0.196 (CI: −0.435, 0.827) log cd/m2 (p = 0.518) for the rod limb, while the time constant on retest for the cone limb was −0.021 (CI: -0.128, 0.169) minutes, (p = 0.770) and 0.276 (CI: -0.424, 0.976) minutes (p = 0.410) for the rod limb.
Conclusions
None of the DA parameters that were examined demonstrated a learning effect of clinical significance between test and retest. None of the changes in mean from test to retest for the seven parameters were found to be statistically significant, and the changes were clinically negligible. Therefore, any change among patients that may occur in dark adaptation between a visit interval may be considered real, and not due to the effect of learning.


Similar content being viewed by others
References
Goodman G, Gunkel RD (1958) Familial electroretinographic and adaptometric studies in retinitis pigmentosa. Am J Ophthalmol 46:142–178
Alexander KR, Fishman GA (1984) Prolonged rod dark adaptation in retinitis pigmentosa. Br J Ophthalmol 68(8):561–569
Fulton AB, Hansen RM (1996) Mayer DL (1996) Vision in Leber congenital amaurosis. Arch Ophthalmol 114(6):698–703
Jacobson SG, Cideciyan AV, Regunath G, Rodriguez FJ, Vandenburgh K, Sheffield VC, Stone EM (1995) Night blindness in Sorsby’s fundus dystrophy reversed by vitamin A. Nat Genet 11:27–32
Kaiser–Kupfer MI, Caruso RC, Valle D (1991) Gyrate atrophy of the choroid and retina: long-term reduction of ornithine slows retinal degeneration. Arch Ophthalmol 109:1539–1548
Gouras P, Carr RE, Gunkel RD (1971) Retinitis pigmentosa in abetalipoproteinemia: Effects of vitamin A. Invest Ophthalmol 10(10):784–793
Russell RM, Smith VC, Multack R, Krill AE, Rosenberg IH (1973) Dark-adaptation testing for diagnosis of subclinical vitamin A deficiency and evaluation of therapy. Lancet 2:1161–1164
Walt RP, Kemp CM, Lyness L, Bird AC, Sherlock S (1984) Vitamin A treatment for night blindness in primary biliary cirrhosis. Br Med J 288:1030–1031
Russell RM, Morrison SA, Smith FR, Oaks EV, Caney EA (1978) Vitamin A reversal of abnormal dark adaptation in cirrhosis: study of effects on the plasma retinol transport system. Ann Intern Med 88(5):622–626
Abbott-Johnson WJ, Kerlin P, Abiad G, Clague AE, Cuneo RC (2011 Dark adaptation in vitamin A-deficient adults awaiting liver transplantation: improvement with intramuscular vitamin A treatment. Br J Ophthalmol 95(4):544–548
Weleber RG, Denman ST, Hanifin JM, Cunningham WJ (1986) Abnormal retinal function associated with isotretinoin therapy for acne. Arch Ophthalmol 104(6):831–837
Caruso RC, Zujewski J, Iwata F, Podgor MJ, Conley BA, Ayres LM, Kaiser-Kupfer MI (1998) Effects of fenretinide (4-HPR) on dark adaptation. Arch Ophthalmol 116(6):759–763
Decensi A, Torrisi R, Polizzi A, Gesi R, Brezzo V, Rolando M, Rondanina G, Orengo MA, Formelli F, Costa A (1994) Effect of synthetic retinoid fenretinide on dark adaptation and the ocular surface. J Natl Cancer Inst 86(2):105–110
Maguire AM, High KA, Auricchio A, Wright JF, Pierce EA, Testa F, Mingozzi F, Bennicelli JL, Ying GS, Rossi S, Fulton A, Marshall KA, Banfi S, Chung DC, Morgan JI, Hauck B, Zelenaia O, Zhu X, Raffini L, Coppieters F, De Baere E, Shindler KS, Volpe NJ, Surace EM, Acerra C, Lyubarsky A, Redmond TM, Stone E, Sun J, McDonnell JW, Leroy BP, Simonelli F, Bennett J (2009) Age-dependent effects of RPE65 gene therapy for Leber's congenital amaurosis: a phase 1 dose-escalation trial. Lancet 374(9701):1597–1605
Berger AS, Tezel TH, Del Priore LV, Kaplan HJ (2003) Photoreceptor transplantation in retinitis pigmentosa: short-term follow-up. Ophthalmology 110(2):383–91
Wood JM, Wild JM, Hussey MK, Crews SJ (1987) Serial examination of the normal visual field using Octopus automated projection perimetry: evidence for a learning effect. Acta Ophthalmol 65:325–333
Wild JM, Dengler-Harles M, Searle AET, O’Neill EC, Crews SJ (1989) The influence of the learning effect on automated perimetry in patients with suspected glaucoma. Acta Ophthalmol 67:537–545
Kulze JC, Stewart WC, Sutherland SE (1990) Factors associated with a learning effect in glaucoma patients using automated perimetry. Acta Ophthalmol 68:681–686
Wild JM, Searle AET, Dengler-Harles M, O’Neill EC (1991) Long-term follow-up of baseline learning and fatigue effects in the automated perimetry of glaucoma and ocular hypertensive patients. Acta Ophthalmol 69:210–216
Aulhorn E, Harms H (1972) Visual perimetry. In: Jameson D, Hurvich LM (eds) Handbook of sensory physiology, Volume VII. Springer, Berlin Heidelberg New York, pp 11–113
Arditi A, Cagenello R (1993) On the statistical reliability of letter chart visual acuity measurements. Invest Ophthalmol Vis Sci 34(1):120–129
van den Brom HJ, Kooijman AC, Blanksma LJ, van Rij G (1995) Measurement of visual acuity with two different charts; a comparison of results and repeatability in patients with cataract. Doc Ophthalmol 90(1):61–66
Raasch TW, Bailey IL MA (1998) Repeatability of visual acuity measurement. Optom Vision Sci 75(5):342–348
Rosser DA, Cousens SN, Murdoch IE, Fitzke FW, Laidlaw DAH (2003) How sensitive to clinical change are ETDRS logMAR visual acuity measurements? Invest Ophthalmol Vis Sci 44(8):3278–3281
Elliott DB, Sanderson K, Conkey A (1990) The reliability of the Pelli–Robson contrast sensitivity chart. Ophthalmic Physiol Opt 10(1):21–24
Reeves BC, Wood JM, Hill AR (1993) Reliability of high- and low-contrast letter charts. Ophthalmic Physiol Opt 13(1):17–26
Kiser AK, Mladenovich D, Eshraghi F, Bourdeau D, Dagnelie G (2006) Reliability and consistency of dark-adapted psychophysical measures in advanced eye disease. Invest Ophthalmol Vis Sci 47(1):444–52
Herse P (1995) A new method for quantification of the dynamics of dark adaptation. Optom Vis Sci 72(12):907–10
Omar R, Herse P (2004) Quantification of dark adaptation dynamics in retinitis pigmentosa using non-linear regression analysis. Clin Exp Optom 87(6):386–389
Peters AY, Locke KG, Birch DG (2000) Comparison of the Goldmann–Weekers dark adaptometer and LKC Technologies Scotopic Sensitivity tester-1. Doc Ophthalmol 101(1):1–9
Van Boemel GB (1999) Special skills and techniques. In: Ledford JK, David K, Campbell R (eds) The basic bookshelf for the eyecare professional. SLACK Inc., Thorofare NJ, pp 39–42
Snedecor GW, Cochran WG (1980) Statistical methods. Iowa State University Press, Ames, IA
Maloney CJ, Rastogi SC (1970) Significance tests for Grubbs’ estimators. Biometrics 26:671–676
Bland JB, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476):307–10
Lin LIK (1989) A concordance correlation coefficient to evaluate reproducibility. Biometrics 45:255–268
Havelius U, Bergqvist D, Falke P, Hindfelt B, Krakau T (1997) Impaired dark adaptation in symptomatic carotid artery disease. Neurology 49(5):1353–1359
Acknowledgements
I wish to acknowledge the support given in this study by the late Muriel Kaiser–Kupfer, MD and the late Marvin Podgor, PhD during my tenure at the National Eye Institute. I would also like to acknowledge the guidance for the project given by Rafael Caruso, MD.
Conflict of interest
The author has no financial disclosures or conflicts of interest that pertain to the information presented in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 32 kb)
Rights and permissions
About this article
Cite this article
Christoforidis, J., Zhang, X. Learning effect of dark adaptation among normal subjects. Graefes Arch Clin Exp Ophthalmol 249, 1345–1352 (2011). https://doi.org/10.1007/s00417-011-1706-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-011-1706-9