Abstract
Neuroinflammation (microglial activation) and subclinical nigrostriatal dysfunction have been reported in subjects at risk of Parkinsonism. Eight non-manifesting carriers (NMCs) of LRRK2 G2019S mutation had 11C-PK11195 and 18F-DOPA PET to assess microglial activation and striatal dopamine system integrity, respectively. Comparisons were made with healthy controls. Five LRRK2-NMCs had subclinical reductions of putaminal 18F-DOPA uptake. Three of them had significantly raised nigral 11C-PK11195 binding bilaterally. These findings indicate that nigrostriatal dysfunction and neuroinflammation occur in LRRK2-NMCs. Studies in larger cohorts with appropriate follow-up are needed to elucidate the significance of neuroinflammation in the premotor phase of LRRK2-PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mutations in the leucine-rich repeat kinase 2 gene (LRRK2) are known to cause inherited Parkinson’s disease (PD). LRRK2-associated PD (LRRK2-PD) presents with a low penetrant autosomal-dominant inheritance pattern with a cumulative risk of developing PD ranging from 26 to 80% at the age of 80 years [1, 2]. Patients with the G2019S mutation, the most common mutation in LRRK2-PD, are clinically indistinguishable from idiopathic PD and most cases present similar pathological findings with degeneration of dopaminergic neurons in the substantia nigra and occurrence of Lewy-type α-synuclein pathology [3]. Studying non-manifesting carriers (NMCs) of the LRRK2 G2019S mutation provides an opportunity to identify pathophysiological processes occurring in the premotor phase of genetic PD. This is essential to identify biomarkers and therapeutic targets to halt disease progression.
Microglia, the major resident immune cells of the central nervous system, monitors the brain milieu in their resting physiologic state, but when activated by injury, they can express both neuroprotective and cytotoxic phenotypes. It is hypothesized that a pro-inflammatory phenotype, leading to neuronal dysfunction, may drive neurodegeneration [4]. Microglial activation has been observed in idiopathic PD [5], but its role in the pathophysiology of genetic PD is unknown. A recent study using positron emission tomography (PET) imaging demonstrated increased microglial activation in the substantia nigra along with putaminal dopaminergic dysfunction in patients with idiopathic rapid eye movement sleep behavior disorder [6], a condition that may progress over time to a neurodegenerative alpha-synucleinopathy [7].
The present study aimed to investigate whether raised levels of microglial activation and alterations of the nigrostriatal dopaminergic function occur as well in LRRK2-NMCs.
Methods
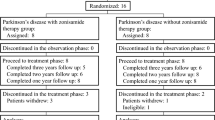
Eight LRRK2-NMCs were recruited from Hospital Clínic de Barcelona between September 2016 and May 2018. Inclusion of LRRK2-NMC was based on the absence of Parkinsonism and availability to perform the study. All NMC had a 60.5-min 11C-(R)-PK11195 PET scan (ECAT HRRT; CTI/Siemens, Knoxville, TN, USA) to assess levels of microglial activation (expressing 18-kDa translocator protein) and a 94.5-min 18F-DOPA PET scan to assess the integrity of the dopaminergic system. Each subject had a T1-weighted MRI (3 T MAGNETOM Skyra, Siemens Healthcare, Germany) performed for co-registration of PET images. PET findings were compared with those of 29 healthy controls (11C-PK11195 PET n = 20, 18F-DOPA PET n = 9). Control PET scans were acquired for two former projects using the exact same scanner and scan protocols [6, 8]. All participants were examined to exclude Parkinsonism. Assessments with the MDS-UPDRS part III, and Mini-Mental State Examination were also performed. All the assessments of this study were performed at the Department of Nuclear Medicine and PET Centre, Aarhus University Hospital.
Volumes of interest (VOI) sampled included the substantia nigra (11C-PK11195 PET only) plus putamen and caudate nucleus for both PET tracers. Image analysis was performed as previously described [6]. Briefly, parametric images of 11C-PK11195 binding potentials (BPND) were generated using a simplified reference tissue model with an individual tissue non-specific input function extracted with a supervised cluster-analysis approach. Similarity between the 11C-PK11195 reference input function extracted from LRRK2-NMCs and controls was confirmed with a repeated measurement analysis (χ2 test, p > 0.05). In those VOI’s where 11C-PK11195 binding is lower than that of the selected reference tissue voxels, this model computes a negative BPND. 18F-DOPA influx constant (Ki) images were generated using the Patlak graphical approach with the occipital lobe as the non-specific uptake reference region.
Group differences in 11C-PK11195 BPnd and 18F-DOPA Ki were interrogated with unpaired Student’s t test (p < 0.05), normal distribution of data was checked with normal probability plots and D’Agostino–Pearson normality test. For descriptive purposes, individually raised regional 11C-PK11195 binding and reduced regional 18F-DOPA uptake was defined as a statistically significant deviation from the controls mean value (left and right side averaged) of two or more standard deviations (z score ≥ 2 and z score ≤ − 2). Statistical analysis and graphical presentations were performed in Stata IC 14.2 (StataCorp LP, TX, USA) and GraphPad Prism 8 (GraphPad Software, La Jolla, CA, USA).
Results
Eight LRRK2-NMCs, 7 men, with a mean UPDRS part III score of 2.6 (SD;1.6) and a mean age of 55.8 years (range 39.8–73.4), were compared to 20 11C-PK11195 controls (12 men, mean age 66.8 years, range 58–80) and 9 18F-DOPA controls (9 men, mean age 64.6 years, range 59.9–69.5). The left–right averaged putaminal 18F-DOPA uptake was significantly (p = 0.006) reduced by − 9.2% (range − 16.9% to 4.7%) in LRRK2-NMCs compared to controls, while caudate 18F-DOPA uptake was similar (p = 0.468). No group differences were observed in VOI analysis with 11C-PK11195 PET (substantia nigra p = 0.075, putamen p = 0.678, caudate nucleus p = 0.695).
Five out of eight LRRK2-NMCs had reduced18F-DOPA uptake in putamen (z score ≤ − 2), four unilateral and one bilateral (Table 1; Fig. 1). Three out of eight LRRK2-NMC had bilaterally raised levels of 11C-PK11195 binding in the substantia nigra (z score ≥ 2), coincidental with unilaterally reduced putaminal 18F-DOPA uptake (z score ≤ − 2) in two and bilaterally reduced in one (Table 1; Fig. 1). One subject had unilateral raised putaminal 11C-PK11195 binding without ipsilateral reduced putaminal 18F-DOPA uptake (Table 1).
18F-DOPA uptake in putamen and ipsilateral 11C-PK11195 binding in substantia nigra in non-manifesting LRRK2 G2019S carriers. Values from left and right side in eight non-manifesting LRRK2 G2019S carriers are depicted. ⨂ indicates significantly reduced 18F-DOPA Ki values, which are two or more standard deviations below the average mean of controls (z score ≤ − 2). Red colour indicates significantly raised 11C-PK11195 BPND two or more standard deviations above the average mean of controls (z score ≥ 2). Observations from each individual carrier are marked with numbers from one to eight, which corresponds to their number in Table 1, individual analysis
Discussion
This PET imaging study performed in LRRK2-NMCs found reduced putaminal 18F-DOPA uptake in five out of eight LRRK2-NMCs as previously reported in subjects without manifest PD carrying different subtypes of LRRK2 mutations [9]. Three carriers in our cohort had bilaterally raised substantia nigra 11C-PK11195 binding, indicating microglial activation, together with reductions in putaminal 18F-DOPA uptake (unilaterally reduced in two subjects and bilaterally in one). To our knowledge, this is the first report of activated microglia in LRRK2-NMC.
While not in all cases, a reduced putaminal 18F-DOPA uptake without increased ipsilateral nigral 11C-PK11195 binding was observed (subject 4 and 5; Fig. 1), suggesting that in LRRK2-NMC, dysfunction of putaminal dopaminergic axonal terminals may antedate microglial activation in nigral cell bodies, presumed to be related with neurodegeneration [4]. A similar pattern (normal range substantia nigra 11C-PK11195 binding and reduced ipsilateral putaminal 18F-DOPA uptake) has been reported previously in occasional subjects with prodromal PD [6] and manifest idiopathic PD patients [5]. The significance of microglial activation in the pathophysiology of PD is yet to be established. The findings in the current study, together with those found in a previous one examining prodromal PD [6] support the concept that similar alterations occur in the premotor phase in both genetic and idiopathic forms of the disease. Microglial cells are able to express either a neuroprotective or a cytotoxic phenotype [4]. Which of these is occurring in the examined LRRK2-NMC can only be determined with PET tracers binding specifically to each microglia phenotype; however, this kind of in vivo tracer is currently not available.
There are limitations to this study to be considered. First, the small number of cases examined may preclude the generalization of the results. Second, the LRRK2-NMC included in this study are younger than the controls which may account for a selection bias. Considering the age-related and low and penetrance of LRRK2 G20109S mutation [1, 2], it is possible that we have studied subjects who will never develop PD or at a very early phase of the disease when biochemical and pathological events have not yet started [10]. However, the alteration of 18F-DOPA PET in five LRRK2-NMC indicates that in most of LRRK-NMC in this cohort, pathological changes are already occurring. Given that age is the greatest risk factor for developing LRRK2-PD, we investigated whether PET findings were more likely to occur in the eldest LRRK2-NMC. We found that age did not correlate with PET alterations in the studied cohort, suggesting that other factors may influence 18F-DOPA dysfunction and microglial activation (individual data including age, not shown to avoid subject identification). Third, as previously reported in animal models [11], levels of microglial activation in PD may be influenced by the presence of pathological α-synuclein inclusions. In LRRK2 G2019S PD, a pleiotropic neuropathology has been reported, including subjects without Lewy-type α-synuclein pathology [3, 12]. This pathological variability may possibly influence the heterogeneity of the results. Finally, 11C-PK11195 may not only bind to the 18-kDa translocator protein located on mitochondria inside the activated microglial cells but also on astrocytes; however, observations show that this only accounts for minor degree of 11C-PK11195 signal [13].
This is the first study performed in LRRK2-NMCs showing dopamine dysfunction in five out of eight subjects and concomitant nigral microglial activation in three of them. These results suggest that PET imaging with 18F-DOPA and 11C-PK11195 could help identify NMCs with ongoing nigrostriatal pathology and show that at least in some cases, neuroinflammation could play a role in the pathophysiology of early phases of LRRK2-PD. The contribution of the observed in vivo microglial response and its clinical relevance at individual level still needs to be elucidated. Prospective studies using similar PET tracers in a larger study population with appropriate clinical follow-up may clarify these issues.
References
Healy DG, Falchi M, O'Sullivan SS, Bonifati V, Durr A, Bressman S, Brice A, Aasly J, Zabetian CP, Goldwurm S, Ferreira JJ, Tolosa E, Kay DM, Klein C, Williams DR, Marras C, Lang AE, Wszolek ZK, Berciano J, Schapira AH, Lynch T, Bhatia KP, Gasser T, Lees AJ, Wood NW, L.C. International (2008) LC International, Phenotype, genotype, and worldwide genetic penetrance of LRRK2-associated Parkinson's disease: a case–control study. Lancet Neurol 7(7):583–590
Marder K, Wang Y, Alcalay RN, Mejia-Santana H, Tang MX, Lee A, Raymond D, Mirelman A, Saunders-Pullman R, Clark L, Ozelius L, Orr-Urtreger A, Giladi N, Bressman S, L.A.J. Consortium (2015) Age-specific penetrance of LRRK2 G2019S in the Michael J. Fox Ashkenazi Jewish LRRK2 Consortium. Neurology 85(1):89–95
Kalia LV, Lang AE, Hazrati LN, Fujioka S, Wszolek ZK, Dickson DW, Ross OA, Van Deerlin VM, Trojanowski JQ, Hurtig HI, Alcalay RN, Marder KS, Clark LN, Gaig C, Tolosa E, Ruiz-Martinez J, Marti-Masso JF, Ferrer I, Lopez de Munain A, Goldman SM, Schule B, Langston JW, Aasly JO, Giordana MT, Bonifati V, Puschmann A, Canesi M, Pezzoli G, Maues De Paula A, Hasegawa K, Duyckaerts C, Brice A, Stoessl AJ, Marras C (2015) Clinical correlations with Lewy body pathology in LRRK2-related Parkinson disease. JAMA Neurol 72(1):100–105
Ransohoff RM (2016) How neuroinflammation contributes to neurodegeneration. Science 353(6301):777–783
Gerhard A, Pavese N, Hotton G, Turkheimer F, Es M, Hammers A, Eggert K, Oertel W, Banati RB, Brooks DJ (2006) In vivo imaging of microglial activation with [11C](R)-PK11195 PET in idiopathic Parkinson's disease. Neurobiol Dis 21(2):404–412
Stokholm MG, Iranzo A, Ostergaard K, Serradell M, Otto M, Svendsen KB, Garrido A, Vilas D, Borghammer P, Santamaria J, Moller A, Gaig C, Brooks DJ, Tolosa E, Pavese N (2017) Assessment of neuroinflammation in patients with idiopathic rapid-eye-movement sleep behaviour disorder: a case–control study. Lancet Neurol 16(10):789–796
Iranzo A, Tolosa E, Gelpi E et al (2013) Neurodegenerative disease status and post-mortem pathology in idiopathic rapid-eye-movement sleep behaviour disorder: an observational cohort study. Lancet Neurol 12(5):443–453
Parbo P, Ismail R, Hansen KV, Amidi A, Marup FH, Gottrup H, Braendgaard H, Eriksson BO, Eskildsen SF, Lund TE, Tietze A, Edison P, Pavese N, Stokholm MG, Borghammer P, Hinz R, Aanerud J, Brooks DJ (2017) Brain inflammation accompanies amyloid in the majority of mild cognitive impairment cases due to Alzheimer's disease. Brain 140(7):2002–2011
Wile DJ, Agarwal PA, Schulzer M, Mak E, Dinelle K, Shahinfard E, Vafai N, Hasegawa K, Zhang J, McKenzie J, Neilson N, Strongosky A, Uitti RJ, Guttman M, Zabetian CP, Ding YS, Adam M, Aasly J, Wszolek ZK, Farrer M, Sossi V, Stoessl AJ (2017) Serotonin and dopamine transporter PET changes in the premotor phase of LRRK2 parkinsonism: cross-sectional studies. Lancet Neurol 16(5):351–359
Salat D, Noyce AJ, Schrag A, Tolosa E (2016) Challenges of modifying disease progression in prediagnostic Parkinson's disease. Lancet Neurol 15(6):637–648
Peelaerts W, Bousset L, Van der Perren A, Moskalyuk A, Pulizzi R, Giugliano M, Van den Haute C, Melki R, Baekelandt V (2015) alpha-Synuclein strains cause distinct synucleinopathies after local and systemic administration. Nature 522(7556):340–344
Schneider SA, Alcalay RN (2017) Neuropathology of genetic synucleinopathies with parkinsonism: review of the literature. Mov Disord 32(11):1504–1523
Venneti S, Lopresti BJ, Wiley CA (2006) The peripheral benzodiazepine receptor (translocator protein 18 kDa) in microglia: from pathology to imaging. Prog Neurobiol 80(6):308–322
Acknowledgements
We thank all study participants and biomedical laboratory scientists and radiochemists (Department of Nuclear Medicine and PET Centre, Aarhus University Hospital, Denmark) for technical assistance, and our study coordinator Anne Sofie Møller Andersen (Danish Neuroscience Centre, Aarhus University, Denmark).
Funding
The Independent Research Fund Denmark.
Author information
Authors and Affiliations
Contributions
Study design: NP, ET, MGS, and AG. Data acquisition: MGS, AG, MS, PP, KS, MJM, and NP. All authors contributed to data analyses and the writing of the manuscript. We confirm that all authors have contributed to this work, and have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
ET reports grants from the MJFox Foundation and the Instituto de Salud Carlos III. KØ reports grants from The Danish Parkinson Association, The Danish Council for Independent Research, and Lundbeck Foundation, during the conduct of the study and personal fees from Medtronic Inc., UCB, Fertin Pharma, and AbbVie outside the submitted work. DJB reports grants from The Danish Council for Independent Research, Lundbeck Foundation, The Danish Parkinson Association, European Union FP7 programme, and Alzheimer Research UK and personal fees from GE Healthcare and Plexxikon outside the submitted work. NP reports grants from The Danish Council for Independent Research during the conduct of the study. The other authors declare no competing interests.
Ethical approval
The local Ethics Committee at both centres, Aarhus and Barcelona, approved the study and all participants gave written informed consent according to the Declaration of Helsinki before study enrollment.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gersel Stokholm, M., Garrido, A., Tolosa, E. et al. Imaging dopamine function and microglia in asymptomatic LRRK2 mutation carriers. J Neurol 267, 2296–2300 (2020). https://doi.org/10.1007/s00415-020-09830-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09830-3