Abstract
5q-associated spinal muscular atrophy (SMA) is a rare genetic disease caused by mutations in the SMN1 gene, resulting in a loss of functional SMN protein and consecutive degeneration of motor neurons in the ventral horn. The disease is clinically characterized by proximal paralysis and secondary skeletal muscle atrophy. New disease-modifying drugs driving SMN gene expression have been developed in the past decade and have revolutionized SMA treatment. The rise of treatment options led to a concomitant need of biomarkers for therapeutic guidance and an improved disease monitoring. Intensive efforts have been undertaken to develop suitable markers, and numerous candidate biomarkers for diagnostic, prognostic, and predictive values have been identified. The most promising markers include appliance-based measures such as electrophysiological and imaging-based indices as well as molecular markers including SMN-related proteins and markers of neurodegeneration and skeletal muscle integrity. However, none of the proposed biomarkers have been validated for the clinical routine yet. In this narrative review, we discuss the most promising candidate biomarkers for SMA and expand the discussion by addressing the largely unfolded potential of muscle integrity markers, especially in the context of upcoming muscle-targeting therapies. While the discussed candidate biomarkers hold potential as either diagnostic (e.g., SMN-related biomarkers), prognostic (e.g., markers of neurodegeneration, imaging-based markers), predictive (e.g., electrophysiological markers) or response markers (e.g., muscle integrity markers), no single measure seems to be suitable to cover all biomarker categories. Hence, a combination of different biomarkers and clinical assessments appears to be the most expedient solution at the time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
5q-associated spinal muscular atrophy (SMA) is a rare genetic disease caused by homozygous deletions or compound heterogeneous mutations in the SMN1 gene, resulting in a loss of functional survival motor neuron (SMN) protein [1]. The SMN protein is essential for spinal alpha motor neuron vitality, and its depletion leads to degeneration of these motor neurons with secondary skeletal muscle atrophy, which clinically manifest in proximal paralysis. In much lesser quantities, full-length SMN production is also provided by the SMN2 gene, centromeric copies of SMN1 [2]. However, due to a point mutation at position 6 of exon 7 in SMN2 and an intronic splicing silencer N1 (ISS-N1), splicing of exon 7 of SMN2 pre-mRNA is altered leading to production of only low levels of SMN protein [3]. The clinical phenotype of patients with SMA is most likely multifactorial but generally correlates with SMN2 copy numbers and the amount of the resulting functional SMN protein (SMN-P) [4–6].
While there were no specific treatment options for SMA for years, some promising therapeutic options have risen in the past decade. Currently approved therapeutic strategies aim at increasing the amount of functional SMN protein by either SMN1 gene replacement (onasemnogene abeparvovec, [7–9]) or SMN2 splice modulation (nusinersen [10–14], risdiplam [15, 16, 17–19]) and have shown beneficial therapeutic response [20–22]. SMN-independent approaches are currently tested in ongoing randomized trials. Apitegromab is a myostatin activation inhibitor that has shown to stabilize and improve motor function in patients with SMA additionally to nusinersen in a phase 2 study [23], with an increase in the Hammersmith functional motor scale expanded (HFMSE [24]) of ≥ 1 point in ≥ 40% of the patients and ≥ 3 points in ≥ 20% of the patients. In mouse models, BIO101, a Mas receptor activator, has shown beneficial effects on fatigue levels and motor function [25]. Reldesemtiv is a fast skeletal muscle activator that selectively binds to the fast skeletal troponin complex and sensitizes it to calcium [26], thereby increasing muscle strength relative to the neuronal input. In a phase 2 study, it has proven to increase the slow vital capacity and the six-minute walk test (6MWT) in SMA patients [27]. Amifampridine is a voltage-dependent potassium channel blocker that has proven to empower neuromuscular transmission and muscle function in Lambert–Eaton myasthenic syndrome [28] and most recently in ambulatory SMA type 3 patients [29].
As more therapeutic strategies evolve, there is a rising need for biomarkers, especially to stratify for treatment eligibility and to monitor treatment efficacy. Biomarkers can be classified in different categories, depending on their purpose (see Fig. 1). The U.S. Food and Drug Administration (FDA) has formed a working group that has defined seven main categories of biomarkers [30]. These main categories are (1) diagnostic biomarkers that help to detect or confirm the presence of a disease or to identify individuals with a subtype of the disease, (2) prognostic biomarkers that identify the likelihood of a clinical event or disease progression in an individual with the disease, (3) predictive biomarkers that identify individuals who are more likely to experience an effect from a certain medical product, (4) response biomarkers that show that a biological response has occurred in an individual exposed to medical treatment (e.g., pharmacodynamic biomarkers that measure the biological activity of the medical product, not necessarily drawing conclusions to clinical outcome) (5) monitoring biomarkers for repeated assessment of the status of a disease or the effect of medical treatment, (6) safety biomarkers that indicate toxicity of medical treatment, and (7) risk biomarkers that reflect the potential for developing a disease in an individual who does not currently have the disease [30, 31].
A lot of putative biomarker sources for SMA have been discussed, including molecular analytes, physiologic, imaging-based and clinical as well as digital biomarkers (see Fig. 2, [32, 31, 33]). Besides being valid and reliable, routine biomarkers should be easy and quick to obtain, economic and allow repeated evaluations [34]. Given their relatively easy and fast accessibility and widely available analytic techniques, the main focus will be shifting to blood-derived biomarkers. The project “Biomarkers for SMA” has been established to identify and validate such markers with a focus on correlation to motor function and other functional outcome measures. The program has identified more than 200 candidate blood-derived molecular biomarkers [35] and has proposed a plasma protein panel for SMA including 27 parameters [36]. However, the panel has not entered clinical routine yet.
To date, the in-clinic assessment of motor function as a diagnostic biomarker has been implemented in the management of SMA. However, although major efforts have been made, no physiological, imaging-based, digital or molecular biomarkers have been validated in the clinical routine in SMA patients so far. In this narrative review, we will briefly discuss previously proposed candidate biomarkers for SMA and will focus the discourse on the adoption of skeletal muscle biomarkers, especially given the muscle as a new therapeutic target.
Biomarkers
Molecular biomarkers
SMN protein (and other SMN-related biomarkers)
SMN protein
The amount of functional SMN-P determines the SMA phenotype with a milder phenotype in the presence of higher SMN-P levels in the ventral horn [37]. It consequently is the canonical view in the scientific community that SMN-P levels would be the most accurate biomarker for both prognostic and pharmacodynamic monitoring, especially under the systemically SMN-increasing therapy risdiplam. However, there is dispute about the best way of routinely assessing and interpreting SMN-P (compare [38]). Different groups showed that SMN-P expression varies between different tissue types [39–41]. The most easily accessible tissue for biomarkers in general is blood and a significant amount of biomarker research in SMA has been involved with measuring SMN-P and SMN-related biomarkers in the peripheral blood. SMN-P has evolved as the most promising of these biomarkers.
Some studies found that SMN-P levels in the peripheral blood relate to SMN copy numbers, the severity of denervation, and overall disease activity in mostly functionally more affected SMA patients [42–45] whereas different groups found neither a correlation between SMN-P blood levels and SMN copy numbers nor between SMN-P levels and muscle function and integrity [46, 43, 47]—or both findings at a time [43]. It is further unclear if and how blood SMN-P levels correlate with SMN-P levels in the spinal cord or the skeletal muscle [48]. SMN-P blood levels are generally lower than in the central nervous system (CNS [49]). Further, blood SMN-P levels did not increase under strictly centrally elevated SMN mRNA levels in motor neurons [50]. Given this discrepancy between central and peripheral protein levels, conclusions on central nervous processes are, therefore, limited and must be drawn carefully.
When combining the evidence from the above-mentioned studies, it becomes clear that SMN-P has the potential to serve as a diagnostic and prognostic biomarker in SMA, but that its ability to reflect dynamic processes such as disease progression or therapeutic response is still limited. It is particularly complicated as several studies suggest changing SMN-P dependency throughout the development [51] with high SMN-P levels pre- and 3 months post-natal that decrease with age [52, 53]. The cellular effects of decreasing SMN-P levels with age are not yet understood and might limit the ability to use SMN-P for disease monitoring.
With greater technical abilities and an increased understanding of pathophysiological processes in SMA, we do, however, expect enlightening research on SMN-P as a promising candidate biomarker. Its importance becomes clearer when looking at the current therapeutic options which aim at increasing SMN-P levels in the ventral horn. If a reflection of central nervous SMN-P levels can be achieved peripherally, clinical monitoring of therapy response could be supported by objective and easily accessible laboratory parameters. As a promising first step, risdiplam has been found to increase SMN-P blood levels in animal models and humans with SMA [15], indicating that this peripheral increase might reflect levels in other peripheral organs such as muscle, or the CNS [54] (see Table 1).
SMN mRNA transcripts (SMN2-full length and SMN transcript lacking exon 7)
Briefly, compared to controls, both parameters were decreased in the peripheral blood of patients with SMA type 1 but not in types 2 and 3 [47, 45]. Although there are conflicting data, there is no clear evidence for a correlation between SMN mRNA transcripts and SMA phenotypes [55] or type-specific motor function [56] (see Table 2).
Limitations of SMN-derived molecular biomarkers
Although deficiency of SMN proteins and transcripts is the pathophysiological hallmark of SMA, its assessment in body fluids seems to be less useful because of only weak correlations to clinical characteristics.
Markers of neurodegeneration
Neurofilament
Neurofilaments (NFs) are tissue-specific classes of intermediate filaments that provide structural support and integrity for neurons [57]. They are released with neuronal damage and have been found elevated in numerous neurodegenerative diseases, such as amyotrophic lateral sclerosis [58, 59]. Interestingly, brain volume and change of brain volume have a relevant influence on NF levels [60]. NFs are composed of four subunits with a half-life of up to 8 months and can be assessed in both blood and cerebrospinal fluid (CSF), which makes them easily accessible markers for previous neuronal damage [31]. Especially the phosphorylated heavy chain of NFs (pNFH) and the light chain (NFL) have been studied.
In terms of SMA, elevated CSF pNFH levels have predominantly been found elevated in patients with SMA type 1 [61, 62] and specifically in those younger than 4 years [63]. In these studies, higher baseline pNFH levels correlated with early onset and lower motor function in all age groups and declined to reference levels over time. These findings were confirmed in the CHERISH study, in which pNFH levels decreased under nusinersen regardless of timepoint of treatment initiation [64]. This decline was more rapid in patients treated with nusinersen compared to those without disease-modifying therapy [65, 66], pointing to a pharmacodynamic value of pNFH. In pre-symptomatic infants with SMA, pNFH correlates with future motor milestone achievement and was the strongest predictor of motor function achievement [12].
Whereas NFs are promising biomarkers in infants with SMA, there is somewhat contradictory data in SMA types 2–4 in adolescence or adulthood. ELISA-based analyses showed no difference of serum pNFH [67] and NFL levels between healthy controls and SMA patients neither at baseline nor after treatment with nusinersen after short observation periods [68]. In CSF, NFs were similar to controls but decreasing CSF levels of pNFH and NFL during nusinersen treatment have been shown using commercially available ELISA kits [69] or the high-precision method ELLA [62], particularly in more severely affected SMA types. When corrected to muscle mass, NFL in CSF distinguished strongly between adult SMA types 2 and 3, showing higher ratios in the more severe type [62]. Therefore, normalization of NFs might be useful in progressed disease stages with already big loss of motor neurons to improve the value of these biomarkers. In another study using the highly specific single molecular array (SIMOA), no dynamic of pNFH and NFL level in CSF and serum during nusinersen treatment was reported [70]. Two studies report a negative correlation with motor function [70, 68] while one showed no correlation between NFs and motor function change [69] and one showed a positive correlation between pNFH at baseline with motor function gain under nusinersen [71].
Overall NFs seem to be reliable biomarkers for infants with SMA in terms of prognostic considerations and treatment response to nusinersen but remain unclear in adult-onset SMA or progressed disease stages in all SMA types. However, one should consider that nusinersen was first been approved in 2016 and adolescent and adult patients might have suffered from CNS motor pool exhaustion or muscular skeletal complications (e.g., contractures, scoliosis) that might have limited accurate NF assessment or reliable motor function assessment [31]. Nitz et al. hypothesized that non-neurodegenerative processes such as glia-mediated neuroinflammation or secondary myopathic changes might outweigh motor neuron loss in later stages. The age of treatment initiation might, therefore, be a more relevant determinant of NF level changes or motor function [63] and we are expecting further research on the suitability of NF levels as biomarker for later-onset SMA (see Table 3).
Further molecular markers of neurodegeneration and neuroregeneration
Besides NFs, there are more CSF markers that are commonly associated with neurodegenerative disease, especially tau proteins and ß-amyloid peptides (Aß42 and Aß40). Both have been briefly studied in patients with SMA.
Tau protein is a microtubule-associated protein in the neuronal axons that promotes microtubule assembly and stability [72]. The presence of its phosphorylated form (pTau) is associated with aggregation and microtubule dysfunction [73]. Winter et al. found increased baseline CSF pTau values in an infant with SMA type I that decreased during nusinersen therapy [74]. These data are further supported by Johannsen et al., who replicated increased baseline pTau levels in all pediatric SMA subtypes that decreased under nusinersen [75] and by Walter et al. who reported decreased pTau levels in adults with type 3 under nusinersen [76].ß-Amyloid peptides, particularly Aß42, are assumed to play a major role in neurodegenerative diseases like Alzheimer’s disease, possibly through dysregulation of synaptic activity [77] or axonal degeneration [78]. Aß42 was not elevated in a small cohort of adult SMA patients type 2 and 3 but increased under nusinersen treatment [79] whereas other studies show stable levels of Aß42 and Aß40 under nusinersen [76].
Cathepsin D is a lysosomal aspartyl protease that is expressed in the CNS as well as skeletal and cardiac muscle and is involved in protein degradation [80]. It is believed to play a role in neurodegenerative disorders like ALS [81], Parkinson’s diseases [82] or Alzheimer’s disease [83, 84]. In patients with SMA, CSF cathepsin D levels decreased under nusinersen treatment, particularly in therapy responders, possibly due to a decreased need for protein degradation [85]. The decrease of cathepsin D was significantly correlated to a decrease in plasma NFL levels in patients aged > 12 months at the start of nusinersen treatment. As plasma NFL is a predictor of motor function achievement in children with SMA type 1 (see section on NFL), combined analyses of plasma NFL and cathepsin D might hold a prognostic potential. Cathepsin D was identified using untargeted CSF proteomic analyses, meaning the separation, identification, and quantification of the entire protein complement of the CSF. Using mass spectrometry-based unsupervised proteomic profiling in nusinersen-treated adult SMA patients, Kessler et al. identified two CSF protein clusters that differed in patient age and expression of proteins related to neurodegeneration and neuroregeneration [86]. Similarly to proteomic profiling, metabolic profiling describes the analyses of low-molecular-weight chemicals (< 1 kDa). Metabolic profiling of SMA urine samples provided specific identifiers of SMA compared to controls and was able to distinguish patients with different disease severities. First analyses even suggested the possibility to detect pre-symptomatic patients due to specific fingerprints [87]. Future untargeted analyses using highly sensitive proteomic or metabolomic profiling technologies might provide a deeper insight into SMA pathologies.
Taken together with the evidence on NFs, it is likely that neurodegenerative markers in general might reflect treatment response in SMA patients, but more data derived from bigger cohorts are needed to prove this hypothesis for tau protein, ß-amyloid peptides, and cathepsin D, and possibly other molecules not yet identified until now (see Table 4).
Limitations of neurodegenerative biomarkers
While markers of neurodegeneration seem promising at early stages of the disease and rapidly progressing subtypes, motor pool exhaustion might negatively affect their meaningfulness in advanced stages of the disease. There are no conclusive data on other markers than NFs yet and more investigations are warranted.
Glial biomarkers
An estimated 50% of cells in the human brain is constituted by glia cells, playing a crucial role in many neurodegenerative diseases.
Although the field is relatively unexplored in SMA, there is growing evidence for glia involvement in the course of the disease. Main mechanisms include increased neuroinflammation, synaptic dysregulation, and aberrant immune system activity [88]. Specifically, astrocytes have been shown to influence SMA phenotypes with therapeutically increased SMN levels in astrocytes leading to improved survival and astrogliosis being more prominent in end stage phenotypes [89]. Glial fibrillary acidic protein (GFAP) is an indicator of astroglial activity. In SMA, absolute GFAP levels did not differ from healthy controls in patients with SMA type 2 and 3, possibly due to advanced loss of motor neurons [62, 66]. When corrected to muscle mass, GFAP distinguished strongly between SMA subtypes. It might, therefore, be a candidate as complementary pharmacodynamic biomarker, reporting biological activity on non-neuronal tissue.
Chitotriosidase 1 (CHIT1) is a human endochitinase that is believed to play a role in immune system response [90] and is increased in serum and CSF in various neurodegenerative diseases such as Alzheimer’s disease or ALS [91, 92] as a marker of neuroinflammation. A recent study found elevated CSF CHIT1 levels in SMA patients that did not correlate with disease severity (SMA type, SMN copy number) or duration [93]. CHIT1 does not seem suitable to reflect disease severity, but indicates a role of neuroinflammation in the disease. Although microglial activity decreased in animal models of SMA during ASO-treatment, this observation could not be translated to treated humans [94]. In contrast, CHIT1 levels increased in response to treatment with nusinersen, independent of change in motor function [93]. This observation was supported by an independent study [95]. Taken together with observations of unknown macrophage inclusions during nusinersen therapy [96], CHIT might serve as a safety biomarker for off-target activation of innate immunity treatment but did not show pharmacodynamic potential in case of ASO treatment.
Chitinase-3-like protein 1 (CHI3L1) or YKL-40 is a chitinase that is expressed in astrocytes in neuroinflammation and is, thus, discussed as a marker of astroglial activity [97, 98]. Children with SMA type 1 showed elevated YKL-40 levels [99]. Under therapy, a decrease of YKL-40 levels was associated with improved motor function in patients with SMA type 2 and 3 [95].
S100B is a calcium-binding protein that is mainly found in glial cells and supports cell survival [100]. It is a marker of glial cell death and has mainly been studied in traumatic brain injuries [101], but its overexpression has also been related to active neuronal distress in neurodegenerative disorders like Alzheimer’s disease or ALS [102]. In SMA, S100B was slightly elevated in 1 out of 11patients in serum and CSF [67]. More data are warranted.
Although data on glial biomarkers in SMA are scarce, some of them might be valuable as diagnostic and pharmacodynamic biomarkers, particularly as they might reflect neuroinflammation. The relevance might be higher in more rapidly progressive SMA subtypes (see Table 5).
Limitations of glial markers
Despite some promising insights in glial pathology in SMA, the existing data do not allow a conclusive routine exertion of glial biomarkers in clinical SMA management yet.
Skeletal muscle biomarkers
SMN-P is an ubiquitously expressed protein and, as a consequence, disturbances in multiple peripheral organs have been described in the past years. Schreml et al. found abnormalities in intestine, heart, lung, and skeletal muscle vasculature in SMA mice [103] and in humans, there are numerous reports on cardiac and autonomous defects (for example, see [104–106]) as well as liver and metabolic disorders (for an overview, see [107]). Accordingly, SMA has been considered to be a multi-systemic disease [108].
Regarding the skeletal muscle, there is growing evidence that SMN depletion leads to aberrant muscle and NMJ development in SMA mice [109–113] and aberrant muscle structure and function in human SMA patients have been confirmed (see chapter on electrophysiological biomarkers and [103, 108, 114–116]).
Skeletal muscle regulates synaptic activity and axonal function of motor neurons and provides trophic support [117]. Although SMA is primarily a motor neuron disorder, secondary skeletal muscle atrophy and myopathy, developmental alterations of the postsynaptic motor endplate and neurodegeneration of other extra-motor tissues have been well described.
Given this muscular involvement in the pathogenesis and clinical features in SMA, skeletal muscle laboratory parameters have recently become of interest.
Creatinine and creatine kinase
Creatine and the creatine kinase (CK) play an important regulatory role in the energy metabolism in cells with high energy demand by ensuring restoration of adenosine triphosphate levels [118]. While there are small concentrations of creatine and CK in cardiac and smooth muscle, brain, and other tissues, more than 90% of creatine are stored in the skeletal muscle [119]. The creatine metabolism, therefore, is essential for muscle function and integrity. Creatinine (Crn) is a metabolite from skeletal muscle creatine metabolism and the measurable parameter of this process. Research in other neurodegenerative diseases has shown decreased Crn levels and increased CK levels in spinal and bulbar muscular atrophy (SBMA, [120, 121]) and ALS [122, 123]. Crn is generally considered a marker of muscle mass and CK a marker of muscle damage.
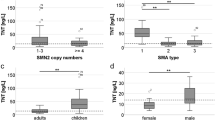
Similarly to SBMA, two studies report increased CK levels and decreased Crn levels in SMA patients compared to healthy controls, with Crn levels able to distinguish clearly between SMA subtypes in children and adults [124, 125]. They were further related to motor function and denervation as measured with CMAP and MUNE. When corrected for weight, height, and age, baseline CK und Crn levels in treatment-naïve patients differed between responders and non-responders to nusinersen and under treatment, CK decreased and Crn increased, reflecting reduced muscle wasting and improved muscle energy metabolism [125]. Crn is detectable in urine samples, and pilot studies report significant differences between SMA patients and healthy controls [126]. Whether or not Crn might serve as a prognostic, predictive or monitoring biomarker in urine is still to be investigated. The study has a short observation period, in which no changes from baseline were observed [126]. A non-invasive way of Crn assessment is, however, intriguing as blood sample collection can be difficult in some SMA patients. Although data are limited, Crn and CK are promising candidate biomarkers for disease progression with and without therapy in SMA patients. As oral Crn supplementation can increase muscular Crn content and thereby possibly improve muscle function [35], therapeutic effects of Crn have been studied in numerous neurodegenerative disorders and myopathies [127, 128]. Wong et al. reported no significant improvement of motor function, muscle strength or quality of life in children with SMA after 6 months of oral Crn [129]. As this is to the best of our knowledge, the only study on oral Crn in SMA patients, future research including larger cohorts and different dosages should be performed (see Table 6).
Other potential skeletal muscle biomarkers
Given the fact that Crn and CK are promising biomarkers for monitoring disease progression and diagnostic purposes in patients with SMA, and that the skeletal muscle is more and more evolving as a diagnostic and therapeutic target, we consider investigating other potential skeletal muscle biomarkers as important and meaningful in the quest for reliable SMA biomarkers.
Myoglobin
Myoglobin (Myo) is a cytoplasmatic hemoprotein that is solely expressed in cardiac myocytes and oxidative skeletal muscle fibers. It is an important oxygen storage that can release oxygen in case of hypoxia or anoxia, buffer muscular oxygen concentrations. And facilitate oxygen diffusion in activated muscle with the purpose of providing equivocal oxygen levels in any degree of muscle activity [130]. Similar to CK, Myo is released in case of muscle damage or impaired integrity of muscle cell membrane and might serve as a marker for muscle wasting and aberrant muscle metabolism in motor neuron diseases. In SBMA, Myo was significantly elevated compared to ALS patients and related with disease progression [131]. To the best of our knowledge, there are no studies on Myo in SMA yet. However, based on the above-mentioned findings, we propose Myo as a potential SMA biomarker (see Table 7).
Troponin T
Troponins are involved in the calcium regulation in striated muscle and essential for muscle structure and function [132]. There are several troponin isoforms of which Troponin I (TNI) and Troponin T (TNT) are generally considered highly specific for cardiac muscle [133]. However, there is an increasing number of non-cardiac diseases that are associated with TNT elevation, particularly neurodegenerative disorders [134]. A secondary cardiac involvement has previously been proposed. In a recent study in ALS, Castro-Gomez et al. found elevated TNT levels in ALS patients without TNI elevation or clinical signs of cardiac involvement, and thus proposed an extracardiac origin of TNT with TNT serving as a biomarker for lower motor neuron affection [135]. Although SMA and ALS have fundamentally different pathogenesis, they do partially share identical phenotype and pathomechanisms [136]. Changes of troponin isoform expression in muscles of SMA patients are described [137]. An increased understanding of the role of TNT in SMA is especially important as novel troponin activating therapies are in the pipeline [27] (see Table 8).
Limitation of skeletal muscle biomarkers
Skeletal muscle biomarkers comprise markers of muscle destruction and integrity, that can add valuable information in the therapeutic management of SMA when combined. They are, however, dependent on individual factors such as body and muscle mass, renal function, and (cardiac) comorbidities and must, therefore, be interpreted carefully.
Biomarkers of physiological properties
Electrophysiology Electrophysiological measurements can monitor the functional status of the motor unit pool and are, therefore, extremely important in the diagnostic process and monitoring of disease progression in motor neuron disorders. compound muscle action potential (CMAP), motor unit number estimation (MUNE), and motor unit number index (MUNIX) have evolved as the most reliable measures.
CMAP
Reduction of CMAP amplitudes indicate a reduction of motor units supplying a particular muscle or group of muscles [31]. Arnold et al. found significantly reduced CMAP in 2-week-old SMA mice, that could be restored under SMN-increasing therapy [138]. In humans, CMAP of the ulnar nerve was reduced in SMA patients and correlated with SMA type, age, and SMN2 copy number [139–141]. It improved in children treated with onasemnogene abeparvovec [142] and nusinersen [143] and stayed stable during nusinersen treatment [144]. Patients with a faster post-treatment ulnar CMAP-increase tended to have better functional outcome [141]. These data suggest that CMAP is a reliable marker of disease progression under therapy in SMA children and is especially suitable for children as it does not require cooperation of the patient. It might further be an early indicator of the degree of therapy response in children with SMA and underlines the importance for an early therapy start in patients with SMA, regardless of the clinical subtype. However, further research is needed as some data suggest that CMAP might not adequately reflect motor neuron loss in only lightly affected muscle groups [145] (see Table 9).
MUNE
While CMAP measures the electrical output of a muscle, MUNE estimates the number of innervating motor neurons [31]. Similarly to CMAP, it is reduced in patients with SMA type 1 and 2, correlated with SMA type, age, and SMN2 copy number [140, 141] and improved in children treated with onasemnogene abeparvovec [142] and nusinersen [143]. In adult SMA type 3 patients, MUNE was decreased compared to controls but did not change under nusinersen [146]. MUNE holds great potential as a biomarker for diagnostic measures and also promising value for prognostic and pharmacodynamic purpose. However, further research is needed as follow-up data on children with SMA type 3 show decreasing long-term MUNE measures, despite therapy [144] and data in adult SMA patients are scarce (see Table 10).
MUNIX
Assessing the motor unit number index (MUNIX) is a non-invasive technique that estimates the number of functional motor units innervating a particular muscle or group of muscles [147]. It has been well established in ALS [147, 148] as a reliable and valid marker for motor unit loss. Recent studies in patients with SMA showed relevant correlations of MUNIX and motor function and disease progression in both adults and children [139, 145, 149, 150]. MUNIX further detects disease-specific patterns of motor unit loss, allowing a precise distinction of SMA versus ALS patients [139]. Summed up, MUNIX seems to be a suitable biomarker for monitoring disease progression in the natural course of the disease and possibly under disease-modifying therapies (see Table 11).
Other electrophysiological markers
MUSIX
Motor unit size index (MUSIX) can be calculated with MUNIX and CMAP amplitudes and provides information on the size of motor units of a particular muscle or muscle groups [151]. They show increased values in SMA patients, suggesting re-innervation [145]. Investigations of the relevance of MUSIX as a biomarker in SMA are scarce, but MUSIX might add valuable information for the monitoring of disease progression with and without therapy. However, more research needs to be done (see Table 12).
EIM
Electrical impedance myography (EIM) is a relatively new, easy, and painless technique which provides information on the impedance characteristics of the underlying muscle. It showed a good correlation with muscle strengths in children with SMA type 2 and 3 [152] and might be able to discriminate between healthy subjects and those with SMA [153]. Animal models further show correlation to SMN protein levels and CMAP data [154] (see Table 13).
Repetitive nerve stimulation
Animal models have suggested early disturbances of the neuromuscular junction (NMJ) in SMA pathology [155–157]. It is unclear whether or not SMN-increasing therapy has beneficial effects on the NMJ integrity or function. Arnold et al. used repetitive nerve stimulation to detect NMJ transmission defects in adult SMA patients [158]. The defects were not corrected after 14 months of nusinersen treatment and correlated negatively with motor function. Although data on repetitive nerve stimulation and NMJ deficits in SMA in general are rare, studying the NMJ in SMA appears to be a promising field for establishing new therapeutic approaches and possibly also biomarkers, especially in the context of new muscle-targeted therapeutic approaches. In a phase 2 study, Bonanno et al. found improved motor function in ambulatory SMA type 3 patients treated with amifampridine, which improves NMJ transmission [29] (see Table 14).
Limitations to electrophysiological biomarkers
The above-mentioned electrophysiological methods partly reflect the integrity and function of the motor unit in SMA patients, both adults and children suggesting a high biomarker potential. However, there are some considerable limitations: Some of the techniques are painful (e.g., CMAP, MUNE, MUNIX) and/or require the cooperation of the patient (e.g., MUNIX, spirometry) and might, thus, not be suitable for infants and children. While spirometry shows promising diagnostic, prognostic, and monitoring properties and is well established in the clinical routine, the electrophysiological techniques might be more difficult to be implemented routinely as they are resource and time consuming, exhibit inter-rater variability, and need intensive training.
Functional biomarkers
Dynamometry
Muscle strength of SMA patients is usually assessed using the Medical Research Council (MRC) scale that ranges from 0 (no muscle contraction at all) to 5 (normal strength) [159]. However, the scale requires extensive training, lacks sensitivity in very weak muscles and displays high intra- and inter-rater variability [160–162]. Merlini et al. showed reliable measurements of muscle strength in SMA with a hand-held dynamometer [163] and linked muscle strength to motor function [164]. Under nusinersen, handgrip strength significantly improved in patients with SMA type 3 and 4 and correlated with motor function change in the RULM [165]. Seferian et al. further investigated grip and pinch strength in patients with SMA type 2 and 3 and found significantly lower muscle strength in type 2 patients [166]. Interestingly, both grip and pinch strength increased in young non-ambulatory patients (< 14 years of age) but declined in older patients [166]. A possible explanation is an inability of growth to compensate for strength loss in older patients. Dynamometry is a non-invasive tool that seems to be suitable for the implementation in clinical routine to assess and monitor motor function in SMA patients (see Table 15).
Spirometry
Respiratory dysfunction is a crucial cause of death in neuromuscular diseases including SMA, particularly in more severely affected patients [167]. Pulmonary function usually declines throughout the natural cause of the disease, often leading to the need for ventilatory support or tracheotomy [168]. Both the forced expiratory volume in 1 s (FEV1) and forced vital capacity (FVC) differ between SMA subtypes and decline over time [169]. Under nusinersen, multiple studies report a stable or even improved pulmonary function and an higher likelihood of event-free survival (e.g., free from tracheotomy or ventilation assistance) in SMA types 1 and 2 [170–172] whereas a few do not [173, 174] (see Table 16).
Imaging-based biomarkers
Quantitative MR imaging
Muscle
Quantitative magnetic resonance imaging (qMRI) is a device-based tool for muscle physiology assessment.qMRI of muscles has been performed in several neuromuscular diseases, for example Charcot–Marie–Tooth disease, inclusion body myositis [175] or Duchenne muscular dystrophy [176]. Especially in Charcot–Marie–Tooth disease, it has proven to correlate with motor function scales and disease severity at baseline and longitudinally.
In patients with SMA, Bonati et al. demonstrated a reduced muscle mass and density of the thigh muscle with an increased infiltration by fatty tissue. Similarly, Wadman et al. reported fatty degeneration of mouth opening muscles and a sign of bulbar dysfunction in SMA [177] and fatty degeneration of muscles of upper and lower extremity muscles are well described [178–181]. Further cross-sectional evaluations of qMRI indices were able to clearly distinguish between SMA patients and healthy participants but it remains unclear if a stratification among SMA types is feasible [46]. Muscle volume and other qMRI markers in SMA patients correlated strongly with impairment of motor function in several studies; however, these markers did not seem to have a prognostic potential [46, 180, 178–183]. qMRI measures were associated with decrease of motor function in a recent study. However, no changes were observed during 6 months [181, 185] or 14 months [107] of nusinersen treatment whereas motor function measured with motor scores increased [107], arguing for a limited monitoring biomarker potential. In treatment-naïve patients, Otto et al. reported a slow disease progression in qMRI despite sustained motor function and muscle strength [179]. These somewhat contradictory findings leave room for further investigation of the utility of qMRI as a biomarker in SMA, especially as a monitoring biomarker. As of today, qMRI is a non-invasive and well-tolerable method to add valuable information on morphological characteristics of the effector tissue muscle, unaffected by influencing factors such as patient’s fatigue or daily fluctuations [46]. It is, however, relatively expensive and can currently not be used as a stand-alone biomarker. Nonetheless, qMRI will be of interest for further investigations, especially in the context of new muscle-targeting drugs (see Table 17).
Nerve
Quantitative MR neurography (qMRN) is a 3 Tesla MRI-based technique that enables high-resolution visualization of both the peripheral nervous system and the musculature in one step. One important strength of qMRN is its ability to assess even the most proximal nerve segments, i.e., spinal nerves and plexus, that are hardly accessible through traditional electrophysiologic methods but are of special interest in SMA [186]. qMRN has proven to detect PNS lesions with high sensitivity in a wide variety of PNS-affecting diseases [187, 188], Similarly, qMRN detected and quantified PNS lesions in therapy-naïve patients with SMA types 2, 3a, and 3b in vivo [189]. This work also defined qMRN parameters (T2 relaxation time, proton spin density, cross-sectional area) that might serve as imaging biomarkers in SMA to indicate early microstructural nerve tissue changes. One particular parameter, the magnetization transfer ratio, differed between SMA type 3 patients and healthy controls and correlated with clinical scores [190]. Further research is needed to determine the value of these qMRN markers in evaluating response to SMA treatments and diagnostic procedures [189, 190].
Central nervous quantitative MR imaging has exposed cervical spinal cord atrophy in treatment-naïve adult SMA patients compared to healthy controls [191] and these changes might be based on gray matter atrophy [192, 193]. A longitudinal pilot study with three adult SMA patients found stable gray matter volumes in two out of three patients under nusinersen and increasing volumes in the third patient [193]. Thus, spinal cord and particular gray matter volume are candidate diagnostic, response and monitoring biomarkers. However, a lot more research in larger cohorts is warranted (see Table 18).
Ultrasonography
Muscle
Muscle ultrasonography is a non-invasive and relatively inexpensive tool in the diagnostics of neuromuscular disorders. It has proven its worth in different diseases involving muscle atrophy, for example Duchenne muscular dystrophy [194–196]. Different diseases show different ultrasonography changes with SMA showing an inhomogeneous increase of echo intensity with severe atrophy of the muscle [195]. A small pilot study reported feasibility of discrimination between healthy controls and SMA patients [197], but this study was limited by a small sample size and many possible confounding factors (e.g., technical factors involving the ultrasonography machine and high inter- and intra-rater variability) still limit the usability of this method (see Table 19).
Nerve
Similar to muscle ultrasonography, nerve ultrasonography is a non-invasive and relatively inexpensive diagnostic tool. To this day, there is one small study on ultra-high-frequency nerve ultrasonography in patients with SMA [199]. The authors investigated nerve area and fascicle density and number in the median nerve of one patient with each SMA type 1, 2, and 3 in comparison to healthy controls. While there were no differences between controls and SMA type 2 and 3, the patient with SMA type 1 showed a reduced fascicle number, possibly related to the rapid clinical progress in this subtype. The study is, however, too small for conclusive information (see Table 20).
Diaphragm
Diaphragmatic ultrasound has found diaphragmatic dysfunction in adult SMA patients that correlates with the FEV1 and FVC [200–202]. Pathological findings mainly include reduced contractility but not atrophy with differential data for adults and children (compare [202]). It is an easy and non-invasive tool for the assessment of pulmonary function, that does not require the patient’s compliance and is, thus, also suitable for children. To this day, the clinical benefit over spirometric parameters remains unclear (see Table 21.
Dual-energy X-ray absorptiometry
Measuring body composition (BC) with dual-energy X-ray absorptiometry has been used for monitoring disease severity and progression in patients with neuromuscular disorders [203]. Baranello et al. investigated relevant BC parameters like body weight, supine lengths, body mass index, fat and lean mass as well as composite measures consistent of bone mineral content and lean mass (“FFM”) in correlation to motor function [204]. The study revealed that a good body composition is associated with good motor function, which underlines the importance of monitoring the nutritional status of SMA patients. Furthermore, lean body mass might be a co-factor when interpreting molecular biomarkers of muscle integrity [124]. The authors themselves, however, recognize that further research should be undertaken considering relatively low correlations (see Table 22).
Limitations of imaging-based biomarkers
Imaging-based biomarkers reflect the current muscle and nerve structure in SMA patients. However, they have not been proven to be of use in monitoring disease courses in SMA with or without treatments (monitoring biomarker). Promising data come from central nervous quantitative MRI imaging. The techniques are costly and standardized protocols are not yet widely available. To date, their routine clinical use remains limited.
Digital biomarkers
Electronics and digital devices have long become a substantial part of our daily private and professional life. In SMA, they facilitate participation and are an important part of the patient’s autonomy. It is only consistent to investigate the use of digital technology in the SMA management. Two studies have investigated the suitability of different movement sensors for the assessment of upper limb function in SMA patients. Chen et al. used the Microsoft Kinect sensor to record movements of patients with SMA type 3 and compared them to healthy controls [205]. Although the sensor distinguished between controls and patients at later stages of the disease, it was not (yet) able to distinguish early-stage differences. Chabanon et al. used the motor sensor ActiMyo to measure upper limb function and found that numerous parameters correlated to motor function as measured with the common scales and differed between SMA subtypes [206]. More app-based tools are currently under investigation. One example is the Konectom app that includes the assessment of upper and lower limb motor function [207].
Overall, digital outcome assessments hold the strong potential to monitor motor function in SMA patients in the future, but more research is warranted. They are particularly interesting as they might provide valuable insight on motor function in the patients’ everyday life and fluctuations during the day.
Classification of digital biomarkers is challenging. They measure physiological functions and could, therefore, be listed under biomarkers of physiological properties. We did, however, distinguish them from conventional (electro-)physiological measures due to the novelty of the used technology and appliances and the fact that they can be used remotely outside the clinic (see Table 23).
Conclusion
The interest in biomarkers for SMA has grown over the past decade, alongside with a change of research focus from basic to clinical research. Driver of this paradigm shift has not at least been the development of new disease-modifying therapies and a concomitant need for parameters that help clinicians navigate through the therapeutic process.
Research on suitable biomarkers has been extensive and broad, but a lot of work still remains to be done. Many multimodal potential biomarkers for diagnostic, prognostic, and predictive purposes have been identified; however, none of them have (yet) emerged as one single overarching marker.
Circulating SMN-related biomarkers (SMN protein, particularly SMN2 copy number) have a good diagnostic value and hold the potential to monitor therapy response in the future. Markers of neurodegeneration such as NFs have proven to be good prognostic markers and monitor therapy response in SMA patients. Skeletal muscle-associated plasma proteins (Crn, CK) can predict treatment response and further accurately monitor disease progression and motor function. Similar routine parameters (TropT and Myo) show promising potential in other neurodegenerative diseases and could be of additional predictive value to the monitoring of patients with SMA; however, pending investigations need to be done. Electrophysiological parameters such as CMAP, MUNE, and MUNIX developed as trustworthy measures of motor function in patients with SMA during the course of the disease and allow prediction of treatment effect. Imaging-based techniques involving MRI und ultrasonography can distinguish between healthy subjects and SMA patients and provide insight in morphological properties of muscle and nerve during disease course; however, difficulties in the clinical routine are expected due to cost in relation to other measures, inter- and intra-rater variability, and limited ability. Digital biomarkers can be easily implemented in the patient’s daily routine and can assess motor function under real-world conditions. As telemedicine and e-health are progressively established in health care, the importance of digital biomarkers is likely to grow in the next years.
Different biomarkers are needed for different purposes. As laid out above, none of the markers can sufficiently meet all the expected criteria. A combination of different biomarkers with clinical assessments at different times in the course of the disease appears to be the most comprehensive solution at the time. Besides the obligatory genetic testing and clinical assessment, a possible biomarker scheme could include baseline acquisition of SMN2 copy number, electrophysiology (CMAP), plasma protein levels of SMN protein, NF, Crn, CK, and CSF NF protein levels with regular follow-ups on fluid and digital biomarkers and annual or biennial follow-ups on the electrophysiological markers (see Table 24).
Data availability
There are no data to disclose as this work is a narrative review.
References
So BR, Zhang Z, Dreyfuss G (2017) Chapter 6—the function of survival motor neuron complex and its role in spinal muscular atrophy pathogenesis. In: Sumner CJ, Paushkin S, Ko C-P (eds) Spinal muscular atrophy. Academic Press, pp 99–111
Kolb SJ, Kissel JT (2015) Spinal muscular atrophy. Neurol Clin 33:831–846
Lorson CL, Hahnen E, Androphy EJ, Wirth B (1999) A single nucleotide in the SMN gene regulates splicing and is responsible for spinal muscular atrophy. Proc Natl Acad Sci U S A 96:6307–6311
Campbell L, Potter A, Ignatius J, Dubowitz V, Davies K (1997) Genomic variation and gene conversion in spinal muscular atrophy: implications for disease process and clinical phenotype. Am J Hum Genet 61:40–50
Mailman MD, Heinz JW, Papp AC, Snyder PJ, Sedra MS, Wirth B, Burghes AH, Prior TW (2002) Molecular analysis of spinal muscular atrophy and modification of the phenotype by SMN2. Genet Med 4:20–26
Wirth B, Herz ME, Wetter A, Moskau S, Hahnen E, Rudnik-Schöneborn S, Wienker TF, Zerres K (1999) Quantitative analysis of survival motor neuron copies: identification of subtle SMN1 mutations in patients with spinal muscular atrophy, genotype-phenotype correlation, and implications for genetic counseling. Am J Hum Genet 64(5):1340–1356
Day JW, Finkel RS, Chiriboga CA, Connolly AM, Crawford TO, Darras BT, Iannaccone ST, Kuntz NL, Peña LDM, Shieh PB, Smith EC, Kwon JM, Zaidman CM, Schultz M, Feltner DE, Tauscher-Wisniewski S, Ouyang H, Chand DH, Sproule DM, Macek TA, Mendell JR (2021) Onasemnogene abeparvovec gene therapy for symptomatic infantile-onset spinal muscular atrophy in patients with two copies of SMN2 (STR1VE): an open-label, single-arm, multicentre, phase 3 trial. The Lancet Neurology 20:284–293
Mendell JR, Al-Zaidy S, Shell R, Arnold WD, Rodino-Klapac LR, Prior TW, Lowes L, Alfano L, Berry K, Church K, Kissel JT, Nagendran S, L’Italien J, Sproule DM, Wells C, Cardenas JA, Heitzer MD, Kaspar A, Corcoran S, Braun L, Likhite S, Miranda C, Meyer K, Foust KD, Burghes AHM, Kaspar BK (2017) Single-dose gene-replacement therapy for spinal muscular atrophy. N Engl J Med 377:1713–1722
Mendell JR, Al-Zaidy SA, Lehman KJ, McColly M, Lowes LP, Alfano LN, Reash NF, Iammarino MA, Church KR, Kleyn A, Meriggioli MN, Shell R (2021) Five-year extension results of the phase 1 START trial of onasemnogene abeparvovec in spinal muscular atrophy. JAMA Neurol 78:834–841
Acsadi G, Crawford TO, Müller-Felber W, Shieh PB, Richardson R, Natarajan N, Castro D, Ramirez-Schrempp D, Gambino G, Sun P, Farwell W (2021) Safety and efficacy of nusinersen in spinal muscular atrophy: The EMBRACE study. Muscle Nerve 63:668–677
Claborn MK, Stevens DL, Walker CK, Gildon BL (2019) Nusinersen: a treatment for spinal muscular atrophy. Ann Pharmacother 53:61–69
De Vivo DC, Bertini E, Swoboda KJ, Hwu WL, Crawford TO, Finkel RS, Kirschner J, Kuntz NL, Parsons JA, Ryan MM, Butterfield RJ, Topaloglu H, Ben-Omran T, Sansone VA, Jong YJ, Shu F, Staropoli JF, Kerr D, Sandrock AW, Stebbins C, Petrillo M, Braley G, Johnson K, Foster R, Gheuens S, Bhan I, Reyna SP, Fradette S, Farwell W, Group NS (2019) Nusinersen initiated in infants during the presymptomatic stage of spinal muscular atrophy: Interim efficacy and safety results from the Phase 2 NURTURE study. Neuromuscul Disord 29:842–856
Finkel RS, Mercuri E, Darras BT, Connolly AM, Kuntz NL, Kirschner J, Chiriboga CA, Saito K, Servais L, Tizzano E, Topaloglu H, Tulinius M, Montes J, Glanzman AM, Bishop K, Zhong ZJ, Gheuens S, Bennett CF, Schneider E, Farwell W, De Vivo DC (2017) Nusinersen versus Sham control in infantile-onset spinal muscular atrophy. N Engl J Med 377:1723–1732
Mercuri E, Darras BT, Chiriboga CA, Day JW, Campbell C, Connolly AM, Iannaccone ST, Kirschner J, Kuntz NL, Saito K, Shieh PB, Tulinius M, Mazzone ES, Montes J, Bishop KM, Yang Q, Foster R, Gheuens S, Bennett CF, Farwell W, Schneider E, De Vivo DC, Finkel RS (2018) Nusinersen versus sham control in later-onset spinal muscular atrophy. N Engl J Med 378:625–635
Baranello G, Darras BT, Day JW, Deconinck N, Klein A, Masson R, Mercuri E, Rose K, El-Khairi M, Gerber M, Gorni K, Khwaja O, Kletzl H, Scalco RS, Seabrook T, Fontoura P, Servais L (2021) Risdiplam in type 1 spinal muscular atrophy. N Engl J Med 384:915–923
Darras BT, Masson R, Mazurkiewicz-Bełdzińska M, Rose K, Xiong H, Zanoteli E, Baranello G, Bruno C, Vlodavets D, Wang Y, El-Khairi M, Gerber M, Gorni K, Khwaja O, Kletzl H, Scalco RS, Fontoura P, Servais L (2021) Risdiplam-Treated Infants with Type 1 Spinal Muscular Atrophy versus Historical Controls. N Engl J Med 385:427–435
Kakazu J, Walker NL, Babin KC, Trettin KA, Lee C, Sutker PB, Kaye AM, Kaye AD (2021) Risdiplam for the use of spinal muscular atrophy. Orthop Rev 13:25579
Mercuri E, Baranello G, Boespflug-Tanguy O, De Waele L, Goemans N, Kirschner J, Masson R, Mazzone ES, Pechmann A, Pera MC, Vuillerot C, Bader-Weder S, Gerber M, Gorni K, Hoffart J, Kletzl H, Martin C, McIver T, Scalco RS, Yeung WY, Servais L (2022) Risdiplam in types 2 and 3 spinal muscular atrophy: a randomised, placebo-controlled, dose-finding trial followed by 24 months of treatment. Eur J Neurol. https://doi.org/10.1111/ene.15499
Singh RN, Ottesen EW, Singh NN (2020) The first orally deliverable small molecule for the treatment of spinal muscular atrophy. Neurosci Insights 15:2633105520973985
Erdos J, Wild C (2022) Mid- and long-term (at least 12 months) follow-up of patients with spinal muscular atrophy (SMA) treated with nusinersen, onasemnogene abeparvovec, risdiplam or combination therapies: a systematic review of real-world study data. Eur J Paediatr Neurol EJPN 39:1–10
Messina S, Sframeli M (2020) New Treatments in Spinal Muscular Atrophy: Positive Results and New Challenges. J Clin Med 9(7):2222. https://doi.org/10.3390/jcm9072222
Nicolau S, Waldrop MA, Connolly AM, Mendell JR (2021) Spinal muscular atrophy. Semin Pediatr Neurol 37:100878
Crawford T, Darras B, Day J, Song G, Nomikos G, Place A, Barrett D, Bilic S, O’Neil J, Kertesz N, Cote S, Patel J, Chyung Y (2022) Apitegromab in spinal muscular atrophy (SMA): an analysis of multiple efficacy endpoints in the TOPAZ trial (P15–500.5). Neurology 98:1859
Pera MC, Coratti G, Forcina N, Mazzone ES, Scoto M, Montes J, Pasternak A, Mayhew A, Messina S, Sframeli M, Main M, Lofra RM, Duong T, Ramsey D, Dunaway S, Salazar R, Fanelli L, Civitello M, de Sanctis R, Antonaci L, Lapenta L, Lucibello S, Pane M, Day J, Darras BT, De Vivo DC, Muntoni F, Finkel R, Mercuri E (2017) Content validity and clinical meaningfulness of the HFMSE in spinal muscular atrophy. BMC Neurol 17:39
Bezier C, Hashemi PN, Cottin S, Lafont R, Veillet S, Charbonnier F, Dilda P, Latil M, Biondi O (2022) FP1.0 Combination of BIO101 with antisense oligonucleotide therapy demonstrates synergistic beneficial effects in severe SMA-like mice. Neuromusc Disord 32:S58
Hwee DT, Kennedy AR, Hartman JJ, Ryans J, Durham N, Malik FI, Jasper JR (2015) The small-molecule fast skeletal troponin activator, CK-2127107, improves exercise tolerance in a rat model of heart failure. J Pharmacol Exp Ther 353:159–168
Rudnicki SA, Andrews JA, Duong T, Cockroft BM, Malik FI, Meng L, Wei J, Wolff AA, Genge A, Johnson NE, Tesi-Rocha C, Connolly AM, Darras BT, Felice K, Finkel RS, Shieh PB, Mah JK, Statland J, Campbell C, Habib AA, Kuntz NL, Oskoui M, Day JW (2021) Reldesemtiv in patients with spinal muscular atrophy: a phase 2 hypothesis-generating study. Neurotherapeutics J Am Soc Exp NeuroTherap 18:1127–1136
Maddison P, Newsom-Davis J, Mills KR (1998) Distribution of electrophysiological abnormality in Lambert-Eaton myasthenic syndrome. J Neurol Neurosurg Psychiatry 65:213–217
Bonanno S, Giossi R, Zanin R, Porcelli V, Iannacone C, Baranello G, Ingenito G, Iyadurai S, Stevic Z, Peric S, Maggi L (2022) Amifampridine safety and efficacy in spinal muscular atrophy ambulatory patients: a randomized, placebo-controlled, crossover phase 2 trial. J Neurol 269:5858–5867
FDA-NIH Biomarker Working Group (2016) BEST (Biomarkers, EndpointS, and other Tools) Resource. In: Food and Drug Administration (US), Silver Spring (MD) Bethesda (MD)
Pino MG, Rich KA, Kolb SJ (2021) Update on biomarkers in spinal muscular atrophy. Biomark Insights 16:11772719211035644
Navarrete-Opazo A, Garrison S, Waite M (2021) Molecular biomarkers for spinal muscular atrophy. Syst Rev 11:e524–e536
Youn BY, Ko Y, Moon S, Lee J, Ko SG, Kim JY (2021) Digital biomarkers for neuromuscular disorders: a systematic scoping review. Diagnostics (Basel, Switzerland) 11(7):1275. https://doi.org/10.3390/diagnostics11071275
Selleck MJ, Senthil M, Wall NR (2017) Making meaningful clinical use of biomarkers. Biomark Insights 12:1177271917715236
Finkel RS, Crawford TO, Swoboda KJ, Kaufmann P, Juhasz P, Li X, Guo Y, Li RH, Trachtenberg F, Forrest SJ, Kobayashi DT, Chen KS, Joyce CL, Plasterer T, on behalf of the Pilot Study of Biomarkers for Spinal Muscular Atrophy Trial G (2012) Candidate proteins, metabolites and transcripts in the biomarkers for spinal muscular atrophy (BforSMA) clinical study. PLoS ONE 7:e35462
Kobayashi DT, Shi J, Stephen L, Ballard KL, Dewey R, Mapes J, Chung B, McCarthy K, Swoboda KJ, Crawford TO, Li R, Plasterer T, Joyce C, Chung WK, Kaufmann P, Darras BT, Finkel RS, Sproule DM, Martens WB, McDermott MP, De Vivo DC, Walker MG, Chen KS, the Biomarkers for Spinal Muscular Atrophy Study G, the Pediatric Neuromuscular Clinical Research N (2013) SMA-MAP: a plasma protein panel for spinal muscular atrophy. PLoS ONE 8:e60113
Monani UR, Sendtner M, Coovert DD, Parsons DW, Andreassi C, Le TT, Jablonka S, Schrank B, Rossoll W, Prior TW, Morris GE, Burghes AH (2000) The human centromeric survival motor neuron gene (SMN2) rescues embryonic lethality in Smn(-/-) mice and results in a mouse with spinal muscular atrophy. Hum Mol Genet 9:333–339
Tiziano FD, Neri G, Brahe C (2011) Biomarkers in rare disorders: the experience with spinal muscular atrophy. Int J Mol Sci 12:24–38
Battaglia G, Princivalle A, Forti F, Lizier C, Zeviani M (1997) Expression of the SMN gene, the spinal muscular atrophy determining gene, in the mammalian central nervous system. Hum Mol Genet 6:1961–1971
Groen EJN, Perenthaler E, Courtney NL, Jordan CY, Shorrock HK, van der Hoorn D, Huang YT, Murray LM, Viero G, Gillingwater TH (2018) Temporal and tissue-specific variability of SMN protein levels in mouse models of spinal muscular atrophy. Hum Mol Genet 27:2851–2862
La Bella V, Cisterni C, Salaun D, Pettmann B (1998) Survival motor neuron (SMN) protein in rat is expressed as different molecular forms and is developmentally regulated. Eur J Neurosci 10:2913–2923
Alves CRR, Zhang R, Johnstone AJ, Garner R, Eichelberger EJ, Lepez S, Yi V, Stevens V, Poxson R, Schwartz R, Zaworski P, Swoboda KJ (2020) Whole blood survival motor neuron protein levels correlate with severity of denervation in spinal muscular atrophy. Muscle Nerve 62:351–357
Crawford TO, Paushkin SV, Kobayashi DT, Forrest SJ, Joyce CL, Finkel RS, Kaufmann P, Swoboda KJ, Tiziano D, Lomastro R, Li RH, Trachtenberg FL, Plasterer T, Chen KS, on behalf of the Pilot Study of Biomarkers for Spinal Muscular Atrophy Trial G (2012) Evaluation of SMN protein, transcript, and copy number in the biomarkers for spinal muscular atrophy (BforSMA) Clinical Study. PLoS ONE 7:e33572
Nash LA, McFall ER, Perozzo AM, Turner M, Poulin KL, De Repentigny Y, Burns JK, McMillan HJ, Warman Chardon J, Burger D, Kothary R, Parks RJ (2017) Survival motor neuron protein is released from cells in exosomes: a potential biomarker for spinal muscular atrophy. Sci Rep 7:13859
Vezain M, Saugier-Veber P, Melki J, Toutain A, Bieth E, Husson M, Pedespan JM, Viollet L, Penisson-Besnier I, Fehrenbach S, Bou J, Frebourg T, Tosi M (2007) A sensitive assay for measuring SMN mRNA levels in peripheral blood and in muscle samples of patients affected with spinal muscular atrophy. Eur J Hum Genet 15:1054–1062
Bonati U, Holiga Š, Hellbach N, Risterucci C, Bergauer T, Tang W, Hafner P, Thoeni A, Bieri O, Gerlach I, Marquet A, Khwaja O, Sambataro F, Bertolino A, Dukart J, Fischmann A, Fischer D, Czech C (2017) Longitudinal characterization of biomarkers for spinal muscular atrophy. Ann Clin Transl Neurol 4:292–304
Sumner CJ, Kolb SJ, Harmison GG, Jeffries NO, Schadt K, Finkel RS, Dreyfuss G, Fischbeck KH (2006) SMN mRNA and protein levels in peripheral blood: biomarkers for SMA clinical trials. Neurology 66:1067–1073
Czech C, Tang W, Bugawan T, Mano C, Horn C, Iglesias VA, Fröhner S, Zaworski PG, Paushkin S, Chen K, Kremer T (2015) Biomarker for spinal muscular atrophy: expression of SMN in peripheral blood of SMA patients and healthy controls. PLoS ONE 10:e0139950
Renusch SR, Harshman S, Pi H, Workman E, Wehr A, Li X, Prior TW, Elsheikh BH, Swoboda KJ, Simard LR, Kissel JT, Battle D, Parthun MR, Freitas MA, Kolb SJ (2015) Spinal muscular atrophy biomarker measurements from blood samples in a clinical trial of valproic acid in ambulatory adults. J Neuromuscul Dis 2:119–130
Iyer CC, Wang X, Renusch SR, Duque SI, Wehr AM, Mo XM, McGovern VL, Arnold WD, Burghes AH, Kolb SJ (2017) SMN blood levels in a porcine model of spinal muscular atrophy. J Neuromuscul Dis 4:59–66
Ramos DM, d’Ydewalle C, Gabbeta V, Dakka A, Klein SK, Norris DA, Matson J, Taylor SJ, Zaworski PG, Prior TW, Snyder PJ, Valdivia D, Hatem CL, Waters I, Gupte N, Swoboda KJ, Rigo F, Bennett CF, Naryshkin N, Paushkin S, Crawford TO, Sumner CJ (2019) Age-dependent SMN expression in disease-relevant tissue and implications for SMA treatment. J Clin Investig 129:4817–4831
Burlet P, Huber C, Bertrandy S, Ludosky M, Zwaenepoel I, Clermont O, Roume J, Delezoide A, Cartaud J, Munnich A (1998) The distribution of SMN protein complex in human fetal tissues and its alteration in spinal muscular atrophy. Hum Mol Genet 7:1927–1933
Giavazzi A, Setola V, Simonati A, Battaglia G (2006) Neuronal-specific roles of the survival motor neuron protein: evidence from survival motor neuron expression patterns in the developing human central nervous system. J Neuropathol Exp Neurol 65:267–277
Poirier A, Weetall M, Heinig K, Bucheli F, Schoenlein K, Alsenz J, Bassett S, Ullah M, Senn C, Ratni H, Naryshkin N, Paushkin S, Mueller L (2018) Risdiplam distributes and increases SMN protein in both the central nervous system and peripheral organs. Pharmacol Res Perspect 6:e00447
Tiziano FD, Pinto AM, Fiori S, Lomastro R, Messina S, Bruno C, Pini A, Pane M, D’Amico A, Ghezzo A, Bertini E, Mercuri E, Neri G, Brahe C (2010) SMN transcript levels in leukocytes of SMA patients determined by absolute real-time PCR. Eur J Hum Genet 18:52–58
Wadman RI, Stam M, Jansen MD, van der Weegen Y, Wijngaarde CA, Harschnitz O, Sodaar P, Braun KP, Dooijes D, Lemmink HH, van den Berg LH, van der Pol WL (2016) A comparative study of SMN protein and mRNA in blood and fibroblasts in patients with spinal muscular atrophy and healthy controls. PLoS ONE 11:e0167087
Yuan A, Rao MV, Veeranna, Nixon RA (2017) Neurofilaments and neurofilament proteins in health and disease. Cold Spring Harbor Perspect Biol 9(4):a018309. https://doi.org/10.1101/cshperspect.a018309
Loeffler T, Schilcher I, Flunkert S, Hutter-Paier B (2020) Neurofilament-light chain as biomarker of neurodegenerative and rare diseases with high translational value. Front Neurosci 14:579. https://doi.org/10.3389/fnins.2020.00579
Palermo G, Mazzucchi S, Della Vecchia A, Siciliano G, Bonuccelli U, Azuar C, Ceravolo R, Lista S, Hampel H, Baldacci F (2020) Different clinical contexts of use of blood neurofilament light chain protein in the spectrum of neurodegenerative diseases. Mol Neurobiol 57:4667–4691
Khalil M, Pirpamer L, Hofer E, Voortman MM, Barro C, Leppert D, Benkert P, Ropele S, Enzinger C, Fazekas F, Schmidt R, Kuhle J (2020) Serum neurofilament light levels in normal aging and their association with morphologic brain changes. Nat Commun 11:812
Finkel RS, Mercuri E, Darras BT, Connolly AM, Kuntz NL, Kirschner J, Chiriboga CA, Saito K, Servais L, Tizzano E, Topaloglu H, Tulinius M, Montes J, Glanzman AM, Bishop K, Zhong ZJ, Gheuens S, Bennett CF, Schneider E, Farwell W, De Vivo DC, Group ES (2017) Nusinersen versus sham control in infantile-onset spinal muscular atrophy. N Engl J Med 377:1723–1732
Freigang M, Steinacker P, Wurster CD, Schreiber-Katz O, Osmanovic A, Petri S, Koch JC, Rostásy K, Huss A, Tumani H, Winter B, Falkenburger B, Ludolph AC, Otto M, Hermann A, Günther R (2022) Glial fibrillary acidic protein in cerebrospinal fluid of patients with spinal muscular atrophy. Ann Clin Transl Neurol 9:1437–1448
Nitz E, Smitka M, Schallner J, Akgün K, Ziemssen T, von der Hagen M, Tüngler V (2021) Serum neurofilament light chain in pediatric spinal muscular atrophy patients and healthy children. Ann Clin Transl Neurol 8:2013–2024
Darras BT, Sumner CJ, Muntoni F, Crawford TO, Finkel RS, Mercuri E, De Vivo DC, Oskoui M, Tizzano EF, Ryan MM, Liu Y, Petrillo M, Kandinov B, Wong J, Farwell W (2020) Plasma phosphorylated neurofilament heavy chain levels over time in participants with infantile-and later-onset SMA: data from the SHINE Study (1692). Neurology 94:1692
Darras BT, Crawford TO, Finkel RS, Mercuri E, De Vivo DC, Oskoui M, Tizzano EF, Ryan MM, Muntoni F, Zhao G, Staropoli J, McCampbell A, Petrillo M, Stebbins C, Fradette S, Farwell W, Sumner CJ (2019) Neurofilament as a potential biomarker for spinal muscular atrophy. Ann Clin Transl Neurol 6:932–944
Olsson B, Alberg L, Cullen NC, Michael E, Wahlgren L, Kroksmark AK, Rostasy K, Blennow K, Zetterberg H, Tulinius M (2019) NFL is a marker of treatment response in children with SMA treated with nusinersen. J Neurol 266:2129–2136
Totzeck A, Stolte B, Kizina K, Bolz S, Schlag M, Thimm A, Kleinschnitz C, Hagenacker T (2019) Neurofilament heavy chain and tau protein are not elevated in cerebrospinal fluid of adult patients with spinal muscular atrophy during loading with nusinersen. Int J Mol Sci 20(21):5397. https://doi.org/10.3390/ijms20215397
Wurster CD, Steinacker P, Gunther R, Koch JC, Lingor P, Uzelac Z, Witzel S, Wollinsky K, Winter B, Osmanovic A, Schreiber-Katz O, Al Shweiki R, Ludolph AC, Petri S, Hermann A, Otto M, Net MND (2020) Neurofilament light chain in serum of adolescent and adult SMA patients under treatment with nusinersen. J Neurol 267:36–44
Faravelli I, Meneri M, Saccomanno D, Velardo D, Abati E, Gagliardi D, Parente V, Petrozzi L, Ronchi D, Stocchetti N, Calderini E, D’Angelo G, Chidini G, Prandi E, Ricci G, Siciliano G, Bresolin N, Comi GP, Corti S, Magri F, Govoni A (2020) Nusinersen treatment and cerebrospinal fluid neurofilaments: an explorative study on Spinal Muscular Atrophy type 3 patients. J Cell Mol Med 24:3034–3039
Rich KA, Fox A, Yalvac M, Heintzman S, Tellez M, Bartlett A, Severyn S, Linsenmayer M, Kelly K, Reynolds J, Sterling GB, Weaver T, Rajneesh K, Pino MG, Arnold WD, Elsheikh B, Kolb SJ (2022) Neurofilament levels in CSF and serum in an adult SMA cohort treated with nusinersen. J Neuromuscul Dis 9:111–119
Farrar MA, Muntoni F, Sumner CJ, Crawford TO, Finkel RS, Mercuri E, Jiang X, Sohn J, Petrillo M, Garafalo S, Farwell W (2021) Plasma phosphorylated neurofilament heavy chain (pNF-H) level is associated with future motor function in nusinersen-treated individuals with later-onset Spinal Muscular Atrophy (SMA) (2248). Neurology 96:2248
Buée L, Bussière T, Buée-Scherrer V, Delacourte A, Hof PR (2000) Tau protein isoforms, phosphorylation and role in neurodegenerative disorders. Brain Res Brain Res Rev 33:95–130
Xia Y, Prokop S, Gorion K-MM, Kim JD, Sorrentino ZA, Bell BM, Manaois AN, Chakrabarty P, Davies P, Giasson BI (2020) Tau Ser208 phosphorylation promotes aggregation and reveals neuropathologic diversity in Alzheimer’s disease and other tauopathies. Acta Neuropathol Commun 8:88
Winter B, Guenther R, Ludolph AC, Hermann A, Otto M, Wurster CD (2019) Neurofilaments and tau in CSF in an infant with SMA type 1 treated with nusinersen. J Neurol Neurosurg Psychiatry 90:1068–1069
Johannsen J, Weiss D, Daubmann A, Schmitz L, Denecke J (2021) Evaluation of putative CSF biomarkers in paediatric spinal muscular atrophy (SMA) patients before and during treatment with nusinersen. J Cell Mol Med 25:8419–8431
Walter MC, Wenninger S, Thiele S, Stauber J, Hiebeler M, Greckl E, Stahl K, Pechmann A, Lochmuller H, Kirschner J, Schoser B (2019) Safety and treatment effects of nusinersen in longstanding adult 5q-SMA type 3—a prospective observational study. J Neuromuscul Dis 6:453–465
Palop JJ, Mucke L (2010) Amyloid-β–induced neuronal dysfunction in Alzheimer’s disease: from synapses toward neural networks. Nat Neurosci 13:812–818
Alobuia WM, Xia W, Vohra BP (2013) Axon degeneration is key component of neuronal death in amyloid-β toxicity. Neurochem Int 63:782–789
Introna A, Milella G, D’Errico E, Fraddosio A, Scaglione G, Ucci M, Ruggieri M, Simone IL (2021) Is cerebrospinal fluid amyloid-β42 a promising biomarker of response to nusinersen in adult spinal muscular atrophy patients? Muscle Nerve 63:905–909
Vidoni C, Follo C, Savino M, Melone MA, Isidoro C (2016) The role of Cathepsin D in the pathogenesis of human neurodegenerative disorders. Med Res Rev 36:845–870
Offen D, Barhum Y, Melamed E, Embacher N, Schindler C, Ransmayr G (2009) Spinal cord mRNA profile in patients with ALS: comparison with transgenic mice expressing the human SOD-1 mutant. J Mol Neurosci 38:85–93
Cullen V, Lindfors M, Ng J, Paetau A, Swinton E, Kolodziej P, Boston H, Saftig P, Woulfe J, Feany MB, Myllykangas L, Schlossmacher MG, Tyynela J (2009) Cathepsin D expression level affects alpha-synuclein processing, aggregation, and toxicity in vivo. Mol Brain 2:5
Letronne F, Laumet G, Ayral AM, Chapuis J, Demiautte F, Laga M, Vandenberghe ME, Malmanche N, Leroux F, Eysert F, Sottejeau Y, Chami L, Flaig A, Bauer C, Dourlen P, Lesaffre M, Delay C, Huot L, Dumont J, Werkmeister E, Lafont F, Mendes T, Hansmannel F, Dermaut B, Deprez B, Herard AS, Dhenain M, Souedet N, Pasquier F, Tulasne D, Berr C, Hauw JJ, Lemoine Y, Amouyel P, Mann D, Deprez R, Checler F, Hot D, Delzescaux T, Gevaert K, Lambert JC (2016) ADAM30 downregulates APP-linked defects through cathepsin D activation in Alzheimer’s disease. EBioMedicine 9:278–292
Suire CN, Leissring MA (2021) Cathepsin D: a candidate link between amyloid beta-protein and tauopathy in Alzheimer disease. J Exp Neurol 2:10–15
Schorling DC, Kölbel H, Hentschel A, Pechmann A, Meyer N, Wirth B, Rombo R, Sickmann A, Kirschner J, Schara-Schmidt U, Lochmüller H, Roos A, consortium tS (2022) Cathepsin D as biomarker in cerebrospinal fluid of nusinersen-treated patients with spinal muscular atrophy. Eur J Neurol 29:2084–2096
Kessler T, Latzer P, Schmid D, Warnken U, Saffari A, Ziegler A, Kollmer J, Möhlenbruch M, Ulfert C, Herweh C, Wildemann B, Wick W, Weiler M (2020) Cerebrospinal fluid proteomic profiling in nusinersen-treated patients with spinal muscular atrophy. J Neurochem 153:650–661
Saffari A, Cannet C, Blaschek A, Hahn A, Hoffmann GF, Johannsen J, Kirsten R, Kockaya M, Kölker S, Müller-Felber W, Roos A, Schäfer H, Schara U, Spraul M, Trefz FK, Vill K, Wick W, Weiler M, Okun JG, Ziegler A (2021) (1)H-NMR-based metabolic profiling identifies non-invasive diagnostic and predictive urinary fingerprints in 5q spinal muscular atrophy. Orphanet J Rare Dis 16:441
Abati E, Citterio G, Bresolin N, Comi GP, Corti S (2020) Glial cells involvement in spinal muscular atrophy: Could SMA be a neuroinflammatory disease? Neurobiol Dis 140:104870
Rindt H, Feng Z, Mazzasette C, Glascock JJ, Valdivia D, Pyles N, Crawford TO, Swoboda KJ, Patitucci TN, Ebert AD, Sumner CJ, Ko CP, Lorson CL (2015) Astrocytes influence the severity of spinal muscular atrophy. Hum Mol Genet 24:4094–4102
Kanneganti M, Kamba A, Mizoguchi E (2012) Role of chitotriosidase (chitinase 1) under normal and disease conditions. J Epithelial Biol Pharmacol 5:1–9
Gray E, Thompson AG, Wuu J, Pelt J, Talbot K, Benatar M, Turner MR (2020) CSF chitinases before and after symptom onset in amyotrophic lateral sclerosis. Ann Clin Transl Neurol 7:1296–1306
Mattsson N, Tabatabaei S, Johansson P, Hansson O, Andreasson U, Månsson JE, Johansson JO, Olsson B, Wallin A, Svensson J, Blennow K, Zetterberg H (2011) Cerebrospinal fluid microglial markers in Alzheimer’s disease: elevated chitotriosidase activity but lack of diagnostic utility. NeuroMol Med 13:151–159
Freigang M, Steinacker P, Wurster CD, Schreiber-Katz O, Osmanovic A, Petri S, Koch JC, Rostásy K, Falkenburger B, Ludolph AC, Otto M, Hermann A, Günther R (2021) Increased chitotriosidase 1 concentration following nusinersen treatment in spinal muscular atrophy. Orphanet J Rare Dis 16:330
Ando S, Osanai D, Takahashi K, Nakamura S, Shimazawa M, Hara H (2020) Survival motor neuron protein regulates oxidative stress and inflammatory response in microglia of the spinal cord in spinal muscular atrophy. J Pharmacol Sci 144:204–211
De Wel B, De Schaepdryver M, Poesen K, Claeys KG (2022) Biochemical and clinical biomarkers in adult SMA 3–4 patients treated with nusinersen for 22 months. Ann Clin Transl Neurol 9:1241–1251
Gingele S, Hümmert MW, Alvermann S, Jendretzky KF, Bönig L, Brieskorn M, Schwenkenbecher P, Sühs K-W, Müschen LH, Osmanovic A, Schreiber-Katz O, Stangel M, Petri S, Skripuletz T (2019) Routine cerebrospinal fluid cytology reveals unique inclusions in macrophages during treatment with nusinersen. Front Neurol 10:735. https://doi.org/10.3389/fneur.2019.00735
Bonneh-Barkay D, Bissel SJ, Kofler J, Starkey A, Wang G, Wiley CA (2012) Astrocyte and macrophage regulation of YKL-40 expression and cellular response in neuroinflammation. Brain Pathol 22:530–546
Bonneh-Barkay D, Wang G, Starkey A, Hamilton RL, Wiley CA (2010) In vivo CHI3L1 (YKL-40) expression in astrocytes in acute and chronic neurological diseases. J Neuroinflammation 7:34
Kolb SJ, Coffey CS, Yankey JW, Krosschell K, Arnold WD, Rutkove SB, Swoboda KJ, Reyna SP, Sakonju A, Darras BT, Shell R, Kuntz N, Castro D, Iannaccone ST, Parsons J, Connolly AM, Chiriboga CA, McDonald C, Burnette WB, Werner K, Thangarajh M, Shieh PB, Finanger E, Cudkowicz ME, McGovern MM, McNeil DE, Finkel R, Kaye E, Kingsley A, Renusch SR, McGovern VL, Wang X, Zaworski PG, Prior TW, Burghes AH, Bartlett A, Kissel JT, Neuro NCTN, on behalf of the NNSMABI (2016) Baseline results of the NeuroNEXT spinal muscular atrophy infant biomarker study. Ann Clin Transl Neurol 3:132–145
Donato R (2001) S100: a multigenic family of calcium-modulated proteins of the EF-hand type with intracellular and extracellular functional roles. Int J Biochem Cell Biol 33:637–668
Thelin EP, Zeiler FA, Ercole A, Mondello S, Büki A, Bellander BM, Helmy A, Menon DK, Nelson DW (2017) Serial sampling of serum protein biomarkers for monitoring human traumatic brain injury dynamics: a systematic review. Front Neurol 8:300
Michetti F, D’Ambrosi N, Toesca A, Puglisi MA, Serrano A, Marchese E, Corvino V, Geloso MC (2019) The S100B story: from biomarker to active factor in neural injury. J Neurochem 148:168–187
Schreml J, Riessland M, Paterno M, Garbes L, Roßbach K, Ackermann B, Krämer J, Somers E, Parson SH, Heller R, Berkessel A, Sterner-Kock A, Wirth B (2013) Severe SMA mice show organ impairment that cannot be rescued by therapy with the HDACi JNJ-26481585. Eur J Hum Genet 21:643–652
Møller P, Moe N, Saugstad O, Skullerud K, Velken M, Berg K, Nitter-Hauge S, Børresen AL (1990) Spinal muscular atrophy type I combined with atrial septal defect in three sibs. Clin Genet 38:81–83
Rudnik-Schöneborn S, Heller R, Berg C, Betzler C, Grimm T, Eggermann T, Eggermann K, Wirth R, Wirth B, Zerres K (2008) Congenital heart disease is a feature of severe infantile spinal muscular atrophy. J Med Genet 45:635–638
Rudnik-Schöneborn S, Vogelgesang S, Armbrust S, Graul-Neumann L, Fusch C, Zerres K (2010) Digital necroses and vascular thrombosis in severe spinal muscular atrophy. Muscle Nerve 42:144–147
Shababi M, Lorson CL, Rudnik-Schoneborn SS (2014) Spinal muscular atrophy: a motor neuron disorder or a multi-organ disease? J Anat 224:15–28
Yeo CJJ, Darras BT (2020) Overturning the paradigm of spinal muscular atrophy as just a motor neuron disease. Pediatr Neurol 109:12–19
Bowerman M, Murray LM, Beauvais A, Pinheiro B, Kothary R (2012) A critical smn threshold in mice dictates onset of an intermediate spinal muscular atrophy phenotype associated with a distinct neuromuscular junction pathology. Neuromuscul Disord 22:263–276
Cifuentes-Diaz C, Frugier T, Tiziano FD, Lacène E, Roblot N, Joshi V, Moreau MH, Melki J (2001) Deletion of murine SMN exon 7 directed to skeletal muscle leads to severe muscular dystrophy. J Cell Biol 152:1107–1114
Kariya S, Park GH, Maeno-Hikichi Y, Leykekhman O, Lutz C, Arkovitz MS, Landmesser LT, Monani UR (2008) Reduced SMN protein impairs maturation of the neuromuscular junctions in mouse models of spinal muscular atrophy. Hum Mol Genet 17:2552–2569
Lee YI, Mikesh M, Smith I, Rimer M, Thompson W (2011) Muscles in a mouse model of spinal muscular atrophy show profound defects in neuromuscular development even in the absence of failure in neuromuscular transmission or loss of motor neurons. Dev Biol 356:432–444
Martinez-Hernandez R, Soler-Botija C, Also E, Alias L, Caselles L, Gich I, Bernal S, Tizzano EF (2009) The developmental pattern of myotubes in spinal muscular atrophy indicates prenatal delay of muscle maturation. J Neuropathol Exp Neurol 68:474–481
Boyer JG, Ferrier AR, Kothary R (2013) More than a bystander: the contributions of intrinsic skeletal muscle defects in motor neuron diseases. Front Physiol 4:356. https://doi.org/10.3389/fphys.2013.00356
Hamilton G, Gillingwater TH (2013) Spinal muscular atrophy: going beyond the motor neuron. Trends Mol Med 19:40–50
Martínez-Hernández R, Bernal S, Also-Rallo E, Alías L, Barceló M, Hereu M, Esquerda JE, Tizzano EF (2013) Synaptic defects in type I spinal muscular atrophy in human development. J Pathol 229:49–61
Funakoshi H, Belluardo N, Arenas E, Yamamoto Y, Casabona A, Persson H, Ibáñez CF (1995) Muscle-derived neurotrophin-4 as an activity-dependent trophic signal for adult motor neurons. Science 268:1495–1499
Newsholme EA, Beis I, Leech AR, Zammit VA (1978) The role of creatine kinase and arginine kinase in muscle. Biochem J 172:533–537
Wyss M, Kaddurah-Daouk R (2000) Creatine and creatinine metabolism. Physiol Rev 80:1107–1213
Lombardi V, Querin G, Ziff OJ, Zampedri L, Martinelli I, Heller C, Foiani M, Bertolin C, Lu CH, Malik B, Allen K, Rinaldi C, Zetterberg H, Heslegrave A, Greensmith L, Hanna M, Soraru G, Malaspina A, Fratta P (2019) Muscle and not neuronal biomarkers correlate with severity in spinal and bulbar muscular atrophy. Neurology 92:e1205–e1211
Querin G, Bede P, Marchand-Pauvert V, Pradat P-F (2018) Biomarkers of spinal and bulbar muscle atrophy (SBMA): a comprehensive review. Front Neurol. 9:844. https://doi.org/10.3389/fneur.2018.00844
Chiò A, Calvo A, Bovio G, Canosa A, Bertuzzo D, Galmozzi F, Cugnasco P, Clerico M, De Mercanti S, Bersano E, Cammarosano S, Ilardi A, Manera U, Moglia C, Sideri R, Marinou K, Bottacchi E, Pisano F, Cantello R, Mazzini L, Mora G (2014) Amyotrophic lateral sclerosis outcome measures and the role of albumin and creatinine: a population-based study. JAMA Neurol 71:1134–1142
Shefner JM, Cudkowicz ME, Schoenfeld D, Conrad T, Taft J, Chilton M, Urbinelli L, Qureshi M, Zhang H, Pestronk A, Caress J, Donofrio P, Sorenson E, Bradley W, Lomen-Hoerth C, Pioro E, Rezania K, Ross M, Pascuzzi R, Heiman-Patterson T, Tandan R, Mitsumoto H, Rothstein J, Smith-Palmer T, MacDonald D, Burke D (2004) A clinical trial of creatine in ALS. Neurology 63:1656–1661
Alves CRR, Zhang R, Johnstone AJ, Garner R, Nwe PH, Siranosian JJ, Swoboda KJ (2020) Serum creatinine is a biomarker of progressive denervation in spinal muscular atrophy. Neurology 94:e921–e931
Freigang M, Wurster CD, Hagenacker T, Stolte B, Weiler M, Kamm C, Schreiber-Katz O, Osmanovic A, Petri S, Kowski A, Meyer T, Koch JC, Cordts I, Deschauer M, Lingor P, Aust E, Petzold D, Ludolph AC, Falkenburger B, Hermann A, Günther R (2021) Serum creatine kinase and creatinine in adult spinal muscular atrophy under nusinersen treatment. Ann Clin Transl Neurol 8:1049–1063
Deutsch L, Osredkar D, Plavec J, Stres B (2021) Spinal muscular atrophy after nusinersen therapy: improved physiology in pediatric patients with no significant change in urine, serum, and liquor 1H-NMR metabolomes in comparison to an age-matched, healthy cohort. Metabolites 11(4):206. https://doi.org/10.3390/metabo11040206
Alves CR, Santiago BM, Lima FR, Otaduy MC, Calich AL, Tritto AC, de Sa Pinto AL, Roschel H, Leite CC, Benatti FB, Bonfa E, Gualano B (2013) Creatine supplementation in fibromyalgia: a randomized, double-blind, placebo-controlled trial. Arthritis Care Res (Hoboken) 65:1449–1459
Kley RA, Tarnopolsky MA, Vorgerd M (2013) Creatine for treating muscle disorders. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004760.pub4
Wong BL, Hynan LS, Iannaccone ST, and the American Spinal Muscular Atrophy Randomized Trials G (2007) A randomized, placebo-controlled trial of creatine in children with spinal muscular atrophy. J Clin Neuromusc Dis 8
Ordway GA, Garry DJ (2004) Myoglobin: an essential hemoprotein in striated muscle. J Exp Biol 207:3441–3446
Guo H, Lu M, Ma Y, Liu X (2021) Myoglobin: a new biomarker for spinal and bulbar muscular atrophy? Int J Neurosci 131:1209–1214
Gomes AV, Potter JD, Szczesna-Cordary D (2002) The role of troponins in muscle contraction. IUBMB Life 54:323–333
Park KC, Gaze DC, Collinson PO, Marber MS (2017) Cardiac troponins: from myocardial infarction to chronic disease. Cardiovasc Res 113:1708–1718
Finsterer J, Stöllberger C, Krugluger W (2007) Cardiac and noncardiac, particularly neuromuscular, disease with troponin-T positivity. Neth J Med 65:289–295
Castro-Gomez S, Radermacher B, Tacik P, Mirandola SR, Heneka MT, Weydt P (2021) Teaching an old dog new tricks: serum troponin T as a biomarker in amyotrophic lateral sclerosis. Brain Commun 3:fcab274
Kubinski S, Claus P (2022) Protein network analysis reveals a functional connectivity of dysregulated processes in ALS and SMA. Neuroscience insights 17:26331055221087740
Dhoot GK, Pearce GW (1984) Changes in the distribution of fast and slow forms of troponin I in some neuromuscular disorders. J Neurol Sci 65:1–15
Arnold WD, Porensky PN, McGovern VL, Iyer CC, Duque S, Li X, Meyer K, Schmelzer L, Kaspar BK, Kolb SJ, Kissel JT, Burghes AH (2014) Electrophysiological biomarkers in spinal muscular atrophy: preclinical proof of concept. Ann Clin Transl Neurol 1:34–44
Günther R, Neuwirth C, Koch JC, Lingor P, Braun N, Untucht R, Petzold D, Weber M, Hermann A (2019) Motor Unit Number Index (MUNIX) of hand muscles is a disease biomarker for adult spinal muscular atrophy. Clin Neurophysiol 130:315–319
Swoboda KJ, Prior TW, Scott CB, McNaught TP, Wride MC, Reyna SP, Bromberg MB (2005) Natural history of denervation in SMA: relation to age, SMN2 copy number, and function. Ann Neurol 57:704–712
Weng W-C, Hsu Y-K, Chang F-M, Lin C-Y, Hwu W-L, Lee W-T, Lee N-C, Chien Y-H (2021) CMAP changes upon symptom onset and during treatment in spinal muscular atrophy patients: lessons learned from newborn screening. Genet Med 23:415–420
Al-Zaidy SA, Kolb SJ, Lowes L, Alfano LN, Shell R, Church KR, Nagendran S, Sproule DM, Feltner DE, Wells C, Ogrinc F, Menier M, L’Italien J, Arnold WD, Kissel JT, Kaspar BK, Mendell JR (2019) AVXS-101 (Onasemnogene Abeparvovec) for SMA1: comparative study with a prospective natural history cohort. J Neuromuscul Dis 6:307–317
Kariyawasam D, D’Silva A, Howells J, Herbert K, Geelan-Small P, Lin CS, Farrar MA (2020) Motor unit changes in children with symptomatic spinal muscular atrophy treated with nusinersen. J Neurol Neurosurg Psychiatry 92:78–85
Darras BT, Chiriboga CA, Iannaccone ST, Swoboda KJ, Montes J, Mignon L, Xia S, Bennett CF, Bishop KM, Shefner JM, Green AM, Sun P, Bhan I, Gheuens S, Schneider E, Farwell W, De Vivo DC (2019) Nusinersen in later-onset spinal muscular atrophy: Long-term results from the phase 1/2 studies. Neurology 92:e2492–e2506
Querin G, Lenglet T, Debs R, Stojkovic T, Behin A, Salachas F, Le Forestier N, Amador MdM, Lacomblez L, Meininger V, Bruneteau G, Laforêt P, Blancho S, Marchand-Pauvert V, Bede P, Hogrel J-Y, Pradat P-F (2018) The motor unit number index (MUNIX) profile of patients with adult spinal muscular atrophy. Clin Neurophysiol 129:2333–2340
Schneider C, Wassermann MK, Grether NB, Fink GR, Wunderlich G, Lehmann HC (2021) Motor unit number estimation in adult patients with spinal muscular atrophy treated with nusinersen. Eur J Neurol 28:3022–3029
Nandedkar SD, Barkhaus PE, StÅlberg EV (2010) Motor unit number index (MUNIX): principle, method, and findings in healthy subjects and in patients with motor neuron disease. Muscle Nerve 42:798–807
Escorcio-Bezerra ML, Abrahao A, de Castro I, Chieia MAT, de Azevedo LA, Pinheiro DS, de Oliveira Braga NI, de Oliveira ASB, Manzano GM (2016) MUNIX: reproducibility and clinical correlations in amyotrophic lateral sclerosis. Clin Neurophysiol 127:2979–2984
Boulay C, Delmont E, Audic F, Chabrol B, Attarian S (2021) Motor unit number index: a potential electrophysiological biomarker for pediatric spinal muscular atrophy. Muscle Nerve 64:445–453
Verma S, Forte J, Ritchey M, Shah D (2020) Motor unit number index in children with later-onset spinal muscular atrophy. Muscle Nerve 62:633–637
Fatehi F, Delmont E, Grapperon A-M, Salort-Campana E, Sévy A, Verschueren A, Boucraut J, Attarian S (2017) Motor unit number index (MUNIX) in patients with anti-MAG neuropathy. Clin Neurophysiol 128:1264–1269
Rutkove SB, Shefner JM, Gregas M, Butler H, Caracciolo J, Lin C, Fogerson PM, Mongiovi P, Darras BT (2010) Characterizing spinal muscular atrophy with electrical impedance myography. Muscle Nerve 42:915–921
Kolb SJ, Coffey CS, Yankey JW, Krosschell KJ, Arnold WD, Rutkove SB, Swoboda KJ, Reyna SP, Sakonju A, Darras BT, Shell R, Kuntz NL, Castro D, Iannaccone ST, Parsons JA, Connolly A, Chiriboga CA, McDonald CM, Burnette WB, Werner K, Thangarajh M, Shieh PB, Finanger EL, Cudkowicz ME, McGovern MM, McNeil DE, Finkel RS, Kaye ED, Kingsley A, Renusch SR, McGovern VL, Wang X, Zaworski PG, Prior TW, Burghes AHM, Bartlett A, Kissel JT (2016) Baseline results of the NeuroNEXT spinal muscular atrophy infant biomarker study. Ann Clin Transl Neurol 3:132–145
Li J, Geisbush TR, Arnold WD, Rosen GD, Zaworski PG, Rutkove SB (2014) A comparison of three electrophysiological methods for the assessment of disease status in a mild spinal muscular atrophy mouse model. PLoS ONE 9:e111428
Goulet BB, Kothary R, Parks RJ (2013) At the “junction” of spinal muscular atrophy pathogenesis: the role of neuromuscular junction dysfunction in SMA disease progression. Curr Mol Med 13:1160–1174
Kong L, Wang X, Choe DW, Polley M, Burnett BG, Bosch-Marcé M, Griffin JW, Rich MM, Sumner CJ (2009) Impaired synaptic vesicle release and immaturity of neuromuscular junctions in spinal muscular atrophy mice. J Neurosci 29:842–851
Murray LM, Comley LH, Thomson D, Parkinson N, Talbot K, Gillingwater TH (2008) Selective vulnerability of motor neurons and dissociation of pre-and post-synaptic pathology at the neuromuscular junction in mouse models of spinal muscular atrophy. Hum Mol Genet 17:949–962
Arnold WD, Severyn S, Zhao S, Kline D, Linsenmayer M, Kelly K, Tellez M, Bartlett A, Heintzman S, Reynolds J, Sterling G, Weaver T, Rajneesh K, Burghes AHM, Kolb SJ, Elsheikh B (2021) Persistent neuromuscular junction transmission defects in adults with spinal muscular atrophy treated with nusinersen. BMJ neurology open 3:e000164
Memorandum MRC (1976) Aids to the examination of the peripheral nervous system. HMSO, London
Escolar DM, Henricson EK, Mayhew J, Florence J, Leshner R, Patel KM, Clemens PR (2001) Clinical evaluator reliability for quantitative and manual muscle testing measures of strength in children. Muscle Nerve 24:787–793
Florence JM, Pandya S, King WM, Robison JD, Baty J, Miller JP, Schierbecker J, Signore LC (1992) Intrarater reliability of manual muscle test (Medical Research Council scale) grades in Duchenne’s muscular dystrophy. Phys Ther 72:115–122
Van der Ploeg R, Oosterhuis H (2001) Physical examination–measurement of muscle strength. Ned Tijdschr Geneeskd 145:19–23
Merlini L, Mazzone ES, Solari A, Morandi L (2002) Reliability of hand-held dynamometry in spinal muscular atrophy. Muscle Nerve 26:64–70
Merlini L, Bertini E, Minetti C, Mongini T, Morandi L, Angelini C, Vita G (2004) Motor function–muscle strength relationship in spinal muscular atrophy. Muscle Nerve 29:548–552
De Wel B, Goosens V, Sobota A, Van Camp E, Geukens E, Van Kerschaver G, Jagut M, Claes K, Claeys KG (2021) Nusinersen treatment significantly improves hand grip strength, hand motor function and MRC sum scores in adult patients with spinal muscular atrophy types 3 and 4. J Neurol 268:923–935
Seferian AM, Moraux A, Canal A, Decostre V, Diebate O, Le Moing AG, Gidaro T, Deconinck N, Van Parys F, Vereecke W, Wittevrongel S, Annoussamy M, Mayer M, Maincent K, Cuisset JM, Tiffreau V, Denis S, Jousten V, Quijano-Roy S, Voit T, Hogrel JY, Servais L (2015) Upper limb evaluation and one-year follow up of non-ambulant patients with spinal muscular atrophy: an observational multicenter trial. PLoS ONE 10:e0121799
Gozal D (2000) Pulmonary manifestations of neuromuscular disease with special reference to Duchenne muscular dystrophy and spinal muscular atrophy. Pediatr Pulmonol 29:141–150
Ioos C, Leclair-Richard D, Mrad S, Barois A, Estournet-Mathiaud B (2004) Respiratory capacity course in patients with infantile spinal muscular atrophy. Chest 126:831–837
Wijngaarde CA, Veldhoen ES, van Eijk RPA, Stam M, Otto LAM, Asselman F-L, Wösten-van Asperen RM, Hulzebos EHJ, Verweij-van den Oudenrijn LP, Bartels B, Cuppen I, Wadman RI, van den Berg LH, van der Ent CK, van der Pol WL (2020) Natural history of lung function in spinal muscular atrophy. Orphanet J Rare Dis 15:88
Gómez-García de la Banda M, Amaddeo A, Khirani S, Pruvost S, Barnerias C, Dabaj I, Bénézit A, Durigneux J, Carlier RY, Desguerre I, Quijano-Roy S, Fauroux B (2021) Assessment of respiratory muscles and motor function in children with SMA treated by nusinersen. Pediatr Pulmonol 56:299–306
Lavie M, Diamant N, Cahal M, Sadot E, Be’er M, Fattal-Valevski A, Sagi L, Domany KA, Amirav I (2021) Nusinersen for spinal muscular atrophy type 1: real-world respiratory experience. Pediatr Pulmonol 56:291–298
LoMauro A, Mastella C, Alberti K, Masson R, Aliverti A, Baranello G (2019) Effect of nusinersen on respiratory muscle function in different subtypes of type 1 spinal muscular atrophy. Am J Respir Crit Care Med 200:1547–1550
Chacko A, Sly PD, Ware RS, Begum N, Deegan S, Thomas N, Gauld LM (2022) Effect of nusinersen on respiratory function in paediatric spinal muscular atrophy types 1–3. Thorax 77:40–46
Pechmann A, Behrens M, Dörnbrack K, Tassoni A, Stein S, Vogt S, Zöller D, Bernert G, Hagenacker T, Schara-Schmidt U, Schwersenz I, Walter MC, Baumann M, Baumgartner M, Deschauer M, Eisenkölbl A, Flotats-Bastardas M, Hahn A, Horber V, Husain RA, Illsinger S, Johannsen J, Köhler C, Kölbel H, Müller M, von Moers A, Schlachter K, Schreiber G, Schwartz O, Smitka M, Steiner E, Stögmann E, Trollmann R, Vill K, Weiß C, Wiegand G, Ziegler A, Lochmüller H, Kirschner J, group tSs, (2022) Effect of nusinersen on motor, respiratory and bulbar function in early-onset spinal muscular atrophy. Brain 146(2):668–677. https://doi.org/10.1093/brain/awac252
Morrow JM, Sinclair CD, Fischmann A, Machado PM, Reilly MM, Yousry TA, Thornton JS, Hanna MG (2016) MRI biomarker assessment of neuromuscular disease progression: a prospective observational cohort study. Lancet Neurol 15:65–77
McDonald CM, Carter GT, Abresch RT, Widman LM, Styne DM, Warden N, Kilmer DD (2005) Body Composition and water compartment measurements in boys with duchenne muscular dystrophy. Am J Phys Med Rehabil 84:483–491
Wadman RI, van Bruggen HW, Witkamp TD, Sparreboom-Kalaykova SI, Stam M, van den Berg LH, Steenks MH, van der Pol WL (2014) Bulbar muscle MRI changes in patients with SMA with reduced mouth opening and dysphagia. Neurology 83:1060–1066
Hooijmans MT, Habets LE, van den Berg-Faay SAM, Froeling M, Asselman FL, Strijkers GJ, Jeneson JAL, Bartels B, Nederveen AJ, van der Pol WL (2022) Multi-parametric quantitative magnetic resonance imaging of the upper arm muscles of patients with spinal muscular atrophy. NMR Biomed 35:e4696
Otto LAM, Froeling M, van Eijk RPA, Asselman FL, Wadman R, Cuppen I, Hendrikse J, van der Pol WL (2021) Quantification of disease progression in spinal muscular atrophy with muscle MRI-a pilot study. NMR Biomed 34:e4473
Otto LAM, van der Pol WL, Schlaffke L, Wijngaarde CA, Stam M, Wadman RI, Cuppen I, van Eijk RPA, Asselman FL, Bartels B, van der Woude D, Hendrikse J, Froeling M (2020) Quantitative MRI of skeletal muscle in a cross-sectional cohort of patients with spinal muscular atrophy types 2 and 3. NMR Biomed 33:e4357
Sprenger-Svačina A, Haensch J, Weiss K, Große Hokamp N, Maintz D, Schlamann M, Fink GR, Schloss N, Laukamp K, Wunderlich G, Lehmann HC, Lichtenstein T (2023) MRI correlates of motoneuron loss in SMA. J Neurol 270:503–510
Sproule DM, Punyanitya M, Shen W, Dashnaw S, Martens B, Montgomery M, Montes J, Battista V, Finkel R, Darras B, De Vivo DC, Kaufmann P (2011) Muscle volume estimation by magnetic resonance imaging in spinal muscular atrophy. J Child Neurol 26:309–317
Sproule DM, Montgomery MJ, Punyanitya M, Shen W, Dashnaw S, Montes J, Dunaway S, Finkel R, Darras B, Vivo DC, Kaufmann P (2011) Thigh muscle volume measured by magnetic resonance imaging is stable over a 6-month interval in spinal muscular atrophy. J Child Neurol 26:1252–1259
Gallone A, Mazzi F, Bonanno S, Zanin R, Moscatelli M, Aquino D, Maggi L (2022) Muscle quantitative MRI in adult SMA patients on nusinersen treatment: a longitudinal study. Acta Myolog Myopathies Cardiomyopathies 41:76–83
Kollmer J, Bendszus M, Pham M (2015) MR neurography: diagnostic imaging in the PNS. Clin Neuroradiol 25(Suppl 2):283–289
Kollmer J, Sahm F, Hegenbart U, Purrucker JC, Kimmich C, Schonland SO, Hund E, Heiland S, Hayes JM, Kristen AV, Rocken C, Pham M, Bendszus M, Weiler M (2017) Sural nerve injury in familial amyloid polyneuropathy: MR neurography vs clinicopathologic tools. Neurology 89:475–484
Kollmer J, Weiler M, Purrucker J, Heiland S, Schonland SO, Hund E, Kimmich C, Hayes JM, Hilgenfeld T, Pham M, Bendszus M, Hegenbart U (2018) MR neurography biomarkers to characterize peripheral neuropathy in AL amyloidosis. Neurology 91:e625–e634
Kollmer J, Hilgenfeld T, Ziegler A, Saffari A, Sam G, Hayes JM, Pietsch A, Jost M, Heiland S, Bendszus M, Wick W, Weiler M (2019) Quantitative MR neurography biomarkers in 5q-linked spinal muscular atrophy. Neurology 93:e653–e664
Kollmer J, Kessler T, Sam G, Hayes JM, Lentz SI, Heiland S, Bendszus M, Wick W, Weiler M (2021) Magnetization transfer ratio: a quantitative imaging biomarker for 5q spinal muscular atrophy. Eur J Neurol 28:331–340
El Mendili MM, Lenglet T, Stojkovic T, Behin A, Guimarães-Costa R, Salachas F, Meininger V, Bruneteau G, Le Forestier N, Laforêt P, Lehéricy S, Benali H, Pradat PF (2016) Correction: cervical spinal cord atrophy profile in adult SMN1-linked SMA. PLoS ONE 11:e0167886
Querin G, El Mendili MM, Lenglet T, Behin A, Stojkovic T, Salachas F, Devos D, Le Forestier N, del Mar Amador M, Debs R, Lacomblez L, Meininger V, Bruneteau G, Cohen-Adad J, Lehéricy S, Laforêt P, Blancho S, Benali H, Catala M, Li M, Marchand-Pauvert V, Hogrel J-Y, Bede P, Pradat PF (2019) The spinal and cerebral profile of adult spinal-muscular atrophy: a multimodal imaging study. NeuroImage Clin 21:101618
Savini G, Asteggiano C, Paoletti M, Parravicini S, Pezzotti E, Solazzo F, Muzic SI, Santini F, Deligianni X, Gardani A, Germani G, Farina LM, Bergsland N, Gandini Wheeler-Kingshott CAM, Berardinelli A, Bastianello S, Pichiecchio A (2021) Pilot study on quantitative cervical cord and muscular MRI in spinal muscular atrophy: promising biomarkers of disease evolution and treatment? Front Neurol 12:613834. https://doi.org/10.3389/fneur.2021.613834
Fischer AQ, Carpenter DW, Hartlage PL, Carroll JE, Stephens S (1988) Muscle imaging in neuromuscular disease using computerized real-time sonography. Muscle Nerve 11:270–275
Pillen S, Arts IMP, Zwarts MJ (2008) Muscle ultrasound in neuromuscular disorders. Muscle Nerve 37:679–693
Pillen S, Verrips A, Van Alfen N, Arts I, Sie L, Zwarts M (2007) Quantitative skeletal muscle ultrasound: diagnostic value in childhood neuromuscular disease. Neuromuscul Disord 17:509–516
Wu JS, Darras BT, Rutkove SB (2010) Assessing spinal muscular atrophy with quantitative ultrasound. Neurology 75:526–531
Pillen S, van Alfen N, Sorenson EJ, Boon AJ, Wu JS, Darras BT, Rutkove SB (2011) Assessing spinal muscular atrophy with quantitative ultrasound. Neurology 76:933 (author reply 933-934)
Regensburger AP, Wagner AL, Hanslik G, Schussler SC, Fahlbusch FB, Woelfle J, Jungert J, Trollmann R, Knieling F (2020) Ultra-high-frequency ultrasound in patients with spinal muscular atrophy: a retrospective feasibility study. Muscle Nerve 61:E18–E21
Buonsenso D, Berti B, Palermo C, Leone D, Ferrantini G, De Sanctis R, Onesimo R, Curatola A, Fanelli L, Forcina N, Norcia G, Carnicella S, Lucibello S, Mercuri E, Pane M (2020) Ultrasound assessment of diaphragmatic function in type 1 spinal muscular atrophy. Pediatr Pulmonol 55:1781–1788
Harlaar L, Ciet P, van der Ploeg A, Brusse E, van der Beek N, Wielopolski P, de Bruijne M, Tiddens H, van Doorn P (2018) Imaging of respiratory muscles in neuromuscular disease: a review. Neuromuscul Disord 28:246–256
Hermann W, Langner S, Freigang M, Fischer S, Storch A, Günther R, Hermann A (2022) Affection of respiratory muscles in ALS and SMA. J Clin Med 11:1163
Skalsky AJ, Han JJ, Abresch RT, McDonald CM (2012) Regional and whole-body dual-energy X-ray absorptiometry to guide treatment and monitor disease progression in neuromuscular disease. Phys Med Rehabil Clin N Am 23(67–73):x
Baranello G, De Amicis R, Arnoldi MT, Zanin R, Mastella C, Masson R, Leone A, Alberti K, Foppiani A, Battezzati A, Bertoli S (2020) Evaluation of body composition as a potential biomarker in spinal muscular atrophy. Muscle Nerve 61:530–534
Chen X, Siebourg-Polster J, Wolf D, Czech C, Bonati U, Fischer D, Khwaja O, Strahm M (2017) Feasibility of using microsoft kinect to assess upper limb movement in type III spinal muscular atrophy patients. PLoS ONE 12:e0170472
Chabanon A, Seferian AM, Daron A, Péréon Y, Cances C, Vuillerot C, De Waele L, Cuisset J-M, Laugel V, Schara U, Gidaro T, Gilabert S, Hogrel J-Y, Baudin P-Y, Carlier P, Fournier E, Lowes LP, Hellbach N, Seabrook T, Toledano E, Annoussamy M, Servais L, the NatHis SMAsg, (2018) Prospective and longitudinal natural history study of patients with Type 2 and 3 spinal muscular atrophy: Baseline data NatHis-SMA study. PLoS ONE 13:e0201004
Biogen (2021) A study to assess the clinical validity of Konectom™ in adults living with neuromuscular disorders. ClinicalTrialsgov Identifier: NCT05109637
Funding
Open Access funding enabled and organized by Projekt DEAL. Author HL declares that she has no financial interests. Author MF has received a speaker honorarium from Biogen. Author TH has received research support from Biogen, Novartis GeneTherapies, Roche and Sanofi Genzyme, speakers and consultant honoraria from Biogen, Hormosan, Roche, Alexion, Novartis, Roche, Sanofi-Genzyme, Alnylam and Argenx. Author MW has received consultant honoraria from Biogen and Roche, and has received speaker honoraria and travel support for conference attendance from Biogen. Author CW has received honoraria from Biogen as an advisory board member and for lectures and as an advisory member and consultant from Hoffmann-La Roche. She also received travel expenses from Biogen. Author RG has received personal fees from Biogen, Hofmann-La Roche, Zambon and ITF Pharma. Authors HL, TH, and CW declare that they have no non-financial interests. Author MF received non-financial support from Biogen. Author MW is a member of the European Reference Network for Neuromuscular Diseases (ERN EURO-NMD). Author RG received non-financial support from Biogen. All support was received outside the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical standard statement
This is a narrative review which required no ethical approval.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lapp, H.S., Freigang, M., Hagenacker, T. et al. Biomarkers in 5q-associated spinal muscular atrophy—a narrative review. J Neurol 270, 4157–4178 (2023). https://doi.org/10.1007/s00415-023-11787-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-11787-y