Abstract
Background
Corneal neovascularization is a major risk factor for graft failure after corneal transplantation. The purpose of this study was to investigate the effect of subconjunctival, perilimbal, and/or intrastromal bevacizumab (Avastin®) on corneal neovascularization in patients with penetrating keratoplasty (PKP).
Methods
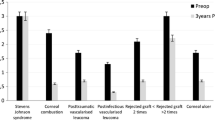
Fourteen eyes of 14 patients with high risk corneal transplantation and corneal neovascularization after PKP (nine men and five women with a mean age of 63 years) were included in this non-comparative interventional case series. Indications for PKP were: vascularized leucomas after herpetic keratitis and chemical burn, advanced pseudophakic bullous keratopathy with superficial and deep corneal vascularization, keratoconus, severe infection in hereditary corneal dystrophy, and failed corneal grafts. Subconjunctival, perilimbal, and/or intrastromal bevacizumab of dose of 2.5 mg/ 0.1 ml/ per affected quadrant was injected at the site of neovascularization in each patient at the end of surgery and/or at follow up visits. One or two injections were applied. At each visit a full eye examination with photo documentation was performed. Follow-up period was 2 to 8 months (mean 7.1 months).
Results
Decrease of corneal neovascularization was observed in eleven patients (78.6%). Regression of neovascularization with fading of small vessels was demonstrated. Despite high- risk patient pool, twelve grafts (85.7%) remained transparent for the period of observation, and patients maintained good visual acuity. In two patients with initial graft rejection and vascularization, subconjunctival and perilimbal application of bevacizumab was beneficial in overcoming the corneal inflammation and initial rejection. No adverse reactions have been detected to date in patients with subconjunctival, perilimbal, and/or intrastromal injection of bevacizumab.
Conclusions
Bevacizumab is an efficient and safe additional treatment option for improvement of prognosis in high-risk corneal transplantation with pre- and postoperative corneal neovascularization.





Similar content being viewed by others
References
George AJ, Larkin DF (2004) Corneal transplantation: the forgotten graft. Am J Transplant 4(5):678–685
Folkman J (1995) Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat Med 1:27–31
Philipp W, Speicher L, Humpel C (2000) Expression of vascular endothelial growth factor and its receptors in inflamed and vascularized human corneas. Invest Ophthalmol Vis Sci 41:2514–2522
Barraquer J, Rutllan J (1984) Microsurgery of the cornea; an Atlas and Textbook. Ediciones Scriba, Barcelona
Manzano RP, Peyman GA, Khan P, Carvounis PE, Kivilcim M, Ren M, Lake JC, Chévez-Barrios P (2007) Inhibition of experimental corneal neovascularisation by bevacizumab (Avastin). Br J Ophthalmol 91(6):804–807
Barros LF, Belfort R Jr (2007) The effects of the subconjunctival injection of bevacizumab (Avastin) on angiogenesis in the rat cornea. An Acad Bras Cienc 79(3):389–394
Tübingen Bevacizumab Study Group, Yoeruek E, Ziemssen F, Henke-Fahle S, Tatar O, Tura A, Grisanti S, Bartz-Schmidt KU, Szurman P (2008) Safety, penetration and efficacy of topically applied bevacizumab: evaluation of eyedrops in corneal neovascularization after chemical burn. Acta Ophthalmol 86(3):322–328
Bahar I, Kaiserman I, McAllum P, Rootman D, Slomovic A (2008) Subconjunctival bevacizumab injection for corneal neovascularization. Cornea 27(2):142–147
Erdurmus M, Totan Y (2007) Subconjunctival bevacizumab for corneal neovascularization. Graefes Arch Clin Exp Ophthalmol 245(10):1577–1579
Awadein A (2007) Subconjunctival bevacizumab for vascularized rejected corneal grafts. J Cataract Refract Surg 33(11):1991–1993
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have full control of all primary data, and agree to allow Graefe’s Archive for Clinical and Experimental Ophthalmology to review our data upon request.
Rights and permissions
About this article
Cite this article
Vassileva, P.I., Hergeldzhieva, T.G. Avastin use in high risk corneal transplantation. Graefes Arch Clin Exp Ophthalmol 247, 1701–1706 (2009). https://doi.org/10.1007/s00417-009-1170-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-009-1170-y