Abstract
Objective
Ocular lateral deviation (OLD) is a conjugate, ipsilesional, horizontal ocular deviation associated with brief (3–5 s) closing of the eyes, commonly linked to the lateral medullary syndrome (LMS). There is limited information regarding OLD in patients with the acute vestibular syndrome (AVS). In one case series 40 years ago OLD was suggested to be a central sign. Recently, horizontal ocular deviation on imaging (RadOLD) was frequently associated with anterior circulation stroke and horizontal gaze palsy. Similarly, RadOLD has been associated with posterior circulation stroke, e.g., LMS and cerebellar stroke, but without clinical correlation with OLD.
Methods
This is a prospective, cross-sectional diagnostic study of 151 acute AVS patients. Patients had spontaneous nystagmus. Horizontal gaze paralysis was an exclusion criterion. We noted the effect of brief 3–5 s eyelid closure on eye position, and then used the HINTS algorithm (the head-impulse test, nystagmus characteristics and skew deviation) and RadOLD, to establish a correlation between clinical and radiologic findings
Results
Of the 151 AVS patients, 100 had a central lesion and 51 a peripheral lesion; 29 of the central lesions were LMS, and 11 had OLD. Additionally, one lateral pontine syndrome had OLD. On opening the eyes 11 patients with OLD and LMS made multiple, hypometric corrective saccades to bring gaze back to straight ahead. 10/11 patients with LMS showed RadOLD.
Conclusions
OLD with multiple hypometric corrective saccades on opening the eyes was infrequent but highly localizing and lateralizing. We emphasize how simple it is to test for OLD, with the caveat that to be specific, it must be present after just brief (3–5 s) eyelid closure.



Similar content being viewed by others
Abbreviations
- AVS:
-
Acute vestibular syndrome
- OLD:
-
Ocular lateral deviation
- LMS:
-
Lateral medullary syndrome
- RadOLD:
-
Radiographic ocular lateral deviation
- HIT:
-
Head-impulse test
- HINTS:
-
Head impulse, nystagmus and tests of skew
- OTR:
-
Ocular tilt reaction
- OMV:
-
Oculomotor vermis
- FOR:
-
Fastigial oculomotor region
References
Tarnutzer AA, Berkowitz AL, Robinson KA, Hsieh YH, Newman-Toker DE (2011) Does my dizzy patient have a stroke? A systematic review of bedside diagnosis in acute vestibular syndrome. CMAJ 183:E571–592
Saber Tehrani AS, Kattah JC, Kerber KA et al (2018) Diagnosing stroke in acute dizziness and vertigo: pitfalls and pearls. Stroke 49:788–795
Moberg APL, Silfverskiöld BP, Valbo S (1962) Imbalance, nystagmus and diplopia in Wallenberg's syndrome. Acta Otolaryngol 55:269–282
Hägstrom L, Hornsten G, Silfverskiöld BP (1969) Oculostatic and visual phenomena occurring in association with Wallenberg's syndrome. Acta Neurol Scand 45:568–582
Hörnsten G (1974) Wallenberg's syndrome. II. Oculomotor and oculostatic disturbances. Acta Neurol Scand 50:447–468
Crevits L, vander Eecken H (1982) Ocular lateropulsion in Wallenberg's syndrome: a prospective clinical study. Acta Neurol Scand 65:219–222
Kim JS, Moon SY, Kim KY et al (2004) Ocular contrapulsion in rostral medial medullary infarction. Neurology 63:1325–1327
Frisen L (1978) Lateropulsion of the eyes—a localizing brainstem sign. J Neurol 218:171–177
Meyer KT, Baloh RW, Krohel GB, Hepler RS (1980) Ocular lateropulsion. A sign of lateral medullary disease. Arch Ophthalmol 98:1614–1616
Jiang N, Fong C, Sahlas DJ, Monteiro S, Larrazabal R (2019) Response to "Potential clinical and radiographic horizontal gaze deviation an early sign of stroke”. J Stroke Cerebrovasc Dis 28:1093–1098
Jiang NN, Fong C, Sahlas DJ, Monteiro S, Larrazabal R (2019) Response to "Potential clinical and radiographic horizontal gaze deviation an early sign of stroke". J Stroke Cerebrovasc Dis 28:104393
Nishimura K, Ohara T, Nagatsuka K, Minematsu K, Toyoda K (2015) Radiographic conjugate horizontal eye deviation in patients with acute cerebellar infarction. J Neurol Sci 355:68–71
Teufel J, Strupp M, Linn J, Kalla R, Feil K (2019) Conjugate eye deviation in unilateral lateral medullary infarction. J Clin Neurol 15:228–234
Kattah JC, Pula J, Newman-Toker DE (2011) Ocular lateropulsion as a central oculomotor sign in acute vestibular syndrome is not posturally dependent. Ann NY Acad Sci 1233:249–255
Yang YJ, Choi JE, Kim MT et al (2019) Measurement of horizontal ocular deviation on magnetic resonance imaging in various disease with acute vertigo. PLoS ONE 14:e0224605
Newman-Toker DE, Kerber KA, Hsieh YH et al (2013) HINTS outperforms ABCD2 to screen for stroke in acute continuous vertigo and dizziness. Acad Emerg Med 20:986–996
Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE (2009) HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke 40:3504–3510
Carmona S, Martinez C, Zalazar G et al (2016) The diagnostic accuracy of truncal ataxia and HINTS as cardinal signs for acute vestibular syndrome. Front Neurol 7:125
Lesley WS, Rangaswamy R, Smith KH, Watkins DM (2009) Predicting acute ischemic stroke by measuring the degree of ocular gaze deviation (Prevost sign) on CT. J Neurointerv Radiol 1:32–34
von Elm E, Altman DG, Egger M et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 147:573–577
Lesley WS, Rangaswamy R, Smith KH, Watkins DM (2009) Predicting acute ischemic stroke by measuring the degree of ocular gaze deviation (Prevost's sign) on CT. J Neurointerv Surg 1:32–34
Kim JS (2003) Pure lateral medullary infarction: clinical-radiological correlation of 130 acute, consecutive patients. Brain 126:1864–1872
Lee H (2014) Isolated vascular vertigo. J Stroke 16:124–130
Lee SU, Park SH, Park JJ et al (2015) Dorsal medullary infarction: distinct syndrome of isolated central vestibulopathy. Stroke 46:3081–3087
Lee JO, Park SH, Kim HJ, Kim MS, Park BR, Kim JS (2014) Vulnerability of the vestibular organs to transient ischemia: implications for isolated vascular vertigo. Neurosci Lett 558:180–185
Kim JS (2000) Vertigo and gait ataxia without usual signs of lateral medullary infarction: a clinical variant related to rostral-dorsolateral lesions. Cerebrovasc Dis 10:471–474
Leigh RJ, Zee DS (2015) the neurology of eye movements. Oxford University Press, New York
Waespe W, Wichmann W (1990) Oculomotor disturbances during visual-vestibular interaction in Wallenberg's lateral medullary syndrome. Brain 113(Pt 3):821–846
Solomon D, Galetta SL, Liu GT (1995) Possible mechanisms for horizontal gaze deviation and lateropulsion in the lateral medullary syndrome. J Neuroophthalmol 15:26–30
Tilikete C, Hermier M, Pelisson D, Vighetto A (2002) Saccadic lateropulsion and upbeat nystagmus: disorders of caudal medulla. Ann Neurol 52:658–662
Kheradmand A, Zee DS (2011) Cerebellum and ocular motor control. Front Neurol 2:53
Robinson FR, Straube A, Fuchs AF (1993) Role of the caudal fastigial nucleus in saccade generation. II. Effects of muscimol inactivation. J Neurophysiol 70:1741–1758
Sato H, Noda H (1992) Saccadic dysmetria induced by transient functional decortication of the cerebellar vermis [corrected]. Exp Brain Res 88:455–458
Kirkham TH, Guitton D, Gans M (1981) Task dependent variations of ocular lateropulsion in Wallenberg's syndrome. Can J Neurol Sci 8:21–26
Helmchen C, Straube A, Buttner U (1994) Saccadic lateropulsion in Wallenberg's syndrome may be caused by a functional lesion of the fastigial nucleus. J Neurol 241:421–426
Tilikete C, Koene A, Nighoghossian N, Vighetto A, Pelisson D (2006) Saccadic lateropulsion in Wallenberg syndrome: a window to access cerebellar control of saccades? Exp Brain Res 174:555–565
Noda H, Sugita S, Ikeda Y (1990) Afferent and efferent connections of the oculomotor region of the fastigial nucleus in the macaque monkey. J Comp Neurol 302:330–348
Takagi M, Zee DS, Tamargo RJ (1998) Effects of lesions of the oculomotor vermis on eye movements in primate: saccades. J Neurophysiol 80:1911–1931
Fuchs AF, Robinson FR, Straube A (1993) Role of the caudal fastigial nucleus in saccade generation. I. Neuronal discharge pattern. J Neurophysiol 70:1723–1740
Kommerell G, Hoyt WF (1973) Lateropulsion of saccadic eye movements. Electro-oculographic studies in a patient with Wallenberg's syndrome. Arch Neurol 28:313–318
Estanol B, Lopez-Rios G (1982) Neuro-otology of the lateral medullary infarct syndrome. Arch Neurol 39:176–179
Cogan DG (1948) Neurologic significance of lateral conjugate deviation of the eyes on forced closure of the lids. Arch Ophthal 39:37–42
Sullivan HC, Kaminski HJ, Maas EF, Weissman JD, Leigh RJ (1991) Lateral deviation of the eyes on forced lid closure in patients with cerebral lesions. Arch Neurol 48:310–311
Maranhao ET, Maranhao-Filho P, Lima MA (2007) Evaluation of the "spasticity of conjugate gaze phenomenon" in unilateral cerebral lesions. Arq Neuropsiquiatr 65:440–442
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Jorge C. Kattah, M.D. Disclosure: Otometrics Corporation loaned us research equipment in 2012, this equipment is no longer in use. Evaluates legal cases related to vestibular disorders in thiamine deficiency. Sherwin Badihian, M.D. has no disclosures. John H. Pula, M.D. has no disclosures. Alexander A. Tarnutzer, M.D. had no disclosures. David E. Newman-Toker, M.D., PhD Evaluates media legal cases and conducts funded research related to dizziness and stroke diagnosis. He had equipment leases by two commercial companies: Otometrics and Interacoustic. David S. Zee has no disclosures.
Ethical approval
This study is part of an “on-going” prospective investigation of patients with acute vestibular syndrome. The study was approved by the University of Illinois College of Peoria IRB. We follow the tenets of the Declaration of Helsinki.
Electronic supplementary material
Below is the link to the electronic supplementary material.
415_2020_10100_MOESM1_ESM.mp4
Supplementary file1Video 1 (patient 12, Table 1). Video obtained from a patient with a left dorsolateral medullary-cerebellar stroke. The first section obtained during the acute stroke phase shows an OLD to the left with brief eyelid closure and corrective hypometric saccades to the right on opening the eyes. The second section, obtained three months later show oblique saccades, as the patient refixate between vertical targets. The trajectory of these vertical saccades shows ipsilesional, horizontal lateropulsion. Horizontal saccades (not shown) were hypermetric to the left and hypometric to the right. The patient also a left head tilt. (MP4 75369 kb)
415_2020_10100_MOESM2_ESM.docx
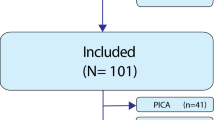
Supplementary file2Supplementary Table1. Clinical findings in lateral medullary syndrome without OLD. Supplementary table 2. Previous literature describing location of lesions with OLD, cause, fixation block technique and clinical course. Supplementary Figure 1 OLD Study Diagram: The Diagram provides a graphic comparison between HINTS/HINTS plus (associated with hearing loss) and OLD in AVS patients. Supplementary Figure 2 Axial DWI MRI in the patient with left-sided pontine stroke (Patient 3, see also Table 1). The left panel illustrates the rostral extent of the infarction, partially affecting the left superior cerebellar peduncle (SCP), and the right panel shows the caudal extent of the infarction including partial DWI signal in the flocculus. The middle panels show restricted signal in the left pons. (DOCX 2852 kb)
Rights and permissions
About this article
Cite this article
Kattah, J.C., Badihian, S., Pula, J.H. et al. Ocular lateral deviation with brief removal of visual fixation differentiates central from peripheral vestibular syndrome. J Neurol 267, 3763–3772 (2020). https://doi.org/10.1007/s00415-020-10100-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-10100-5