Abstract
Background
Improved survival of preterm neonates has increased the incidence of retinopathy of prematurity (ROP) in many middle-income countries.
Aim
This study aimed to verify the main risk factors for the development of ROP according to different gestational age (GA) groups.
Methods
A prospective cohort study including infants weighing ≤1,500 g or GA ≤32 weeks at birth was conducted. The main clinical outcomes were the occurrence of any stage of ROP and severe ROP. The perinatal variables considered for the study were: birth weight; GA; gender; to be small for GA (SGA); weight gain from birth to the sixth week of life; use of oxygen in mechanical ventilation or nasal CPAP; multiple gestations; therapeutic use of surfactant, indomethacin, and erythropoietin; occurrence of sepsis, meningitis, intraventricular hemorrhage, and patent ductus arteriosus; need for and volume of blood transfusion; and 10-min Apgar score. The patients were divided into three groups according to GA: (group 1) infants of GA ≤28 weeks at birth (n = 100); (group 2) infants of GA = 29–31 weeks at birth (n = 215); and (group 3) infants of GA ≥32 weeks at birth (n = 152).
Results
A total of 467 newborn infants were included. Mean BW and GA in the total cohort were 1,216.5 g (±278.3) and 30.3 weeks (±2.2), respectively. Gestational age groups were not matched for BW and SGA. Any stage of ROP occurred in 111 patients (23.8%) and 24 (5.1%) patients developed severe ROP. Only BW and volume of blood transfusion were significant factors for the occurrence of any stage of ROP in all groups. In group 1, GA, the twin situation, and use of erythropoietin were statistically significant factors. In group 2, only GA and need for blood transfusion were significant. In group 3, use of oxygen in mechanical ventilation, sepsis, and need for blood transfusion were significant for ROP onset. The logistic regression determined that patients in groups 2 and 3 were less likely to develop ROP than patients in group 1.
Conclusions
Patients in groups 1 and 2 developed ROP due to general immaturity, whereas bigger babies, of GA ≥32 weeks, developed ROP because they were “sicker” babies with more comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Retinopathy of prematurity (ROP) is a leading cause of childhood preventable blindness, and its earlier detection allows specific prevention and treatment approaches. Investigations on risk factors (RF) for ROP onset are, therefore, extremely important for ophthalmologists involved in neonatal screening programs to detect ROP among preterm infants.
Several institution- and population-based studies have investigated RF for the occurrence of ROP [1–8]. However, for the most part, data are unified into a single homogeneous cohort of patients, i.e., patients are not grouped according to gestational age (GA), although it is well known that preterm babies with lower GA are more likely to develop ROP and that clinical conditions of patients of lower GA are quite different from those of more mature infants (of greater GA) [9, 10].
This study aimed to analyze the prevalence and possible risk factors for ROP onset among patients attending a neonatal center in southern Brazil, dividing patients into different groups according to GA.
Methods
Patients
A prospective cohort study was conducted including preterm infants with a BW ≤1,500 g or GA ≤32 weeks at birth admitted to Hospital de Clínicas de Porto Alegre (HCPA), southern Brazil, between October 2002 and December 2008. The sample included all preterm infants who survived from the initial ophthalmological examination, performed between the fourth and sixth week after birth, to 45 weeks of postmenstrual age. There were no exclusion criteria. Preterm infants were divided into three groups according to GA: (group 1) patients of GA ≤28 weeks at birth; (group 2) patients of GA between 29 and 31 weeks at birth; and (group 3) patients of GA ≥32 weeks at birth.
All patients underwent an eye examination, which consisted of binocular indirect ophthalmoscopy following dilated pupil examination in both eyes associated with 0.5% tropicamide and 2.5% phenylephrine eye drops, using 28-diopter lens (Nikon, Melville, NY, USA), and a newborn infant eyelid speculum (Alfonso Eye Speculum, Storz, Bausch & Lomb Inc., San Dimas, CA, USA). Scleral indentation was performed when necessary.
All patients were examined in the neonatal intensive care unit (NICU) and, after hospital discharge, attended outpatient follow-up appointments until 45 weeks of postmenstrual age, or until effective stabilization of retinopathy was achieved after treatment. The screening sessions and the follow-up were performed according to the Brazilian guidelines to detect and treat ROP, which recommend screening for all babies born with a BW ≤1,500 g or GA ≤32 weeks and for those babies with risk factors such as respiratory distress syndrome, sepsis, intraventricular hemorrhage, babies who needed blood transfusions, and for those being born from multiple gestations. The initial ophthalmological examination should be performed between the fourth and sixth weeks of life and should be repeated weekly or more frequent according to the findings until full vascularization of the peripheral retina is observed or until 45 weeks of postmenstrual age. The Brazilian guidelines state treatable ROP in ROP zone I, any stage with plus disease, ROP in zone I, stage 3 with no-plus or ROP in zone II, stages 2 or 3 with plus disease or at least, at threshold ROP [11].
Outcome and variables
Clinical outcomes included the onset of any stage of ROP and the development of ROP severe enough to require treatment. Staging of disease was recorded according to the 1984/1987 International Classification of ROP [12, 13] and always corresponded to the highest stage of ROP found during patient follow-up. Severe ROP and threshold ROP were defined according to the Multicenter Trial of Cryotherapy for Retinopathy of Prematurity [14]. All eye examinations were performed by the same authors (JBFF, GUE, and PGBS).
The following continuous variables were prospectively analyzed: birth weight (BW); GA (evaluated by obstetric history, early obstetric ultrasound, and confirmed by newborn infant clinical examination); weight gain in grams from birth to the sixth week of life (defined as the baby’s weight measured at completed 6 weeks of life minus the BW); 10-min Apgar score; volume of blood transfusion; and units of erythropoietin administered. The categorical variables were also prospectively analyzed: infant being appropriate or small for GA (SGA <10th percentile for GA); gender; the twin situation (multiple or single gestation); use of oxygen in mechanical ventilation or by nasal continuous positive airway pressure (CPAP); use of indomethacin, surfactant, and erythropoietin; occurrence of sepsis, meningitis, patent ductus arteriosus, and any stage intraventricular hemorrhage; and need for blood transfusion. Sepsis, meningitis, and intraventricular hemorrhage were diagnosed by clinical examination, microbiological culture, and cranial ultrasound, respectively. The diagnosis of clinical sepsis was based on the presence of three or more of the following: apnea, difficult breathing, cyanosis, tachycardia or bradycardia, perfusion deficit or shock; irritability, lethargy, hypotonia and seizures; abdominal distention, vomits, dietary intolerance, gastric residue, hepatomegaly, idiopathic jaundice, thermal instability, petechiae or purpura; and a general poor appearance. Babies with positive blood cultures for coagulase-negative staphylococci and clinical sepsis had the following definitions to distinguish proven infection from contaminants: two positive blood cultures drawn within 2 days of each other or one positive blood culture and elevated C-reactive protein>10 mg/l within 2 days of blood culture. For all other pathogens, proven sepsis was defined by the presence of the organism in the blood culture.
Statistical methods and ethics
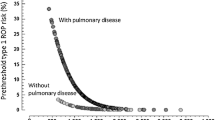
All statistical analyses were conducted using the SSPS software (SPSS 14.0 for Windows, SPSS Inc., Chicago, IL, USA). Incidence of ROP was calculated for all three groups. One-way ANOVA was used to analyze continuous variables between groups, and the Chi-square test was used to compare categorical variables. Variables considered for logistic regression were selected based on their significance after univariate analysis. Receiver operating characteristic (ROC) curves were used to demonstrate the predictive value of each significant variable for any stage or for severe ROP. The results were considered significant for p < 0.05, with 95% confidence intervals.
The study protocol was approved by the Research Ethics Committee of HCPA, no. 03–248, on Aug 20, 2003. The protocol also conforms to the provisions of the Declaration of Helsinki in 1995 (as revised in Edinburgh, 2000).
Results
A total of 467 preterm infants, corresponding to around 93% of all patients with a BW ≤1,500 g or GA ≤32 weeks admitted to the institution were screened for ROP and were included in this study. Mean BW and GA for the total cohort was 1,216.5 g (±278.3) and 30.3 weeks (±2.2), respectively. A total of 111 (23.8%) patients developed any stage ROP, and 24 (5.1%) patients developed severe ROP. Of these, 23 patients were treated with diode laser photocoagulation. The sample was divided into three different groups according to GA. The characteristics of the included patients are described in Table 1.
Incidence of ROP was significantly higher in group 1 and significantly lower in group 3, p < 0.001 (Table 2).
After univariate analysis, the significant variables for any stage ROP were, in group 1, BW, GA, weight gain, volume of transfused blood, and the twin situation; in group 2, BW, volume of transfused blood, weight gain, and need for blood transfusion; and in group 3, BW, volume of transfused blood, use of oxygen therapy in mechanical ventilation, sepsis, and need for blood transfusion.
The variables infant SGA or appropriate for GA, Apgar index, gender, use of oxygen by nasal CPAP, use of indomethacin, use of surfactant, use of erythropoietin, occurrence of meningitis, patent ductus arteriosus, units of erythropoietin, and intraventricular hemorrhage were not considered significant factors for the development of any stage ROP in all three study groups (Table 3).
For severe ROP, only BW was a significant RF in groups 1 and 2, whereas in group 1, GA and need for blood transfusion, were statistically significant for the development of severe ROP. Among patients in group 2, in addition to BW, need for and volume of blood transfusion, units of erythropoietin were significant RF for the occurrence of severe ROP. In group 3, no statistically significant RFs were observed (Table 4).
The logistic regression determined that patients in groups 2 and 3 were less likely to develop any stage ROP than patients in group 1. In group 1, GA showed significance at p = 0.024 and OR = 0.547 (95%CI 0.324–0.925), when adjusted for the twin situation, volume of blood transfusion and units of erythropoietin. In group 2, volume of blood transfusion showed significance at p = 0.009 and OR = 1.017 (95%CI 1.004–1.030), when adjusted for GA and need for blood transfusions. In group 3, volume of blood transfusion showed significance at p = 0.043 and OR = 1.032 (95%CI 1.001–1.063), when adjusted for GA, use of oxygen in mechanical ventilation, and need for blood transfusions (Table 5). It was not possible to perform the logistic regression for severe ROP due to the reduced number of this outcome in all three groups.
Area under the ROC curves for the most important and significant study variables is described in Table 6.
All patients weighing more than 1,500 g and of greater than 32 weeks’ GA at birth who developed ROP showed spontaneous regression of the disease and did not need to undergo treatment.
Of the 24 patients who developed severe ROP, 23 were treated with transpupillary diode laser photocoagulation in the retinal periphery, and one patient was not treated (Table 7). This patient developed ROP 5 and total bilateral blindness for not attending follow-up appointment due to NICU discharge. Among the 23 babies who required treatment for severe ROP, 22 had received blood transfusions and 20 erythropoietin therapy, 20 had sepsis, 15 had undergone mechanical ventilation, 13 received indomethacin, ten surfactant, eight had intraventricular hemorrhage, three had meningitis, three had persistent ductus arteriosus, and four were born from multiple gestation.
Discussion
The incidence of severe ROP during the study period was 5.1%, which is a very low percentage, even for countries with established standards of excellence in perinatal care [15].
Gilbert et al. [16] suggested that ROP prevails among preterm infants weighing less than 1,000 g at birth in industrialized countries and has emerged as a major cause of childhood blindness in developing countries, such as Brazil, and in several other places in Latin America, Asia, and Eastern Europe due to a sharp increase in the survival of very low birth weight (VLBW) preterm infants [17, 18]. Although these figures vary greatly among countries, survival rates of infants between 27 and 28 weeks’ GA at birth have been reported to reach approximately 90% [19]. This is not the present situation in the middle-income countries regarding survival rates. In a previous article, we related survival rates of 88.7% among babies with a BW >1,000 and ≤1,500 g (or with mean GA 30.9 ± 1.9), and only 47.8% among babies with a BW ≤1.000 g (or with mean GA 28.5 ± 2.1) at our institution [10].
Studies suggest that the incidence and severity of ROP are inversely related to BW and GA, with a few diagnoses of severe ROP (stage 3, threshold disease, or greater) being identified among infants with a BW >1,500 g or GA >32 weeks [20]. In population-based studies, the incidence of severe ROP was previously related as being higher among infants of less than 28 weeks’ GA or weighing less than 1,000 g [21, 22], although there are some reports of severe ROP among infants of 34–35 weeks’ GA and a BW >1,500 g, mainly in the presence of complications after birth [23].
In our study, the patients were grouped according to the GA. Group 1 comprised extremely premature babies (GA ≤28 weeks at birth). This GA range was chosen because similarity of clinical conditions usually happens among this group of patients. Group 2 comprised premature patients with GA of 29–31 weeks. In this range, usually, are inserted most of the patients screened for ROP in the middle-income countries context where standards of perinatal care have been improving in recent years. In group 3 were included babies over GA 32 weeks at birth. This is also a very homogenous group (regarding GA and BW) including bigger babies but with more comorbidities, some of them previously related with the onset of ROP, as sepsis [24], intraventricular hemorrhage [25], blood transfunded patients [26], or others. In our cohort of 467 patients, severe ROP occurred in 14% of group 1 patients, in 4.3% of group 2 patients, and in only 0.7% of group 3 patients, these differences being considered statistically significant (p < 0.001) (Table 2). No cases of severe ROP were observed among patients with a BW >1,500 g or GA >32 weeks at birth in our study. Our analysis revealed the influence of GA on the risk factors for occurrence of ROP. The population-based study conducted by Holmström et al. in Sweden, published in 1993, corroborates the statement concerning the importance of GA for the onset of ROP [27]. A number of studies analyzing perinatal RF for ROP have been published but only a few have analyzed the dynamic behavior of risk factors in relation to GA as has been performed in the present study. Koerner et al. in 1986 [28], published a very interesting study regarding the influence of GA and retinal maturity on the statistical behavior of risk factors for ROP and related that below 32 weeks GA, acidosis, hyperoxemia, GA, paCO2 levels and multiple birth are strong regressors while above 31 weeks GA, the most important regressor are multiple birth and acidosis and that GA and FiO2 >0.4 are much less influential on onset of ROP. The final conclusion of this study stated that it is the proportion of infants with an immature retinal vascularization in populations of given GA rather than the GA itself that is responsible for the widely varying importance of certain RF for ROP [28].
In our study, the main RF associated with the development of any stage of ROP among infants of lower GA (group 1) were: low GA, low BW, the twin situation, weight gain from birth to the sixth week of life, and volume of blood transfusion. Weight gain, need for and volume of blood transfusion, GA, and BW were statistically significant RF among patients in group 2. Among babies in group 3, who were bigger and more mature, but sicker, need for and volume of blood transfusion, need for oxygen therapy in mechanical ventilation, and occurrence of sepsis were significant factors for the development of any stage of ROP.
Birth weight, GA, and oxygen therapy are often considered the most important RF for ROP, but some studies have not found a significant correlation between BW and GA, as independent factors for onset of ROP, after logistic regression analyses. This situation might be explained within a statistical scope, since all patients included in ROP studies already have lower BW and GA when compared to a normal population, and mutual influence of variables varies greatly according to the statistical models selected for logistic regression in each study [29]. It is also worth noting that most patients in groups 1 and 2 in our study received oxygen therapy in mechanical ventilation or in nasal CPAP (Tables 3 and 4). Patients in group 3 disclosed more comorbidities as sepsis, bronchopulmonary dysplasia needing oxygen therapy in mechanical ventilation, use of erythropoietin and need for multiple blood red cells transfusions. Dammann et al. [30] investigated the role sepsis plays in the occurrence of ROP and concluded that, in their cohort of patients, severe ROP was absent in infants of greater than 29 weeks’ GA; however, when sepsis was present in these babies, there was an increased risk for development of any stage of ROP and severe ROP. Of the 23 patients who underwent laser treatment for severe ROP in our study, 20 (87%) had developed proven sepsis.
Weight gain from birth to the sixth week of life is a recently mentioned RF for predicting ROP. Our previously published article [31], and others [32, 33], disclosed the usefulness of this parameter in predicting any stage or severe ROP with some weeks in advance of onset of threshold ROP. The areas under the ROC curve of the weight gain, 0.719 and 0.76, respectively, in the whole cohort in our study, again disclosed that weight gain can be a better predictor for any stage of ROP or for severe, rather than other RFs.
HCPA is a university-based tertiary hospital located in Porto Alegre, southern Brazil, a city with a total population of approximately 3 million inhabitants. HCPA NICU has 20 intensive care beds. The prevalence of ROP at HCPA has been previously reported as occurring in 24.7% of infants with a BW ≤1,500 g or GA ≤32 weeks between 2002 and 2006 [34] and our survival rates reach around 88.7% among babies with a BW >1,000 and ≤1,500 g and only 47.8% among babies with a BW≤1,000 g [10]. Of the 24 patients who developed severe ROP and threshold disease severe enough to require treatment in our cohort at HCPA, 14 patients were in group 1, nine were in group 2, and only one patient was in group 3 (the group of bigger, but sicker, babies). However, none of these patients developed aggressive posterior ROP or ROP in zone I. No cases of aggressive posterior ROP were detected in our cohort, maybe by chance or, perhaps, by the higher mean of BW and GA of our patients if compared in these same parameters with data from the industrialized countries with lower BW and GA patients. It is of current knowledge that aggressive posterior ROP seems to occur especially among smaller and more immature patients.
Since the cohort of babies in the 28-week or less GA (group 1) was only 100 babies with a mean GA of 27.1 weeks corresponding to only 24.1% of the entire cohort, there may be limited generalizability of the results of this study to countries where a larger proportion of babies in a less than 26-week gestation group are surviving to develop ROP.
Conclusions
The general ROP incidence of 23.8% and severe ROP requiring laser treatment of 5.1% found in our study agrees within the variation reported by other institution-based studies. In group 3, only one preterm infant with a BW of 1,315 g and GA of 32 weeks at birth needed laser treatment.
Based on the dynamic analysis of the RF involved in the development of any stage of ROP and ROP severe enough to require treatment, we can hypothesize that smaller and more immature babies (lower GA and BW) are more likely to develop ROP solely due to general immaturity and not necessarily because they are “sicker” babies, whereas bigger and more mature babies can develop ROP due to the presence of a higher number of or more severe comorbidities (or because they were “sicker” babies) after premature birth.
It is worth mentioning that our observations are based on data from a single neonatal center and should not be extrapolated to patients from centers with neonatal care procedures different from those applied in a university-based tertiary hospital.
References
Shah VA, Yeo CL, Ling YL, Ho LY (2005) Incidence, risk factors of retinopathy of prematurity among very low birth weight infants in Singapore. Ann Acad Med Singapore 34:169–178
Akkoyun I, Oto S, Yilmaz G, Gurakan B, Tarcan A, Anuk D et al (2006) Risk factors in the development of mild and severe retinopathy of prematurity. J AAPOS 10:449–453
Allegaert K, Casteels I, Cossey V, Devlieger H (2003) Retinopathy of prematurity: any difference in risk factors between a high and low risk population? Eur J Ophthalmol 13:784–788
Yang MB, Donovan EF, Wagge JR (2006) Race, gender, and clinical risk index for babies (CRIB) score as predictors of severe retinopathy of prematurity. J AAPOS 10:253–261
Brown BA, Thach AB, Song JC, Marx JL, Kwun RC, Frambach DA (1998) Retinopathy of prematurity: evaluation of risk factors. Int Ophthalmol 22:279–283
Holmström G, Broberger U, Thomassen P (1998) Neonatal risk factors for retinopathy of prematurity-a population-based study. Acta Ophthalmol Scand 76:204–207
Seiberth V, Linderkamp O (2000) Risk factors in retinopathy of prematurity. a multivariate statistical analysis. Ophthalmologica 214:131–135
Palmer EA, Flynn JT, Hardy RJ, Phelps DL, Phillips CL, Schaffer DB et al (1991) Incidence and early course of retinopathy of prematurity. The cryotherapy for retinopathy of prematurity cooperative group. Ophthalmology 98:1628–1640
Karna P, Muttineni J, Angell L, Karmaus W (2005) Retinopathy of prematurity and risk factors: a prospective cohort study. BMC Pediatr 5:18
Fortes Filho JB, Eckert GU, Procianoy L, Barros CK, Procianoy RS (2009) Incidence and risk factors for retinopathy of prematurity in very low and in extremely low birth weight infants in a unit-based approach in southern Brazil. Eye 23:25–30
Zin A, Florencio T, Fortes Filho JB, Nakanami CR, Gianini N, Graziano RM et al (2007) Brazilian guidelines proposal for screening and treatment of retinopathy of prematurity (ROP). Arq Bras Oftalmol 70:875–883
The Committee for the Classification of Retinopathy of Prematurity (1984) An international classification of retinopathy of prematurity. Arch Ophthalmol 102:1130–1134
The International Committee for the Classification of the Late Stages of Retinopathy of Prematurity (1987) Arch Ophthalmol 105:906–912
Cryotherapy for Retinopathy of Prematurity Cooperative Group (1988) Multicenter trial of cryotherapy for retinopathy of prematurity: preliminary results. Pediatrics 81:697–706
Quinn GE (2007) Retinopathy of prematurity in Brazil: an emerging problem. J Pediatr (Rio J ) 83:191–193
Gilbert C, Fielder A, Gordillo L, Quinn G, Semiglia R, Visintin P et al (2005) Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics 115:e518–e525
Gilbert C, Rahi J, Eckstein M, O'Sullivan J, Foster A (1997) Retinopathy of prematurity in middle-income countries. Lancet 350(9070):12–14
Shah NJ (2005) Are the Indian retinopathy of prematurity criteria appropriate for Indian babies? Indian J Ophthalmol 53:295
Ingelfinger JR (2007) Prematurity and the legacy of intrauterine stress. N Engl J Med 17;356(20):2093–2095
Lermann VL, Fortes Filho JB, Procianoy RS (2006) The prevalence of retinopathy of prematurity in very low birth weight newborn infants. J Pediatr (Rio J) 82:27
Haines L, Fielder AR, Baker H, Wilkinson AR (2005) UK population based study of severe retinopathy of prematurity: screening, treatment, and outcome. Arch Dis Child Fetal Neonatal Ed 90:F240–F244
Darlow BA, Hutchinson JL, Henderson-Smart DJ, Donoghue DA, Simpson JM, Evans NJ (2005) Prenatal risk factors for severe retinopathy of prematurity among very preterm infants of the Australian and New Zealand Neonatal Network. Pediatrics 115:990–996
Jalali S, Matalia J, Hussain A, Anand R (2006) Modification of screening criteria for retinopathy of prematurity in India and other middle-income countries. Am J Ophthalmol 141:966–968
Manzoni P, Maestri A, Leonessa M, Mostert M, Farina D, Gomirato G (2006) Fungal and bacterial sepsis and threshold ROP in preterm very low birth weight neonates. J Perinatol 26:23–30
Procianoy RS, Garcia-Prats JA, Hittner HM, Adams JM, Rudolph AJ (1981) An association between retinopathy of prematurity and intraventricular hemorrhage in very low birth weight infants. Acta Paediatr Scand 70:473–477
Dani C, Reali MF, Bertini G, Martelli E, Pezzati M, Rubaltelli FF (2001) The role of blood transfusions and iron intake on retinopathy of prematurity. Early Hum Dev 62:57–63
Holmström G, el Azazi M, Jacobson L, Lennerstrand G (1993) A population based, prospective study of the development of ROP in prematurely born children in the Stockolm area of Sweden. Br J Ophthakmol 77:417–423
Koerner F, Bossi E, Wetzel C, Flury B (1986) Retinopathy of prematurity: the influence of gestational age and retinal maturity on the statistical behavior of risk factors. Graefes Arch Clin Exp Ophthalmol 224:40–45
Katz MH (2003) Multivariable analysis: a primer for readers of medical research. Ann Intern Med 138:644–650
Dammann O, Brinkhaus MJ, Bartels DB, Dordelmann M, Dressler F, Kerk J et al (2009) Immaturity, perinatal inflammation, and retinopathy of prematurity: a multi-hit hypothesis. Early Hum Dev. doi:10.1016/j.earlhumdev.12.010
Fortes Filho JB, Bonomo PP, Maia M, Procianoy RS (2009) Weight gain measured at 6 weeks after birth as a predictor for severe retinopathy of prematurity: study with 317 very low birth weight preterm babies. Graefes Arch Clin Exp Ophthalmol 247:831–836
Hellström A, Hard AL, Engström E, Niklasson A, Andersson E, Smith L et al (2009) Early weight gain predicts retinopathy in preterm infants: new, simple, efficient approach to screening. Pediatrics 123:e638–e645
García-Serrano JL, Ramírez-García MC, Piñar-Molina R (2009) Enfermedad plus em La retinopatia del prematuro de gestacíon múltiple. Análisis de riesgo. Arch Soc Esp Oftalmol 84:191–198
Fortes Filho JB, Barros CK, da Costa MC, Procianoy RS (2007) Results of a program for the prevention of blindness caused by retinopathy of prematurity in southern Brazil. J Pediatr (Rio J ) 83:209–216
Acknowledgements
The authors certify that the content has not been published or submitted for publication elsewhere. The authors also certify that the protocol for the research project has been approved by a suitably constituted Ethics Committee of the institution within which the work was undertaken under the number 03–248, and that it conforms to the provisions of the Declaration of Helsinki in 1995 (as revised in Edinburgh in 2000). The authors declare no financial support or relationships that may pose a conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Fortes Filho, J.B., Eckert, G.U., Valiatti, F.B. et al. The influence of gestational age on the dynamic behavior of other risk factors associated with retinopathy of prematurity (ROP). Graefes Arch Clin Exp Ophthalmol 248, 893–900 (2010). https://doi.org/10.1007/s00417-009-1248-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-009-1248-6