Abstract
Purpose
To report anatomic and visual outcomes of vitrectomy and indocyanine green (ICG)-assisted peeling of the retinal internal limiting membrane (ILM) in the treatment of diffuse diabetic macular edema.
Methods
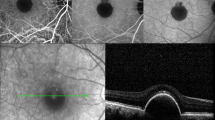
In a retrospective interventional case series, 15 eyes of 11 patients with refractory diffuse diabetic macular edema underwent pars plana vitrectomy with removal of the ILM, which was stained by intravitreal injection of ICG (0.1–0.2 ml of 0.5% ICG), performed by a single surgeon. The patients were followed up for 14–28 months (mean 20.5 months). The main outcome measures were assessment of macular edema by optical coherence tomography and determination of visual acuity and visual field.
Results
Intravitreal ICG visualized the ILM to facilitate complete removal of the structure. Qualitative assessment of optical coherence tomography images at the end of follow-up revealed that retinal thickness in the macula appeared nearly normal with or without reappearance of foveal pit in 11 of the 15 eyes (73.3%), decreased in 3 eyes (20.0%), and did not change in 1 eye (6.6%). Best-corrected visual acuity at the end of follow-up improved by 2 lines or more in 4 eyes (26.7%), virtually unchanged in 6 eyes (40.0%), and deteriorated by 2 lines or more in 5 eyes (26.7%). The mean logMAR visual acuity was 0.680 (approximately 12/60) preoperatively and 0.812 (approximately 9/60) postoperatively, the difference being not statistically significant (paired t-test, P=0.445). Seven (46.7%) of the 15 eyes developed optic nerve atrophy that occurred gradually within 6 months after surgery and caused irreversible peripheral visual field defect predominantly affecting the nasal field.
Conclusion
Intravitreal application of ICG is beneficial in uneventful ILM peeling to help resolution of diffuse diabetic macular edema, but it may potentially damage the optic nerve fibers and lead to unfavorable visual outcomes.


Similar content being viewed by others
References
Ando F, Sasano K, Ohba N, Hirose H, Yasui O (2004) Anatomical and visual outcomes after indocyanine green-assisted peeling of the retinal internal limiting membrane in idiopathic macular hole surgery. Am J Ophthalmol 137:609–614
Arima T, Uemura A, Otsuka S, Doi N, Nakao K (1998) Macular hole surgery associated peripheral visual field loss. Jpn J Ophthalmol 42:476–483
Bopp S, Lucke K, Hille U (1997) Peripheral visual field loss after vitreous loss after vitreous surgery for macular holes. Graefes Arch Clin Exp Ophthalmol 235:362 371
Brooks HL Jr (2000) Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology 107:1939–1948
Ciardella AP, Schiff W, Barile G, Vidne O, Sparrow J, Langton K, Chan S (2003) Persistent indocyanine green fluorescence after vitrectomy for macular hole. Am J Ophthalmol 136:174–177
Da Matta AP, Burk SE, Riemann CD, et al (2001) Indocyanine green-assisted peeling of the retinal internal limiting membrane during vitrectomy surgery for macular hole repair. Ophthalmology 108:1187–1192
Enaida H, Sakamoto T, Hisatomi T, Goto Y, Ishibashi T (2002) Morphological and functional damage of the retina caused by intravitreous indocyanine green in rat eyes. Graefes Arch Clin Exp Ophthalmol 209:209–213
Engelbrecht NE, Freeman J, Sternberg P, et al (2002) Retinal pigment epithelial changes after macular hole surgery with indocyanine green-assisted internal limiting membrane peeling. Am J Ophthalmol 133:89–94
Gandorfer A, Messmer EM, Ulbig KW, Kampik A (2000) Resolution of diabetic macular edema after successful removal of the posterior hyaloid and the internal limiting membrane. Retina 20:126–133
Gandorfer A, Messmer EM, Ulbig MW (2001) Indocyanine green selectively stains the internal limiting membrane. Am J Ophthalmol 131:387–388
Gandorfer A, Haritoglou C, Gass CA, Ulbig MW, Kampik A (2001) Indocyanine green-assisted peeling of the internal limiting membrane may cause retinal damage. Am J Ophthalmol 132:431–433
Gandorfer A, Haritoglou C, Gandorfer A, Kampik A (2003) Retinal damage from indocyanine green in experimental macular surgery. Invest Ophthalmol Vis Sci 44:316–323
Gass CA, Haritoglou C, Schaumberger M Kampik A (2003) Functional outcome of macular hole surgery with and without indocyanine green-assisted peeling of the internal limiting membrane. Graefes Arch Clin Exp Ophthalmol 241:716–720
Haritiglou C, Gandorfer A, Gass CA, Ulbig MW, Kampik A (2002) Indocyanine green-assisted peeling of the internal limiting membrane in macular hole surgery affects visual outcome: a clinicopathologic correlation. Am J Ophthalmol 134:836–841
Haritoglou C, Gass CA, Schaumberger M, Gandorfer A, Ulbig MW, Kampik A (2002) Long term follow-up after macular hole surgery with internal limiting membrane peeling. Am J Ophthalmol 134:661–666
Kampik A, Sternberg P (2003) Editorial. Indocyanine green in vitreomacular surgery—(Why) is it a problem? Am J Ophthalmol 136:527–529
La Heij EC, Hendrikse F, Kessels AG, Derhaag PJ (2001) Vitrectomy results in diabetic macular edema without evident vitreomacular traction. Graefes Arch Clin Exp Ophthalmol 239:264–270
Lewis H, Abrams GW, Blumenkrantz MS, Campo RV (1992) Vitrectomy for diabetic macular traction and edema associated with posterior vitreous traction. Ophthalmology 99:753–759
Otani T, Kishi S (2002) A controlled study of vitrectomy for diabetic macular edema. Am J Ophthalmol 134:214–219
Sakamoto T, Itaya K, Noda Y, Ishibashi T (2002) Retinal pigment epithelial changes after indocyanine green-assisted vitrectomy. Retina 22:794–796
Sippy BD, Engelbrecht NE, Hubbard GB, et al (2001) Indocyanine green effects on cultured human retinal pigment epithelial cells: implication for macular hole surgery. Am J Ophthalmol 132:433–435
Tachi N, Ogino N (1996) Vitrectomy for diffuse macular edema in cases of diabetic retinopathy. Am J Ophthalmol 22:258–260
Tadayoni R, Paques M, Girmens JF, Massin P, Gaudric A (2003) Persistence of fundus fluorescence after use of indocyanine green for macular surgery. Ophthalmology 110:604–608
Uemura A, Kanda S, Sakamoto Y, Kita H (2003) Visual field defects after uneventful vitrectomy for epiretinal membrane with indocyanine green-assisted internal limiting membrane peeling. Am J Ophthalmol 136:252–257
Author information
Authors and Affiliations
Corresponding author
Additional information
No proprietary interest
Rights and permissions
About this article
Cite this article
Ando, F., Yasui, O., Hirose, H. et al. Optic nerve atrophy after vitrectomy with indocyanine green-assisted internal limiting membrane peeling in diffuse diabetic macular edema. Graefe's Arch Clin Exp Ophthalmol 242, 995–999 (2004). https://doi.org/10.1007/s00417-004-0864-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-004-0864-4