Abstract
Background
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disorder affecting the upper and lower motor neurons, which can lead to death from respiratory failure within 3–5 years after the onset of this disease. Nowadays, no drug can effectively slow down the progression of this disease. High-calorie therapy, an emerging complementary alternative treatment, has been reported in studies to prolong the survival time of patients, prevent muscle atrophy and provide a better prognosis. However, no systematic review and meta-analysis were performed to summarize the evidence of this therapy. This meta-analysis comprehensively evaluates the effectiveness and safety of high-calorie therapy for treating ALS.
Methods
We searched the electronic databases from inception to 1 April 2023: PubMed, Embase, Web of Science, Cochrane Library, Scopus, Ovid/Medline, and ProQuest. Randomized controlled trials (RCTs) that met the inclusion criteria were performed by meta-analysis. All statistical analyses were performed in STATA software.
Results
A total of six eligible RCTs were included in this meta-analysis, involving 370 ALS patients. The meta-analyses showed that high-calorie therapy had superiority in improving body weight (SMD = 1, 95% CI 0.36, 1.65) and BMI (SMD = 0.83, 95% CI 0.02, 1.63). With respect to safety, there was no difference between the high-calorie therapy and the control group regarding the number of adverse events (RR = 3.61, 95% CI 0.08, 162.49). However, ALSFRS-R scores (SMD = 0.34, 95% CI − 0.4, 1.08), survival rate (RR = 1.23, 95% CI 0.98, 1.55), and lipid profile (LDL: SMD = 0.21, 95% CI − 0.33, 0.75; HDL: SMD = 0.17, 95% CI − 0.37, 0.71; TC: SMD = 0.21, 95% CI − 0.33, 0.75), CRP (SMD = 0.85, 95% CI − 1.37, 3.06) showed no significant difference compared to the control groups.
Conclusions
High-calorie therapy is effective in gaining weight and BMI with few side effects. However, no significant superiority was detected in ALSFRS-R scores, survival time, lipid profile, and CRP indicator. The overall quality of the included studies is high, and the results have some credibility, but future corroboration by high-quality RCTs is also expected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS) is an incurable neurodegenerative disease affecting the upper and lower motor neurons in the spinal bulb, cerebral cortex, and spinal cord [1]. The clinical features of ALS are limb paralysis, muscle atrophy, dysphagia, dysarthria, and shortness of breath, which can lead to death due to respiratory failure [2]. According to the epidemiology of ALS, the incidence rate is estimated to be approximately 2.6 cases per 100,000 individuals annually [3], and the median survival period is only 30 months [4]. Nowadays, the etiology and pathogenesis of ALS remain unclear, and no effective cure has yet been found for this condition. Riluzole, a glutamatergic neurotransmission inhibitor, can slightly benefit the survival period and has been approved by the USA Food and Drug Administration (FDA). It is most commonly used in clinical practice [5]. However, an original cost-effective analysis found that the price range for riluzole fluctuated widely. ALS patients spend approximately $1000 per year on riluzole in the USA [6]. Nevertheless, in the UK, annual spending on the drug ranges from £834 to £3263 among ALS patients [7]. Overall, riluzole has been considered an expensive drug that imposes a significant financial burden on patients and families and can only prolong the life span for 3–5 months. In recent years, some emerging clinical investigational drugs, which the FDA also proved for the treatment of ALS, including relyvrio and in familial forms linked to SOD1 mutation, tofersen, have been able to alleviate disease progression to some extent. However, their effectiveness still needs to be corroborated by long-term follow-up and rigorously designed RCTs [8]. Considering the high expenses, a growing number of patients prefer palliative care and less-cost treatment.
Recently, weight loss has been considered as an independent prognostic factor for survival in ALS9. An observational study on malnutrition status during the disease found negative correlations between fluctuation in body mass index (BMI) and mortality [10]. The result showed a 30% increase in mortality for every one-point loss in BMI. The multicausal explanation of weight loss is that ALS patients with increasing resting energy expenditure exhibit a status of intrinsic hypermetabolism [11]. It has been proven that high-calorie nutrition can stabilize body weight. Targeting weight loss and supportive therapy for ALS patients may be effective, since increasing the calories in the diet of the ALS mice model showed positively prolonged survival [12] and a homogeneous trend in ALS patients with gastrostomy [13].
High-calorie diet therapy is an easy-to-implement, low-cost life intervention therapy. Compared to receiving treatment in professional medical institutions, lifestyle intervention has gained popularity among ALS patients worldwide for its advantages of being less painful and easier to accept. Therefore, researchers have shifted their focus to nutritional therapy to extend the survival period of ALS patients. High calorie includes a variety of nutritional therapies such as high-fat, high-carbohydrate, and high-protein nutrition [14]. Although this intervention can effectively stabilize body weight, there is no direct evidence showing that high-calorie therapies are safe and effective for ALS patients' survival period. Meanwhile, several studies have pointed out that this therapeutic intervention frequently accompanies a range of side effects [13, 14], such as gastrointestinal reactions and dysphagia. Evidence regarding high-calorie therapy's comparative safety and effectiveness remains uncertain. Given this scenario, evidence-based strategies are required to support judicious high-calorie therapy while ensuring the potential effects in ALS patients' management. Hence, we did a systematic review and meta-analysis to assess the safety and effectiveness of high-calorie therapy for ALS.
Methods
This meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [15] and has been registered in PROSPERO (CRD42023414623). There is no need for ethical approval because this is a systematic review.
Search strategy
We systematically searched the following electronic databases from inception to 1 April 2023: PubMed, EMBASE, Web of Science, Cochrane Library, Scopus, Ovid/Medline, and ProQuest. The search strategy used MeSH terms and keywords: ‘Amyotrophic Lateral Sclerosis,’ ‘energy intake,’ ‘Nutrition therapy,’ ‘randomized controlled trial,’ and ‘placebo.’ To ensure literature saturation, we comprehensively searched clinical trials, which are ongoing via the WHO International Clinical Trials Registry Platform (WHO ICTRP) and ClinicalTrials.gov. Preprint servers (such as medRxiv and Research Square) were searched for unpublished data. The search strategy of PubMed is shown in Table 1. The rest of the databases comply in the same way.
Inclusion and exclusion criteria
The following studies were included if they met the inclusion criteria: (1) RCTs of high-calorie therapy for ALS; (2) RCTs with high fat, high protein, and high carbohydrate as components of high calorie were included; (3) patients diagnosed with ALS by a professional medical institution, regardless of gender, age, nationality, or race; (4) the experimental groups on either high-calorie therapy only or combined high-calorie therapy with other common treatment; (5) the control group had conventional therapy.
The exclusion criteria of the studies were as follows: (1) ALS patients diagnosed with other neurodegenerative diseases such as Alzheimer's disease, Parkinson, and Huntington's disease; (2) reviews, case reports, animal experiments, and non-randomized controlled trials; (3) studies with missing data or repeated publications; (4) high-calorie therapy not being a heterogeneous intervention in the experimental group.
Study selection
All retrieved studies were managed in the Note Express software. Firstly, duplicates were removed. Then, study screening was carried out by two independent researchers separately. The studies that did not meet the inclusion criteria were excluded by reading the titles and abstracts. Researchers downloaded the remaining studies and read the full text to determine whether they could meet the inclusion criteria. Any disagreement on the selection process would be resolved by consulting the third researcher (Table 2).
Data extraction
Two reviewers independently extracted the following items from included studies: (1) first author, publication year, the sample size for each group, mean age; (2) interventions, comparisons, treatment time, courses of disease; (3) primary outcome: adverse events, ALSFRS-R scores, and survival rate; secondary outcome: body weight, body mass index, and laboratory parameters including high-density lipoprotein, low-density lipoprotein, and total cholesterol. If the original study presented pre- and post-intervention means and standard deviations (SD), we would follow the formulas provided in the Cochrane Handbook for the Evaluation of Intervention Systems to calculate the mean and SD of the differences. If the data were presented as interquartile range or median, the formulas derived by Wan et al. [16] were used for conversion.
Risk of bias and certainty of evidence assessment
Two blinded independent researchers used the Cochrane Risk of Bias Tool (ROB 2.0 (Centre for Evidence-Based Medicine Odense (CEBMO), Odense, DK)) [17] to evaluate the quality of included studies from five dimensions: (1) bias arising from the randomization process; (2) bias due to deviations from intended interventions; (3) bias due to missing outcome data; (4) bias in the measurement of the outcome; (5) bias in the selection of the reported result. Any disagreements were consulted with the third researcher for resolution.
Two independent researchers used the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) [18] approach to assess the evidence's certainty. Firstly, the initial level of certainty was determined by different study types. If the original study was RCT, high certainty could be awarded, but the observational study was regarded as low certainty. Then, the evidence would be degraded if there existed a risk of bias, inconsistency, indirectness, imprecision, or publication bias. Finally, the levels of evidence were classified as high, moderate, low, and very low. All procedures were implemented in GRADEpro software.
Statistical analysis
All statistical analyses were performed in STATA 15.0 software. We analyzed the data with risk ratios (RR) and 95% confidence interval (CI) for dichotomous variables. For continuous variables, MD and 95% CI were chosen to be analyzed. I2 statistics assess heterogeneity [19]. I2 > 75% is recognized as significant heterogeneity, 50% < I2 ≤ 75% as moderate heterogeneity, 25% < I2 ≤ 50% as low heterogeneity, and I2 ≤ 25% as homogeneity. We used the fixed-effects model if heterogeneity was low or homogeneous. Otherwise, we chose the random effects model. Sensitivity analysis was performed to detect the source of heterogeneity. Moreover, we used funnel plots and Egger’s regression test to assess the publication bias.
Results
Summary of included research
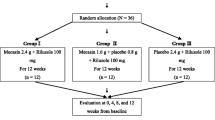
A total of 170 potential studies were retrieved from seven electronic databases based on the search strategy. After removing 49 duplicates, the remaining 121 studies were assessed for eligibility by reading the title and abstracts. We read the full texts of 19 potential studies for further review, and 6 RCTs involving 411 ALS patients were eligible for this meta-analysis. The flow diagram of the study selection is shown in Fig. 1.
The interventions varied slightly in the six included studies. Two studies treated ALS patients with high-fat therapy, one with high-protein diet, one was described as a high-calorie intervention only, one had both a high-carbohydrate and a high-fatty supplement group, and one divided the ALS patients into four groups with high-fat, ultrahigh-fat, ultrahigh-carbohydrate supplements and open control. Since this meta-analysis aims to evaluate the effectiveness and safety of high-calorie therapy, dose–response analysis was not included in our study. Of note, high-calorie therapy includes high carbohydrate, high fat, and high protein. The study of "Wills2014 (A)" refers to high-carbohydrate therapy, and "Wills2014 (B)" refers to high-fat therapy.
Quality assessment and risk of bias
The included studies were assessed using the Cochrane Risk of Bias Tool 2.0 to assess the five domains of RCTs associated with the risk of bias while giving an overall bias. Based on the results, almost all included studies were assessed with low risk. However, Saibo wang2022 was not described in detail in the section on deviations from intended interventions, and therefore had some methodological concerns with the overall risk, the included studies were all RCTs with no missing data, and the reasons for missing visits were explained in the studies. The assessment process is shown in Table 3.
Meta-analyses of outcomes
Primary outcome
(1) Adverse events (AEs).
Three included studies [20,21,22] reported the number of AEs, so they were subjected to meta-analysis. Random effects model was performed for significant heterogeneity detected (I2 = 87%). The meta-analysis results showed no difference between the high-calorie therapy and the control group regarding the number of AEs (RR = 3.61, 95% CI 0.08, 162.49, Fig. 2). Of note, it is reported that the main AEs of high-calorie therapy were temporary gastrointestinal symptoms (nausea, vomiting, diarrhea, constipation, abdominal pain), a feeling of fullness and loss of appetite, infections, pain in the extremities, cough, and dyspnea.
(2) ALSFRS-R scores.
Four included studies [20,21,22,23] reported ALSFRS-R scores, but Johannes Dorst et al. [20] did not disclose the raw data of ALSFRS-R scores in the original study. We failed to obtain the original data by connecting the authors. Hence, we excluded this research. Heterogeneity was apparent with I2 = 74.9%, Q-test P < 0.1. We chose the random effect model for this outcome analysis. The result showed no difference between the high-calorie therapy and control groups in the ALSFRS-R scores (SMD = 0.69, 95% CI − 0.2, 1.57, Fig. 3).
(3) Survival rate.
Three included studies [21, 22, 24] reported the number of deaths. There was homogeneity among the three studies (I2 = 2.2%, Cochran's Q test = 0.36). Therefore, we chose a fixed-effects model. It did not show that high-calorie therapy had superiority in improving survival rate compared with the control group (RR = 1.23, 95% CI 0.98, 1.55, Fig. 4).
Secondary outcome
(1) Body weight.
Four included studies[21, 22, 24] reported changes in body weight. An evident heterogeneity was detected among these four independent studies (I2 = 71.3%). We chose a random effect model for meta-analysis and the result showed that high-calorie group surpassed control groups in weight gain (SMD = 0.74, 95% CI 0.34, 1.13, Fig. 5).
(2) BMI
Four included studies[21,22,23,24] reported BMI. Significant heterogeneity was detected (I2 = 75.6%), so a random effects model was selected for meta-analysis. The results showed that high-calorie therapy increased BMI compared to that of controls (SMD = 0.29, 95% CI 0.05, 0.53, Fig. 6).
(3) Lipid profile.
Two included studies[22, 24] reported on lipid profile parameters, including LDL, HDL, and TC. There was a homogeneity among all three indicators (LDL: I2 = 69.5%, HDL: I2 = 15.3%, TC: I2 = 36.2%). Therefore, the fixed-effects model was selected for meta-analysis in three indicators respectively, and the results showed no difference between the high-calorie therapy compared to the control groups in any of the three indicators of lipid profile (LDL: SMD = − 0.02, 95% CI − 0.52, 0.47; HDL: SMD = 0.03, 95% CI − 0.46, 0.52; TC: SMD = 0.04, 95% CI − 0.45, 0.53, Fig. 7).
(4) C-reactive protein (CRP).
Two included studies reported on CRP indicators. We chose a random effects model for analysis because a significant heterogeneity was detected in two studies. The result showed no statistical difference between high-calorie therapy on CRP compared to controls (SMD = 0.5, 95% CI − 0.89, 1.89, Fig. 8).
Subgroup analyses
We performed subgroup analyses based on different types of high-calorie therapies. Although only six RCTs were included in this meta-analysis, four studies treated ALS patients with high-fat therapies. One was with high-protein and one with high-calorie therapy without a detailed description. Therefore, we mainly performed a statistical analysis of whether high-fat therapy can be effective and safe for ALS patients. However, the results of outcomes, including AEs, ALSFRS-R, survival time, body weight, and BMI, showed no significance compared to the control groups, as shown in Appendix Fig. 10.
GRADE analysis for the certainty of the evidence
Although RCTs of included studies were considered the highest level of evidence, the quality evidence of outcomes still needed to be interpreted cautiously. The outcomes of adverse events and survival rate were assessed as moderate evidence because the domains of imprecision and inconsistency did not meet the criterion. The outcome of ALSFRS-R scores was defined as low evidence, because the heterogeneity between included studies was significant. Furthermore, body weight, BMI, lipid profile, and CRP were assessed as very low-quality evidence by being downgraded to the risk of bias, indirectness, and imprecision (Fig. 9).
Discussion
The systematic review and meta-analysis focused on the safety and effectiveness of high-calorie therapy for treating amyotrophic lateral sclerosis patients. In this meta-analysis of six RCTs involving 370 individuals, high-calorie therapy increased body weight and BMI. Though there were, to some extent, improvements in the primary outcomes of ALSFRS-R scores and survival time, the pooled estimate did not achieve statistical significance. No severe adverse events were reported for the safety outcome, and common gastrointestinal reactions, such as diarrhea, nausea, and vomiting, were self-limiting and temporary. With the extensive reading of full texts of included studies, we revealed that the disease duration of patients was mainly in the range of 9–24 months. Therefore, we cautiously speculate that ALS patients with a disease duration of fewer than 2 years and milder symptoms who receive high-calorie therapy at an early stage may effectively gain weight and thus mitigate the progression of the disease.
Amyotrophic lateral sclerosis is a devastating neurodegenerative disease in which the leading cause of death is inadequate energy intake, malnutrition, and respiratory insufficiency due to complications of dysphagia. A direct association between nutritional status and ALS disease progression has been confirmed. Approximately, 16–55% of ALS patients are diagnosed with malnutrition, and most patients suffer weight loss from diagnosis. An independent prognostic factor linked to shorter survival is regarded as exacerbating muscle loss from denervation [25, 26]. Designing RCTs with stronger feasibility in terms of the debilitating nature of ALS is challenging. As part of a complementary and alternative intervention, high-calorie therapy, a kind of diet management, is feasible to have better compliance for ALS patients. The concept of high calorie includes nutrients with high fat, high carbohydrate, and high protein. We included RCTs in this meta-analysis as long as they used the above-mentioned three therapies. To date, neuroscientists and nutritionists have been dedicated to the role of high-calorie diets in ALS disease progression, and some observational studies have conducted high-calorie diets as an exposure factor. Researchers have also conducted RCTs, but no definitive conclusion exists among mutually independent studies on whether a high-calorie diet can slow disease progression. We systematically searched the databases and identified one systematic review without meta-analysis, which indicated that high-calorie therapy could gain body weight and BMI, prolong survival time, and improve functional status [27]. However, the conclusion from the small sample size was considerably mixed between the results of different studies. Indeed, the absence of meta-analysis may question the validity due to a lack of transparency [28]. Therefore, the results should be interpreted with caution.
To better evaluate which diet would have the best effect on ALS patients, we summarized the composition of dietary supplements in included studies. According to Table 4, all the dietary supplements studied comprised protein, carbohydrates, and fats. One was rich in vitamins, and after 12 months of follow-up, Saibo Wang et al. pointed out that the number of survivors in the experimental group was significantly superior to the number of survivors in the control group [24]. Xia et al. conducted Mendelian randomization of the relationship between dietary nutrients and ALS. Of note, they found that fat-soluble vitamins such as vitamin D and E delayed the progression of ALS and that unsaturated fatty acids were protective factors for ALS. In contrast, linoleic acid was a risk factor for ALS [29]. Less oral intake, potential hypermetabolic state, and progressive muscle atrophy resulted in malnutritional status and weight loss for ALS patients, associated with rapid progression. Emanuele et al. noted the significance of nutritional assessment at the earliest referral. When patients are diagnosed with ALS, adequate nutrition and restriction of pro-inflammatory food intake may help patients with weight maintenance or further weight gain, which can counteract the hypermetabolic state caused by ALS. Further nutritional research is warranted to provide a better understanding of the role of ALS in nutritional and metabolic abnormalities and explore the pathogenic mechanisms of ALS [30]. Boeun et al. conducted an observational study of nutritional intake and survival time in ALS with up to 6 years of follow-up, and they concluded that higher dose intake of fat and protein, especially from meat, in the early stage of the disease could prolong the survival time of ALS patients [31]. So far, there is still no definitive recommendation as to which diet is best for patients with MND. However, a narrative review of the published literature shows that researchers tend to recommend multivitamin-rich, high-protein, high-fat, and antioxidant foods for ALS patients, but not pro-inflammatory foods. Because one of the mechanistic hypotheses of the disease focuses on neuroinflammation, long-term consumption of pro-inflammatory foods may exacerbate neuroinflammation and worsen the disease.
At present, the pathogenesis of ALS remains unknown. However, studies have found that energy metabolism disorders are common in ALS patients [32]. On the one hand, the metabolic pathway of the tricarboxylic acid cycle in ALS patients is damaged [33]. On the other hand, the structure and function of mitochondria are destroyed, resulting in a decrease in the production of adenosine triphosphate [34]. Adenosine monophosphate-activated protein kinase (AMPK) is an intracellular stress sensor that maintains intracellular energy homeostasis [35]. When activated, AMPK consumes glucose, promotes fatty acid oxidation, and inhibits new cholesterol, lipid, and protein synthesis [36]. Studies have found that by feeding a high-fat diet to SOD1G93A mutant mice, the AMPK activity is inhibited, heat shock protein 70 (HSP70), as a downstream substance of the AMPK cascade pathway, is significantly increased, and HSP70, as a molecular chaperone, contributes to the correct folding of proteins and can prolong the survival time of mice [37, 38]. In summary, a high-fat diet may improve ALS survival time by inhibiting AMPK activity. With an extensive reading of studies relevant to the survival rate, it was found that Ludolph (2020)’s study with a sample size exceeding 100 per group significantly differed from the studies of Wang (2022) and Wills (2014), which had sample sizes of less than 30 per group. When we performed subgroup analysis by sample size exceeding 30 for each group, high-calorie therapy significantly improved patients' survival rates in studies with small samples (RR = 1.65, 95% CI 1.03, 2.66), and no heterogeneity was detected (I2 = 3%). Of note, RCTs with larger sample sizes are more stable for meta-analysis results, and small samples involving significant results should still be interpreted with caution. Interestingly, the high-fat therapy in Ludolph (2020) failed to confirm a significant difference in survival compared to the control group. However, stratified analysis by disease progression showed that the high-fat diet group had significantly prolonged survival in the subgroup of fast disease progression. It also prompted us that when high-fat therapy should be conducted, for what population, and how many calories to consume should be taken into account.
In this meta-analysis, six studies were retrieved according to inclusion criteria. Three of them were treated with high-fat therapy. One was a high-carbohydrate, one was a high-protein, and one was a high-calorie diet without a detailed description. For the safety outcome, adverse events in high-calorie therapy were temporary, and no statistical difference was detected compared to the control group. Survival rate and ALSFRS-R scores were defined as effective indicators for the effectiveness of outcomes. From the results of meta-analyses, no statistical significance was detected in these two indicators, accounting for a relatively short duration in the experiment or ALS patients who discontinued high-calorie therapy when they ended the experiment. In the meantime, we tried to conduct subgroup analyses with different interventions. In the subgroup of high-fat diets, three studies reported the adverse events and provided complete raw data for meta-analysis. However, the rest of the outcomes, including CNAQ, ALSFRS-R, and ROADS scores, were presented with descriptive analyses. Furthermore, the high-carbohydrate, high-protein, and high-calorie regimens were reported in only one study; thus, subgroup analyses could not be performed.
In summary, we performed a meta-analysis by including all randomized controlled trials currently studying high-calorie therapy for amyotrophic lateral sclerosis. We concluded that the therapy is effective for ALS patients' weight gain and BMI stabilization. Meanwhile, it is safe. Although survival rates and ALSFRS-R scores did not show superiority, this simple, low-cost, low-risk therapy is still worth investigating. Motor neuron disease is a multiorgan systemic disease, and ALS is one of its most common subtypes. There is mounting evidence from investigations demonstrating that it appears to be restricted to more than the central nervous system and affects systemic physiology. Furthermore, the clinical presentation is heterogeneous, which suggests that ALS is accompanied by a series of syndromes rather than one nosological entity. Amyotrophic lateral sclerosis is typically characterized by dysfunctional metabolism, and researchers are becoming more interested in using dietary interventions to treat neurological diseases [32, 39]. Because of the scarcity of treatment options for amyotrophic lateral sclerosis, more extensive, multicenter, long-course intervention randomized controlled trials should be conducted to explore the effectiveness of high-calorie therapy.
Limitations
This study has some inherent limitations. First, though the RCT methodology is robust evidence, the pooled analyses based on small sample sizes studies were not stable. Second, the limited included studies made it impossible to perform a dose–response analysis of high calorie to determine which level would be better to alleviate the progression of the disease.
Conclusion
The meta-analysis showed that high-calorie therapy was effective against a conventional diet regarding body weight and BMI gain, while no significant side effects occurred. However, no significant superiority was shown in survival time, ALSFRS-R score, CRP, and lipid profile. The level of GRADE evidence ranged from very low to moderate. The outcomes of survival time and ALSFRSR scores did not show statistical differences, which may be explained by the short duration of the intervention and the inability of patients to live with high-calorie therapy after the experiment. Nevertheless, further high-quality RCTs with long-term follow-ups are necessary to validate the efficacy and safety of high-calorie therapy for treating ALS.
Data availability
The data that support the findings of this study are available from the corresponding author, [Yan Zhao and Jing Zhou], upon reasonable request.
References
van Es MA, Hardiman O, Chio A, Al-Chalabi A, Pasterkamp RJ, Veldink JH, van den Berg LH (2017) Amyotrophic lateral sclerosis. Lancet 390(10107):2084–2098. https://doi.org/10.1016/S0140-6736(17)31287-4
Chen L, Zhang B, Chen R, Tang L, Liu R, Yang Y, Yang Y, Liu X, Ye S, Zhan S, Fan D (2015) Natural history and clinical features of sporadic amyotrophic lateral sclerosis in China. J Neurol Neurosurg Psychiatry 86(10):1075–1081. https://doi.org/10.1136/jnnp-2015-310471
Longinetti E, Fang F (2019) Epidemiology of amyotrophic lateral sclerosis: an update of recent literature. Curr Opin Neurol 32(5):771–776. https://doi.org/10.1097/WCO.0000000000000730
Hardiman O, Al-Chalabi A, Chio A, Corr EM, Logroscino G, Robberecht W, Shaw PJ, Simmons Z, van den Berg LH (2017) Amyotrophic lateral sclerosis. Nat Rev Dis Prim 3:17071. https://doi.org/10.1038/nrdp.2017.71
Jaiswal MK (2019) Riluzole and edaravone: a tale of two amyotrophic lateral sclerosis drugs. Med Res Rev 39(2):733–748. https://doi.org/10.1002/med.21528
Thakore NJ, Pioro EP, Udeh BL, Lapin BR, Katzan IL (2020) A cost-effectiveness framework for amyotrophic lateral sclerosis applied to riluzole. Value Health 23(12):1543–1551. https://doi.org/10.1016/j.jval.2020.06.012
Achtert K, Kerkemeyer L (2021) The economic burden of amyotrophic lateral sclerosis: a systematic review. Eur J Health Econ 22(8):1151–1166. https://doi.org/10.1007/s10198-021-01328-7
Martinez-Gonzalez L, Martinez A (2023) Emerging clinical investigational drugs for the treatment of amyotrophic lateral sclerosis. Expert Opin Investig Drugs 32(2):141–160. https://doi.org/10.1080/13543784.2023.2178416
Fayemendy P, Marin B, Labrunie A, Boirie Y, Walrand S, Achamrah N, Coeffier M, Preux PM, Lautrette G, Desport JC, Couratier P, Jesus P (2021) Hypermetabolism is a reality in amyotrophic lateral sclerosis compared to healthy subjects. J Neurol Sci 420:117257. https://doi.org/10.1016/j.jns.2020.117257
Marin B, Desport JC, Kajeu P, Jesus P, Nicolaud B, Nicol M, Preux PM, Couratier P (2011) Alteration of nutritional status at diagnosis is a prognostic factor for survival of amyotrophic lateral sclerosis patients. J Neurol Neurosurg Psychiatry 82(6):628–634. https://doi.org/10.1136/jnnp.2010.211474
Yang LP, Fan DS (2017) Diets for patients with amyotrophic lateral sclerosis: pay attention to nutritional intervention. Chin Med J (Engl) 130(15):1765–1767. https://doi.org/10.4103/0366-6999.211549
Dupuis L, Oudart H, Rene F, Gonzalez DAJ, Loeffler JP (2004) Evidence for defective energy homeostasis in amyotrophic lateral sclerosis: benefit of a high-energy diet in a transgenic mouse model. Proc Natl Acad Sci USA 101(30):11159–11164. https://doi.org/10.1073/pnas.0402026101
Dorst J, Cypionka J, Ludolph AC (2013) High-caloric food supplements in the treatment of amyotrophic lateral sclerosis: a prospective interventional study. Amyotroph Lateral Scler Frontotemporal Degener 14(7–8):533–536. https://doi.org/10.3109/21678421.2013.823999
Dorst J, Kuhnlein P, Hendrich C, Kassubek J, Sperfeld AD, Ludolph AC (2011) Patients with elevated triglyceride and cholesterol serum levels have a prolonged survival in amyotrophic lateral sclerosis. J Neurol 258(4):613–617. https://doi.org/10.1007/s00415-010-5805-z
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hrobjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, McKenzie JE (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372:n160. https://doi.org/10.1136/bmj.n160
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
Stewart LA, Clarke M, Rovers M, Riley RD, Simmonds M, Stewart G, Tierney JF (2015) Preferred reporting items for systematic review and meta-analyses of individual participant data: the PRISMA-IPD statement. JAMA 313(16):1657–1665. https://doi.org/10.1001/jama.2015.3656
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, Hill S, Jaeschke R, Leng G, Liberati A, Magrini N, Mason J, Middleton P, Mrukowicz J, O’Connell D, Oxman AD, Phillips B, Schunemann HJ, Edejer T, Varonen H, Vist GE, Williams JJ, Zaza S (2004) Grading quality of evidence and strength of recommendations. BMJ 328(7454):1490. https://doi.org/10.1136/bmj.328.7454.1490
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Dorst J, Doenz J, Kandler K, Dreyhaupt J, Tumani H, Witzel S, Schuster J, Ludolph AC (2022) Fat-rich versus carbohydrate-rich nutrition in ALS: a randomised controlled study. J Neurol Neurosurg Psychiatry 93(3):298–302. https://doi.org/10.1136/jnnp-2021-328331
Ludolph AC, Dorst J, Dreyhaupt J, Weishaupt JH, Kassubek J, Weiland U, Meyer T, Petri S, Hermann A, Emmer A, Grosskreutz J, Grehl T, Zeller D, Boentert M, Schrank B, Prudlo J, Winkler AS, Gorbulev S, Roselli F, Schuster J, Dupuis L (2020) Effect of high-caloric nutrition on survival in amyotrophic lateral sclerosis. Ann Neurol 87(2):206–216. https://doi.org/10.1002/ana.25661
Wills AM, Hubbard J, Macklin EA, Glass J, Tandan R, Simpson EP, Brooks B, Gelinas D, Mitsumoto H, Mozaffar T, Hanes GP, Ladha SS, Heiman-Patterson T, Katz J, Lou JS, Mahoney K, Grasso D, Lawson R, Yu H, Cudkowicz M (2014) Hypercaloric enteral nutrition in patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled phase 2 trial. Lancet 383(9934):2065–2072. https://doi.org/10.1016/S0140-6736(14)60222-1
Silva LB, Mourao LF, Silva AA, Lima NM, Almeida SR, Franca MJ, Nucci A, Amaya-Farfan J (2010) Effect of nutritional supplementation with milk whey proteins in amyotrophic lateral sclerosis patients. Arq Neuropsiquiatr 68(2):263–268. https://doi.org/10.1590/s0004-282x2010000200021
Wang S, Yuan T, Yang H, Zhou X, Cao J (2022) Effect of complete high-caloric nutrition on the nutritional status and survival rate of amyotrophic lateral sclerosis patients after gastrostomy. Am J Transl Res 14(11):7842–7851
Janse VMM, van Eijk R, van der Burgh HK, Tan H, Westeneng HJ, van Es MA, Veldink JH, van den Berg LH (2020) Prognostic value of weight loss in patients with amyotrophic lateral sclerosis: a population-based study. J Neurol Neurosurg Psychiatry 91(8):867–875. https://doi.org/10.1136/jnnp-2020-322909
Malkki H (2014) Motor neuron disease: high-calorie diet might delay amyotrophic lateral sclerosis. Nat Rev Neurol 10(4):181. https://doi.org/10.1038/nrneurol.2014.40
Kellogg J, Bottman L, Arra EJ, Selkirk SM, Kozlowski F (2018) Nutrition management methods effective in increasing weight, survival time and functional status in ALS patients: a systematic review. Amyotroph Lateral Scler Frontotemporal Degener 19(1–2):7–11. https://doi.org/10.1080/21678421.2017.1360355
Campbell M, Katikireddi SV, Sowden A, Thomson H (2019) Lack of transparency in reporting narrative synthesis of quantitative data: a methodological assessment of systematic reviews. J Clin Epidemiol 105:1–9. https://doi.org/10.1016/j.jclinepi.2018.08.019
Xia K, Wang Y, Zhang L, Tang L, Zhang G, Huang T, Huang N, Fan D (2022) Dietary-derived essential nutrients and amyotrophic lateral sclerosis: a two-sample mendelian randomization study. Nutrients. https://doi.org/10.3390/nu14050920
D’Amico E, Grosso G, Nieves JW, Zanghi A, Factor-Litvak P, Mitsumoto H (2021) Metabolic abnormalities, dietary risk factors and nutritional management in amyotrophic lateral sclerosis. Nutrients. https://doi.org/10.3390/nu13072273
Kim B, Jin Y, Kim SH, Park Y (2020) Association between macronutrient intake and amyotrophic lateral sclerosis prognosis. Nutr Neurosci 23(1):8–15. https://doi.org/10.1080/1028415X.2018.1466459
Dupuis L, Pradat PF, Ludolph AC, Loeffler JP (2011) Energy metabolism in amyotrophic lateral sclerosis. Lancet Neurol 10(1):75–82. https://doi.org/10.1016/S1474-4422(10)70224-6
Geevasinga N, Menon P, Ozdinler PH, Kiernan MC, Vucic S (2016) Pathophysiological and diagnostic implications of cortical dysfunction in ALS. Nat Rev Neurol 12(11):651–661. https://doi.org/10.1038/nrneurol.2016.140
Vandoorne T, De Bock K, Van Den Bosch L (2018) Energy metabolism in ALS: an underappreciated opportunity? Acta Neuropathol 135(4):489–509. https://doi.org/10.1007/s00401-018-1835-x
Carling D, Sanders MJ, Woods A (2008) The regulation of AMP-activated protein kinase by upstream kinases. Int J Obes (Lond) 32(Suppl 4):S55–S59. https://doi.org/10.1038/ijo.2008.124
Hardie DG (2007) AMP-activated/SNF1 protein kinases: conserved guardians of cellular energy. Nat Rev Mol Cell Biol 8(10):774–785. https://doi.org/10.1038/nrm2249
Yenari MA, Liu J, Zheng Z, Vexler ZS, Lee JE, Giffard RG (2005) Antiapoptotic and anti-inflammatory mechanisms of heat-shock protein protection. Ann N Y Acad Sci 1053:74–83. https://doi.org/10.1196/annals.1344.007
Zhao Z, Sui Y, Gao W, Cai B, Fan D (2015) Effects of diet on adenosine monophosphate-activated protein kinase activity and disease progression in an amyotrophic lateral sclerosis model. J Int Med Res 43(1):67–79. https://doi.org/10.1177/0300060514554725
McDonald TS, McCombe PA, Woodruff TM, Lee JD (2020) The potential interplay between energy metabolism and innate complement activation in amyotrophic lateral sclerosis. FASEB J 34(6):7225–7233. https://doi.org/10.1096/fj.201901781
Acknowledgements
We thank the Program supported by the Department of Science and Technology of Hubei Province for funding this research. We also thank Ziyue Xiong, a linguistics graduate from University of California, Los Angeles, for writing and editorial assistance.
Funding
This work was funded by the Program supported by the Department of Science and Technology of Hubei Province (2022BCA055).
Author information
Authors and Affiliations
Contributions
QZ designed the study and wrote the original draft. DL and DY conducted the literature searches and screening process. JZ and HH evaluated the quality of included studies and extracted data. DX and YZ performed the software and analyzed the data. DX and YZ rated the studies for methodological quality and provided professional guidance. All authors have approved the manuscript and contributed to this work.
Corresponding authors
Ethics declarations
Conflicts of interest
All authors declared that they have no competing or conflicting interests.
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhu, Q., Xu, D., Huang, H. et al. The safety and effectiveness of high-calorie therapy for treating amyotrophic lateral sclerosis: a systematic review and meta-analysis. J Neurol 270, 4729–4743 (2023). https://doi.org/10.1007/s00415-023-11838-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-11838-4