Abstract
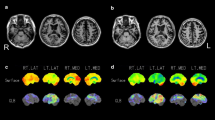
The logopenic variant of primary progressive aphasia (lvPPA) has been associated with Alzheimer disease, although this relationship is still subject to debate. The purpose of this study is to determine the frequency of amyloid biomarkers in patients with lvPPA, and record any potential clinical or topographic differences between patients with and without amyloid deposits. We conducted cognitive examination and positron-emission tomography studies with fluorodeoxyglucose (18F) and florbetapir (18F) in a cohort of 16 patients diagnosed with lvPPA. We evaluated the prevalence of amyloid deposits as well as any clinical and metabolic differences between the groups with and without significant presence of amyloid deposits. Eleven patients (69 %) were considered amyloid-positive. The amyloid-positive group displayed less metabolic activity in the left temporoparietal region than the control group, while the amyloid-negative group showed lower metabolism in the left temporoparietal region extending to the anterior temporal and basal frontal regions. The percentage of change in patients with clinical and FDG-PET follow-up did not differ between the amyloid-positive and amyloid-negative subgroups. The frequency of amyloid-positive cases confirms that lvPPA is frequently associated with Alzheimer disease. Amyloid-negative patients show a different cerebral metabolic pattern. These findings show the relevance of using amyloid PET to study lvPPA, and also suggest that the logopenic variant may not be specific to Alzheimer disease in certain cases.





Similar content being viewed by others
References
Mesulam MM, Rogalski EJ, Wieneke C, Hurley RS, Geula C, Bigio EH, Thompson CK, Weintraub S (2014) Primary progressive aphasia and the evolving neurology of the language network. Nat Rev Neurol. doi:10.1038/nrneurol.2014.159
Matías-Guiu JA, García-Ramos R (2013) Primary progressive aphasia: from syndrome to disease. Neurologia 28:366–374
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, Mohs RC, Morris JC, Rossor MN, Scheltens P, Carrillo MC, Thies B, Weintraub S, Phelps CH (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the Nations Institute on Aging-Alzheimer’s Association Workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7:263–269
Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, Ogar JM, Rohrer JD, Black S, Boeve BF, Manes F, Dronkers NF, Vandenberghe R, Rascovsky K, Patterson K, Miller BL, Knopman DS, Hodges JR, Mesulam MM, Grossman M (2011) Classification of primary progressive aphasia and its variants. Neurology 76:1006–1014
Matias-Guiu JA, Cabrera-Martín MN, García-Ramos R, Moreno-Ramos T, Valles-Delgado M, Carreras JL, Matias-Guiu J (2014) Evaluation of the new consensus criteria for the diagnosis of primary progressive aphasia using fluorodeoxyglucose positron emission tomography. Dement Geriatr Cogn Disord 38:147–152
Diehl-Schmid J, Onur OA, Kuhn J, Gruppe T, Drzezga A (2014) Imaging frontotemporal lobar degeneration. Curr Neurol Neurosci Rep 14:489
Rabinovici GD, Jagsut WJ, Furst AJ, Ogar JM, Racine CA, Mormino EC, O’Neil JP, Lal RA, Dronkers NF, Miller BL, Gorno-Tempini ML (2008) Aβ amyloid and glucose metabolism in three variants of primary progressive aphasia. Ann Neurol 64:388–401
Leyton CE, Villemagne VL, Savage S, Pike KE, Ballard KH, Piguet O, Burrell JR, Rowe CC, Hodges JR (2011) Subtypes of progressive aphasia: application of the international consensus criteria and validation using beta-amyloid imaging. Brain 134:3030–3043
Mendez MF, Sabodash V (2013) Clinical amyloid imaging in logopenic progressive aphasia. Alzheimer Dis Assoc Disord. doi:10.1097/WAD.0b013e3182a683de
Teichmann M, Kas A, Boutet C, Ferrieux S, Nogues M, Samri D, Rogan C, Dormont D, Dubois B, Migliaccio R (2013) Deciphering logopenic primary progressive aphasia: a clinical, imaging and biomarker investigation. Brain 136:3474–3488
Whitwell JL, Duffy JR, Strand EA, Machuda MM, Senjem ML, Schwarz CG, Reid R, Baker MC, Perkerson RB, Lowe VJ, Rademakers R, Jack CR Jr, Josephs KA (2015) Clinical and neuroimaging biomarkers of amyloid-negative logopenic primary progressive aphasia. Brain Lang 142C:45–53
Harris JM, Gall C, Thompson JC, Richardson AMT, Neary D, du Plessis D, Pal P, Mann DMA, Snowden JS, Jones M (2013) Classification and pathology of primary progressive aphasia. Neurology 81:1832–1839
Harris JM, Jones M (2014) Pathology in primary progressive aphasia syndromes. Curr Neurol Neurosci Rep 14:466
Herholz K, Ebmeier K (2011) Clinical amyloid imaging in Alzheimer’s disease. Lancet Neurol 10:667–670
Clark CM, Pontecorvo MJ, Beach TG, Bedell BJ, Coleman RE, Doraiswamy PM, Fleisher AS, Reiman EM, Sabbagh MN, Sadowsky CH, Schneider JA, Arora A, Carpenter AP, Flitter ML, Joshi AD, Krautkramer MJ, Lu M, Mintun MA, Skovronsky DM; AV-45-A-16 Study Group (2012) Cerebral PET with florbetapir compared with neuropathology at autopsy for detection of neuritic amyloid-beta plaques: a prospective cohort study. Lancer Neurol 11:669–678
Landau SM, Breault C, Joshi AD, Pontecorvo M, Mathis CA, Jagust WJ, Mintun MA, Alzheimer’s Disease Neuroimaging Initiative (2013) Amyloid-beta imaging with Pittsburgh compound B and florbetapir: comparing radiotracers and quantification methods. J Nucl Med 54:70–77
Landau SM, Thomas BA, Thurfjell L, Schmidt M, Margolin R, Mintun M, Pontecorvo M, Baker SL, Jagust WJ, Alzheimer’s Disease Neuroimaging Initiative (2014) Amyloid PET imaging in Alzheimer’s disease: a comparison of three radiotracers. Eur J Nucl Med Mol Imaging 41:1398–1407
Mathuranath PS, Nestor PJ, Berrios GE, Rakowicz W, Hodges JR (2000) A brief cognitive test battery to differentiate Alzheimer’s disease and frontotemporal dementia. Neurology 55:1613–1620
Goodglass H, Kaplan E, Barresi B (2001) Boston diagnostic aphasia examination, third edition (BDAE-3). Pro-Ed, Austin
Peña-Casanova J (1990). Programa integrado en la exploración neuropsicológica-test Barcelona. Manual. Integrated program of neuropsychological assessment—revised Barcelona test manual. Masson, Barcelona
Quintana M, Peña-Casanova J, Sánchez Benavides, Neuronorma Study Team et al (2011) Spanish multicenter normative studies (Neuronorma project): norms for the abbreviated Barcelona test. Arch Clin Neuropsychol 26:144–157
Sapolsky D, Bakkour A, Negreira A et al (2010) Cortical neuroanatomic correlated of symptom severity in primary progressive aphasia. Neurology 75:358–366
Joshi AD, Pontecorvo MJ, Clark CM, Carpenter AP, Jennings DL, Sadowsky CH, Adler LP, Kovnat KD, Seibyl JP, Arora A, Saha K, Burns JD, Lowrey MJ, Mintun MA, Skovronsky DM, Florbetapir F18 Study Investigators (2012) Performance characteristics of amyloid PET with florbetapir F 18 in patients with Alzheimer’s disease and cognitively normal subjects. J Nucl Med 53:378–384
Herholz K, Evans R, Anton-Rodriguez J, Hinz R, Matthews JC (2014) The effect of 18F-florbetapir dose reduction on region-based classification of cortical amyloid deposition. Eur J Nucl Med Mol Imaging 41:2144–2149
Clark CM, Pontecorvo MJ, Beach TG, Bedell BJ, Coleman RE, Doraiswamy PM, Fleisher AS, Reiman EM, Sabbagh MN, Sadowsky CH, Schneider JA, Arora A, Carpenter AP, Flitter ML, Joshi AD, Krautkramer MJ, Lu M, Mintum MA, Skovronsky DM; AV-45-A16 Study Group (2012) Cerebral PET with florbetapir compared with neuropathology at autopsy for detection of neuritic amyloid-β plaques: a prospective cohort study. Lancet Neurol 11:669–678
Ashburner J, Friston KJ (2000) Voxel-based morphometry: the methods. Neuroimage 11:805–821
Tzourio-Mazoyer N, Landeau D, Papathanassiou D, Crivello F, Etard O, Delcroix N, Mazoyer B, Joliot M (2002) Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. NeuroImage 15:273–289
Fleisher AS, Chen K, Roontiva A, Thyyagura P, Ayutyanont N, Joshi AD, Clark CM, Mintum MA, Pontecorvo MJ, Doraiswamy PM, Johnson KA, Skovronsky DM, Reiman EM (2011) Using positron emission tomography and florbetapir F18 to image cortical amyloid in patients with mild cognitive impairment or dementia due to Alzheimer disease. Arch Neurol 68:1404–1411
Gorno-Tempini ML, Dronkers NF, Rankin KP, Ogar JM, Phengrasamy L, Rosen HJ, Johnson JK, Weiner MW, Miller BL (2004) Cognition and anatomy in three variants of primary progressive aphasia. Ann Neurol 55:335–346
Matías-Guiu JA, Cabrera-Martín MN, Moreno-Ramos T, García-Ramos R, Porta-Etessam J, Carreras JL, Matías-Guiu J (2015) Clinical course of primary progressive aphasia: clinical and FDG-PET patterns. J Neurol 262:570–577
Zhang S, Smailagic N, Hyde C, Noel-Storr AH, Takwoingi Y, McShane R, Feng J (2014) (11)C-PIB-PET for the early diagnosis of Alzheimer’s disease dementia and other dementias in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev 7:CD010386
Jack CRJR, Wiste HJ, Weigand SD, Rocca WA, Knopman DS, Mielke MM, Lowe VJ, Senjem ML, Gunter JL, Preboske GM, Pankratz VS, Vemuri P, Petersen RC (2014) Age-specific population frequencies of cerebral beta-amyloidosis and neurodegeneration among people with normal cognitive function aged 50-89 years: a cross-sectional study. Lancet Neurol 13:997–1005
Leyton CE, Ballard KJ, Piguet O, Hodges JR (2014) Phonologic errors as a clinical marker of the logopenic variant of PPA. Neurology 82:1620–1627
Leyton CE, Hodges JR (2013) Towards a clearer definition of logopenic progressive aphasia. Curr Neurol Neurosci Rep 13:396
Leyton CE, Hsieh S, Mioshi E, Hodges JR (2013) Cognitive decline in logopenic aphasia. More than losing words. Neurology 80:897–903
Josephs KA, Duffy JR, Strand EA, Machulda MM, Vemuri P, Senjem ML, Perkerson RB, Baker MC, Lowe V, Jack CR Jr, Rademakers R, Whitwell JL (2014) Progranulin-associated PiB-negative logopenic primary progressive aphasia. J Neurol 261:604–614
Matias-Guiu JA, García-Azorín D, García-Ramos R, Basoco E, Elvira C, Matías-Guiu J (2014) Study of outpatient neurological care in the Region of Madrid: the impact of implementing free choice of hospital. Neurologia. doi:10.1016/j.nrl.2014.04.005
Whitwell JL, Lowe VJ, Duffy JR, Strand EA, Machulda MM, Kantarci K, Wille SM, Senjem ML, Murphy MC, Gunter JL, Jack CR Jr, Josephs KA (2013) Elevated occipital β-amyloid deposition is associated with widespread cognitive impairment in logopenic progressive aphasia. J Neurol Neurosurg Psychiatry 84:1357–1364
Acknowledgments
The authors would like to thank Spanish Society of Neurology’s Research Operations Office staff for their help in preparing this manuscript.
Conflicts of interest
The authors have no conflicts of interest to declare.
Ethical standard
The study was approved by the research committee at our hospital and conducted in accordance with the 1964 Helsinki Declaration and its later amendments.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
415_2015_7738_MOESM1_ESM.pptx
Fig. 1. Cortical regions of interest used for analysis of the uptake florbetapir (18F). Numbers represent z-coordinates. (PPTX 1004 kb)
415_2015_7738_MOESM2_ESM.pdf
Table 1 Cortico-cerebellar standardized uptake value ratios for florbetapir (18F). (PDF 56 kb)
415_2015_7738_MOESM3_ESM.pdf
Table 2 Voxel-based analysis results. Coordinates and statistical data from the following analyses of brain metabolism: 1) lvPPA < healthy controls; 2) amyloid-positive lvPPA < healthy controls; 3) amyloid-negative lvPPA < healthy controls; 4) amyloid-positive lvPPA < amyloid-negative lvPPA; 5) amyloid-negative lvPPA < amyloid-positive lvPPA. (PDF 79 kb)
Rights and permissions
About this article
Cite this article
Matías-Guiu, J.A., Cabrera-Martín, M.N., Moreno-Ramos, T. et al. Amyloid and FDG-PET study of logopenic primary progressive aphasia: evidence for the existence of two subtypes. J Neurol 262, 1463–1472 (2015). https://doi.org/10.1007/s00415-015-7738-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-7738-z