Abstract
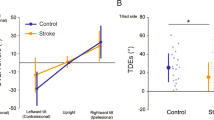
Unilateral stroke can lead to a disorder of postural balance that manifests as a pushing away toward the contralesional side. It is called “pusher syndrome” (PS). The aims of this study were first to assess the anatomical cortical regions that induce PS and second to clarify whether tilt of the subjective visual vertical (SVV)—a sign of vestibular otolith dysfunction—is associated with PS. Sixty-six patients with acute unilateral strokes (28 left-sided lesions, 38 right-sided lesions) were tested for PS, for tilts of the SVV, for hemineglect and for the anatomical lesion site by magnetic resonance imaging (MRI)-based voxelwise lesion-behavior mapping analysis. Our data indicated no significant voxels; however, there was a trend towards an association between lesions of the posterior part of the insula, the operculum and the superior temporal gyrus—key areas of the multisensory vestibular cortical network—and the extent of pushing in patients with right-sided lesions, whereas the rather anterior part of the insula, the operculum as well as the internal capsule reaching to the lateral thalamus seemed to be involved in PS in left-sided lesion patients. These data might point toward a link between the systems responsible for postural control and for processing vestibular otolith information. These findings indicate that vestibular information might be fundamental in right-sided lesion patients for maintaining body posture in space.



Similar content being viewed by others
References
Karnath HO, Ferber S, Dichgans J (2000) The origin of contraversive pushing. Evidence for a second graviceptive system in humans. Neurology 55:1298–1304
Karnath HO, Johannsen L, Broetz D, Küker W (2005) Posterior thalamic hemorrhage induces “pusher syndrome”. Neurology 64:1014–1019
Johannsen L, Broetz D, Naegele T, Karnath HO (2006) “Pusher syndrome” following cortical lesions that spare the thalamus. J Neurol 253:455–463
Ticini LF, Klose U, Naegele T, Karnath HO (2009) Perfusion imaging in pusher syndrome to investigate the neural substrates involved in controlling upright body position. PLoS ONE 4:e5737. doi:10.1371/journal.pone.0005737
Saj A, Honoré J, Coello Y, Rousseaux M (2005) The visual vertical in the pusher syndrome. Influence of hemispace and body position. J Neurol 252:885–891
Johannsen L, Fruhmann Berger M, Karnath HO (2006) Subjective visual vertical (SVV) determined in a representative sample of 15 patients with pusher syndrome. J Neurol 253:1367–1369
Baccini M, Paci M, Nannetti L, Biricolti C, Rinaldi LA (2008) Scale for contraversive pushing: cutoff scores for diagnosing “pusher behavior” and construct validity. Phys Ther 88:947–955
Fels M, Geissner E (1987) Neglect-Test (NET). Ein Verfahren zur Erfassung visueller Neglectphänomene. Hogrefe-Verlag, Göttingen, Bern
Wilson B, Cockburn J, Halligan PW (1987) Behavioural inattention test. Thames Valley Company, Titchfield, Hants
Rorden C, Karnath HO (2010) A simple measure of neglect severity. Neuropsychologia 48:2758–2763
Baier B, Bense S, Dieterich M (2008) Are signs of ocular tilt reaction in patients with cerebellar lesions mediated by the dentate nucleus? Brain 131:1445–1454
Dieterich M, Brandt T (1993) Ocular torsion and tilt of subjective visual vertical are sensitive brainstem signs. Ann Neurol 33:292–299
Rorden C, Karnath HO, Bonilha L (2007) Improving lesion-symptom mapping. J Cogn Neurosci 19:1081–1088
Rorden C, Fridriksson J, Karnath HO (2009) An evaluation of traditional and novel tools for lesion behavior mapping. Neuroimage 44:1355–1362
Bense S, Stephan T, Yousry TA, Brandt T, Dieterich M (2001) Multisensory cortical signal increases and decreases during vestibular galvanic stimulation (fMRI). J Neurophysiol 85:886–899
Dieterich M, Brandt T (1993) Thalamic infarctions: differential effects on vestibular function in the roll plane (35 patients). Neurology 43:1732–1740
Dieterich M, Brandt T (1990) Postural imbalance and subjective visual vertical in medullary Infarctions. In: Brandt T (ed) Disorders of posture and gait. Thieme, Stuttgart, New York, pp 419–422
Brandt T, Dieterich M, Danek A (1994) Vestibular cortex lesions affect the perception of verticality. Ann Neurol 35:403–412
Shelley BP, Trimble MR (2004) The insular lobe of Reil—its anatomico-functional, behavioural and neuropsychiatric attributes in humans—a review. World J Biol Psychiatry 5:176–200
Karnath H-O, Broetz D (2003) Understanding and treating “pusher syndrome”. Phys Ther 83:1119–1125
Pedersen PM, Wandel A, Jorgensen HS et al (1996) Ipsilateral pushing in stroke: incidence, relation to neuropsychological symptoms, and impact on rehabilitation—the Copenhagen stroke study. Arch Phys Med Rehabil 77:25–28
Acknowledgments
Supported by the Deutsche Forschungsgemeinschaft (BA 4097/1-1) to BB. We thank Anja Schröer and the physiotherapists for data assessment.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
B. Baier and J. Janzen contributed equally to the study.
Rights and permissions
About this article
Cite this article
Baier, B., Janzen, J., Müller-Forell, W. et al. Pusher syndrome: its cortical correlate. J Neurol 259, 277–283 (2012). https://doi.org/10.1007/s00415-011-6173-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6173-z