Abstract
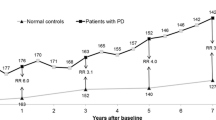
We studied prospectively the epidemiology, clinical impact and prediction of falls in 59 moderately affected patients with Parkinson's disease (PD) (mean UPDRS motor score 31.5; mean age 61 years) and 55 controls (mean age 60 years). At baseline, balance and gait were evaluated extensively. The retropulsion test (response to sudden shoulder pull) was executed first unexpectedly and five more times following prior warning. All persons used standardised scoring forms to document their falls during six months. Thirty patients (50.8 %) and eight controls (14.5 %) fell at least once (relative risk [RR] 6.1; 95 % confidence interval [CI] 2.5–15.1, p < 0.001). Recurrent (≥ 2) falls occurred in 15 patients (25.4 %), but in only two controls (RR 9.0; 95 % CI 2.0–41.7; p=0.001). Recurrent falls were more common among persons taking benzodiazepines (RR 5.0; 95 % CI 1.6–15.5; p < 0.01). Sixty-two percent of the falls in patients caused soft tissue injuries, but no fractures occurred. A fear of future falls was common (45.8 % of patients) and was accompanied by restriction of daily activities (44.1 % of patients). Seventy percent of falls reported by patients were ‘intrinsic’ (due to patient-related factors), but falls in controls were mainly (50 %) ‘extrinsic’ (due to environmental factors). None of the baseline posture and gait variables predicted falls adequately. The first ‘unexpected’ retropulsion test was more often abnormal than all subsequent (predictable) tests. Irrespective of its method of execution, the retropulsion test did not predict falls. A combination of asking for prior falls, disease severity and the Romberg test yielded the best overall diagnostic utility (sensitivity 65 % and specificity 98 %). Recurrent fallers were best predicted by disease severity (RR for Hoehn and Yahr stage 3 was > 100; 95 % CI 3.1–585) and asking for prior falls (RR 5.0; 95 % CI 1.2–20.9). We conclude that falls are common and disabling, even in relatively early stage PD. Recurrent fallers were best predicted by disease severity and presence of prior falls. Strategies to prevent falls in PD should particularly focus at intrinsic (patient-related) factors, such as minimising the use of benzodiazepines.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Received: 18 December 2000, Received in revised form: 15 March 2001, Accepted: 25 March 2001
Rights and permissions
About this article
Cite this article
Bloem, B., Grimbergen, Y., Cramer, M. et al. Prospective assessment of falls in Parkinson's disease. J Neurol 248, 950–958 (2001). https://doi.org/10.1007/s004150170047
Issue Date:
DOI: https://doi.org/10.1007/s004150170047