Abstract
Introduction
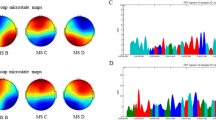
The majority of imaging studies in ALS infer group-level imaging signatures from group comparisons, as opposed to estimating disease burden in individual patients. In a condition with considerable clinical heterogeneity, the characterisation of individual patterns of pathology is hugely relevant. In this study, we evaluate a strategy to track progressive cortical involvement in single patients by using subject-specific reference cohorts.
Methods
We have interrogated a multi-timepoint longitudinal dataset of 61 ALS patients to demonstrate the utility of estimating cortical disease burden and the expansion of cerebral atrophy over time. We contrast our strategy to the gold-standard approach to gauge the advantages and drawbacks of our method. We modelled the evolution of cortical integrity in a conditional growth model, in which we accounted for age, gender, disability, symptom duration, education and handedness. We hypothesised that the variance associated with demographic variables will be successfully eliminated in our approach.
Results
In our model, the only covariate which modulated the expansion of atrophy was motor disability as measured by the ALSFRS-r (t(153) = − 2.533, p = 0.0123). Using the standard approach, age also significantly influenced progression of CT change (t(153) = − 2.151, p = 0.033) demonstrating the validity and potential clinical utility of our approach.
Conclusion
Our strategy of estimating the extent of cortical atrophy in individual patients with ALS successfully corrects for demographic factors and captures relevant cortical changes associated with clinical disability. Our approach provides a framework to interpret single T1-weighted images in ALS and offers an opportunity to track cortical propagation patterns both at individual subject level and at cohort level.






Similar content being viewed by others
Abbreviations
- ALS:
-
Amyotrophic lateral sclerosis
- ALSFRS-r:
-
Revised amyotrophic lateral sclerosis functional rating scale
- ANOVA:
-
Analysis of variance
- Cam-CAN:
-
Cambridge Centre for Ageing and Neuroscience
- CIFTI:
-
Connectivity Informatics Technology Initiative
- CGM:
-
Conditional growth model
- CT:
-
Cortical thickness
- DLPFC:
-
Dorsolateral prefrontal cortex
- EMG:
-
Electromyography
- EP:
-
Electrophysiology
- FA:
-
Flip angle
- FDR:
-
False discovery rate
- FLAIR:
-
Fluid-attenuated inversion recovery
- FOV:
-
Field of view
- FTD:
-
Frontotemporal dementia
- FWER:
-
Family-wise error rate
- GRAPPA:
-
GeneRalised Autocalibrating Partial Parallel Acquisition
- HC:
-
Healthy control
- IR-SPGR:
-
Inversion recovery-prepared spoiled gradient-recalled echo
- IR-TSE:
-
Inversion recovery turbo spin echo
- LL:
-
Log-likelihoods
- M:
-
Arithmetic mean
- ML:
-
Machine learning
- MPRAGE:
-
Magnetisation-prepared rapid gradient echo
- MND:
-
Motor neuron disease
- Mo:
-
Months
- MS:
-
Multiple sclerosis
- PLS:
-
Primary lateral sclerosis
- QC:
-
Quality control
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- SENSE:
-
SENSitivity Encoding
- SR:
-
Spatial resolution
- T:
-
Tesla
- T1w:
-
T1 weighted
- TE:
-
Echo time
- TI:
-
Inversion time
- TMS:
-
Transcranial magnetic stimulation
- TR:
-
Repetition time
- UGM:
-
Unconditional growth model
- UMM:
-
Unconditional means model
- V:
-
Version
- VS:
-
Versus
- Y:
-
Year
References
Eisen, A., et al., Amyotrophic lateral sclerosis: a long preclinical period? J Neurol Neurosurg Psychiatry, 2014.
Querin G et al (2019) Presymptomatic spinal cord pathology in c9orf72 mutation carriers: A longitudinal neuroimaging study. Ann Neurol 86(2):158–167
Lulé, D.E., et al., Deficits in verbal fluency in presymptomatic C9orf72 mutation gene carriers-a developmental disorder. J Neurol Neurosurg Psychiatry, 2020.
Miller T et al (2020) Phase 1–2 Trial of Antisense Oligonucleotide Tofersen for SOD1 ALS. N Engl J Med 383(2):109–119
Mitsumoto H, Brooks BR, Silani V (2014) Clinical trials in amyotrophic lateral sclerosis: why so many negative trials and how can trials be improved? Lancet Neurol 13(11):1127–1138
Chipika RH et al (2019) Tracking a Fast-Moving Disease: Longitudinal Markers, Monitoring, and Clinical Trial Endpoints in ALS. Front Neurol 10:229
Schuster C et al (2015) Presymptomatic and longitudinal neuroimaging in neurodegeneration–from snapshots to motion picture: a systematic review. J Neurol Neurosurg Psychiatry 86(10):1089–1096
Proudfoot M, Bede P, Turner MR (2018) Imaging Cerebral Activity in Amyotrophic Lateral Sclerosis. Front Neurol 9:1148
Schuster C, Hardiman O, Bede P (2016) Development of an Automated MRI-Based Diagnostic Protocol for Amyotrophic Lateral Sclerosis Using Disease-Specific Pathognomonic Features: A Quantitative Disease-State Classification Study. PLoS ONE 11(12):e0167331
Chipika, R.H., et al., The presymptomatic phase of amyotrophic lateral sclerosis: are we merely scratching the surface? J Neurol, 2020.
Devos D et al (2019) A ferroptosis-based panel of prognostic biomarkers for Amyotrophic Lateral Sclerosis. Sci Rep 9(1):2918
Floeter MK, Gendron TF (2018) Biomarkers for Amyotrophic Lateral Sclerosis and Frontotemporal Dementia Associated With Hexanucleotide Expansion Mutations in C9orf72. Front Neurol 9:1063
Blasco H et al (2018) A pharmaco-metabolomics approach in a clinical trial of ALS: Identification of predictive markers of progression. PLoS ONE 13(6):e0198116
Omer T et al (2017) Neuroimaging patterns along the ALS-FTD spectrum: a multiparametric imaging study. Amyotroph Lateral Scler Frontotemporal Degener 18(7–8):611–623
Bede P, Querin G, Pradat PF (2018) The changing landscape of motor neuron disease imaging: the transition from descriptive studies to precision clinical tools. Curr Opin Neurol 31(4):431–438
Menke, R.A.L., et al., The two-year progression of structural and functional cerebral MRI in amyotrophic lateral sclerosis. NeuroImage: Clinical, 2018. 17: p. 953–961.
Trojsi, F., et al., Neurodegeneration of brain networks in the amyotrophic lateral sclerosis-frontotemporal lobar degeneration (ALS-FTLD) continuum: evidence from MRI and MEG studies. CNS Spectr, 2017: p. 1–10.
Trojsi, F., et al., Hippocampal connectivity in Amyotrophic Lateral Sclerosis (ALS): more than Papez circuit impairment. Brain Imaging Behav, 2020.
Bede P et al (2016) The selective anatomical vulnerability of ALS: “disease-defining” and “disease-defying” brain regions. Amyotroph Lateral Scler Frontotemporal Degener 17(7–8):561–570
Christidi F et al (2018) Clinical and Radiological Markers of Extra-Motor Deficits in Amyotrophic Lateral Sclerosis. Front Neurol 9:1005
Agosta F et al (2009) Longitudinal assessment of grey matter contraction in amyotrophic lateral sclerosis: A tensor based morphometry study. Amyotroph Lateral Scler 10(3):168–174
Bede P, Hardiman O (2018) Longitudinal structural changes in ALS: a three time-point imaging study of white and gray matter degeneration. Amyotroph Lateral Scler Frontotemporal Degener 19(3–4):232–241
Meier JM et al (2020) Connectome-Based Propagation Model in Amyotrophic Lateral Sclerosis. Ann Neurol 87(5):725–738
Schuster C, Hardiman O, Bede P (2017) Survival prediction in Amyotrophic lateral sclerosis based on MRI measures and clinical characteristics. BMC Neurol 17(1):73
Welsh RC, Jelsone-Swain LM, Foerster BR (2013) The utility of independent component analysis and machine learning in the identification of the amyotrophic lateral sclerosis diseased brain. Front Hum Neurosci 7:251
Grollemund V et al (2019) Machine Learning in Amyotrophic Lateral Sclerosis: Achievements, Pitfalls, and Future Directions. Front Neurosci 13:135
Querin G et al (2018) Multimodal spinal cord MRI offers accurate diagnostic classification in ALS. J Neurol Neurosurg Psychiatry 89(11):1220–1221
Foerster BR et al (2014) Multimodal MRI as a diagnostic biomarker for amyotrophic lateral sclerosis. Ann Clin Transl Neurol 1(2):107–114
Tahedl M (2020) Towards individualized cortical thickness assessment for clinical routine. J Transl Med 18(1):151
Reuter M, Rosas HD, Fischl B (2010) Highly accurate inverse consistent registration: a robust approach. Neuroimage 53(4):1181–1196
van der Burgh HK et al (2020) Multimodal longitudinal study of structural brain involvement in amyotrophic lateral sclerosis. Neurology 94(24):e2592–e2604
Brooks BR et al (2000) El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord 1(5):293–299
Dale AM, Fischl B, Sereno MI (1999) Cortical surface-based analysis. I Segmentation and surface reconstruction. Neuroimage 9(2):179–194
Fischl, B., M.I. Sereno, and A.M. Dale, Cortical surface-based analysis. II: Inflation, flattening, and a surface-based coordinate system. Neuroimage, 1999. 9(2): p. 195–207.
Fischl B (2012) FreeSurfer. Neuroimage 62(2):774–781
Dickie EW et al (2019) Ciftify: A framework for surface-based analysis of legacy MR acquisitions. Neuroimage 197:818–826
Schaefer A et al (2018) Local-Global Parcellation of the Human Cerebral Cortex from Intrinsic Functional Connectivity MRI. Cereb Cortex 28(9):3095–3114
Yeo BT et al (2011) The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J Neurophysiol 106(3):1125–1165
McFarquhar M et al (2016) Multivariate and repeated measures (MRM): A new toolbox for dependent and multimodal group-level neuroimaging data. Neuroimage 132:373–389
Pinheiro, J., et al., nlme: Linear and Nonlinear Mixed Effects Models. R package version 3.1, 2016. R Core Team.
Laird NM, Ware JH (1982) Random-effects models for longitudinal data. Biometrics 38(4):963–974
Luders, E., A.W. Toga, and P.M. Thompson, Why size matters: Differences in brain volume account for apparent sex differences in callosal anatomy: The sexual dimorphism of the corpus callosum. Neuroimage, 2013. 84c: p. 820–824.
Bede P et al (2014) Sexual dimorphism in ALS: exploring gender-specific neuroimaging signatures. Amyotroph Lateral Scler Frontotemporal Degener 15(3–4):235–243
Menzler K et al (2011) Men and women are different: diffusion tensor imaging reveals sexual dimorphism in the microstructure of the thalamus, corpus callosum and cingulum. Neuroimage 54(4):2557–2562
Agosta F, Spinelli EG, Filippi M (2018) Neuroimaging in amyotrophic lateral sclerosis: current and emerging uses. Expert Rev Neurother 18(5):395–406
Christidi F et al (2018) The Clinical and Radiological Spectrum of Hippocampal Pathology in Amyotrophic Lateral Sclerosis. Front Neurol 9:523
Bede P et al (2019) Brainstem pathology in amyotrophic lateral sclerosis and primary lateral sclerosis: A longitudinal neuroimaging study. Neuroimage Clin 24:102054
Chipika RH et al (2020) “Switchboard” malfunction in motor neuron diseases: Selective pathology of thalamic nuclei in amyotrophic lateral sclerosis and primary lateral sclerosis. Neuroimage Clin 27:102300
Bede P et al (2020) Progressive brainstem pathology in motor neuron diseases: Imaging data from amyotrophic lateral sclerosis and primary lateral sclerosis. Data Brief 29:105229
Feron M et al (2018) Extrapyramidal deficits in ALS: a combined biomechanical and neuroimaging study. J Neurol 265(9):2125–2136
Finegan E et al (2019) Primary lateral sclerosis: a distinct entity or part of the ALS spectrum? Amyotroph Lateral Scler Frontotemporal Degener 20(3–4):133–145
Lebouteux MV et al (2014) Revisiting the spectrum of lower motor neuron diseases with snake eyes appearance on magnetic resonance imaging. Eur J Neurol 21(9):1233–1241
Burke T et al (2016) Measurement of Social Cognition in Amyotrophic Lateral Sclerosis: A Population Based Study. PLoS ONE 11(8):e0160850
Christidi F et al (2020) Neuroimaging data indicate divergent mesial temporal lobe profiles in amyotrophic lateral sclerosis, Alzheimer’s disease and healthy aging. Data Brief 28:104991
Abidi, M., et al., Adaptive functional reorganization in amyotrophic lateral sclerosis: coexisting degenerative and compensatory changes. Eur J Neurol, 2019.
Yunusova Y et al (2019) Clinical Measures of Bulbar Dysfunction in ALS. Front Neurol 10:106
Hardiman, O., et al., Neurodegenerative Disorders: A Clinical Guide. 2016 ed. 2016, Springer Cham Heidelberg New York Dordrecht London© Springer International Publishing Switzerland 2016: Springer International Publishing. 1–336.
Foerster BR et al (2013) Diagnostic accuracy of diffusion tensor imaging in amyotrophic lateral sclerosis: a systematic review and individual patient data meta-analysis. Acad Radiol 20(9):1099–1106
Bede P et al (2018) Connectivity-based characterisation of subcortical grey matter pathology in frontotemporal dementia and ALS: a multimodal neuroimaging study. Brain Imaging Behav 12(6):1696–1707
Westeneng HJ et al (2016) Widespread structural brain involvement in ALS is not limited to the C9orf72 repeat expansion. J Neurol Neurosurg Psychiatry 87(12):1354–1360
Finegan E et al (2019) The clinical and radiological profile of primary lateral sclerosis: a population-based study. J Neurol 266(11):2718–2733
Agosta F et al (2016) Structural brain correlates of cognitive and behavioral impairment in MND. Hum Brain Mapp 37(4):1614–1626
Finegan E et al (2019) Widespread subcortical grey matter degeneration in primary lateral sclerosis: a multimodal imaging study with genetic profiling. Neuroimage Clin 24:102089
Bede P et al (2017) Virtual brain biopsies in amyotrophic lateral sclerosis: Diagnostic classification based on in vivo pathological patterns. Neuroimage Clin 15:653–658
Grollemund V et al (2020) Development and validation of a 1-year survival prognosis estimation model for Amyotrophic Lateral Sclerosis using manifold learning algorithm UMAP. Sci Rep 10(1):13378
Agosta F et al (2010) MRI predictors of long-term evolution in amyotrophic lateral sclerosis. Eur J Neurosci 32(9):1490–1496
Westeneng, H.J., et al., Prognosis for patients with amyotrophic lateral sclerosis: development and validation of a personalised prediction model. Lancet Neurol, 2018.
Elamin M et al (2015) Predicting prognosis in amyotrophic lateral sclerosis: a simple algorithm. J Neurol 262(6):1447–1454
Filippi M et al (1998) Guidelines for using quantitative measures of brain magnetic resonance imaging abnormalities in monitoring the treatment of multiple sclerosis. Ann Neurol 43(4):499–506
Househam E, Swash M (2000) Diagnostic delay in amyotrophic lateral sclerosis: what scope for improvement? J Neurol Sci 180(1–2):76–81
Kraemer M, Buerger M, Berlit P (2010) Diagnostic problems and delay of diagnosis in amyotrophic lateral sclerosis. Clin Neurol Neurosurg 112(2):103–105
Zoccolella S et al (2006) Predictors of delay in the diagnosis and clinical trial entry of amyotrophic lateral sclerosis patients: a population-based study. J Neurol Sci 250(1–2):45–49
Elamin M et al (2017) Identifying behavioural changes in ALS: Validation of the Beaumont Behavioural Inventory (BBI). Amyotroph Lateral Scler Frontotemporal Degener 18(1–2):68–73
Cedarbaum, J.M., et al., The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci, 1999. 169(1–2): p. 13–21.
Burke T et al (2017) Visual encoding, consolidation, and retrieval in amyotrophic lateral sclerosis: executive function as a mediator, and predictor of performance. Amyotroph Lateral Scler Frontotemporal Degener 18(3–4):193–201
Brettschneider J et al (2014) TDP-43 pathology and neuronal loss in amyotrophic lateral sclerosis spinal cord. Acta Neuropathol 128(3):423–437
Brettschneider J et al (2013) Stages of pTDP-43 pathology in amyotrophic lateral sclerosis. Ann Neurol 74(1):20–38
Elamin M et al (2013) Cognitive changes predict functional decline in ALS: a population-based longitudinal study. Neurology 80(17):1590–1597
Westeneng HJ et al (2015) Subcortical structures in amyotrophic lateral sclerosis. Neurobiol Aging 36(2):1075–1082
Pradat PF, El Mendili MM (2014) Neuroimaging to investigate multisystem involvement and provide biomarkers in amyotrophic lateral sclerosis. Biomed Res Int 2014:467560
Pradat P-F et al (2009) Extrapyramidal stiffness in patients with amyotrophic lateral sclerosis. Mov Disord 24(14):2143–2148
Schuster C et al (2016) The segmental diffusivity profile of amyotrophic lateral sclerosis associated white matter degeneration. Eur J Neurol 23(8):1361–1371
Christidi F et al (2014) Uncinate fasciculus microstructure and verbal episodic memory in amyotrophic lateral sclerosis: a diffusion tensor imaging and neuropsychological study. Brain Imaging Behav 8(4):497–505
Agosta F et al (2014) Intrahemispheric and interhemispheric structural network abnormalities in PLS and ALS. Hum Brain Mapp 35(4):1710–1722
Agosta F et al (2014) Resting state functional connectivity alterations in primary lateral sclerosis. Neurobiol Aging 35(4):916–925
Nasseroleslami B et al (2019) Characteristic Increases in EEG Connectivity Correlate With Changes of Structural MRI in Amyotrophic Lateral Sclerosis. Cereb Cortex 29(1):27–41
Lule D et al (2010) Neuroimaging of multimodal sensory stimulation in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 81(8):899–906
Lule D et al (2007) Brain responses to emotional stimuli in patients with amyotrophic lateral sclerosis (ALS). J Neurol 254(4):519–527
Acknowledgements
We are grateful for all patients with ALS for agreeing to participate in this research study, and we are also indebted to their caregivers and families for their support. Without their generosity, this study would have not been possible. We also thank all patients who expressed interest in this study, but were unable to participate for medical or logistical reasons. We also thank the Irish Motor Neuron Disease Association for facilitating recruitment and providing unrelenting support to all patients with ALS and PLS.
Funding
Doctor Marlene Tahedl is funded by the Deutsche Multiple Sklerose Gesellschaft (DMSG), Grant number 2018_DMSG_08. Professor Peter Bede is supported by the Health Research Board (HRB EIA-2017-019), Spastic Paraplegia Foundation, Inc. (SPF), the EU Joint Programme—Neurodegenerative Disease Research (JPND), the Andrew Lydon scholarship, the Irish Institute of Clinical Neuroscience (IICN) and the Iris O'Brien Foundation. The sponsors of the authors had no bearing on the opinions expressed herein.
Author information
Authors and Affiliations
Contributions
MT and PB were involved in the conceptualisation of the study, neuroimaging analyses and drafting the manuscript. RC, JL, SLHS and OH contributed to clinical profiling and data acquisition. MT, RC, JL, SLHS, OH and PB were all involved in the revision of the manuscript for intellectual content.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Ethics approval
All participants provided informed consent in accordance with the approval of the Ethics (Medical Research) Committee—Beaumont Hospital, Dublin, Ireland.
Rights and permissions
About this article
Cite this article
Tahedl, M., Chipika, R.H., Lope, J. et al. Cortical progression patterns in individual ALS patients across multiple timepoints: a mosaic-based approach for clinical use. J Neurol 268, 1913–1926 (2021). https://doi.org/10.1007/s00415-020-10368-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-10368-7