Abstract
Patients with Parkinson’s disease (PD) are likely to become physically inactive, because of their motor, mental, and emotional symptoms. However, specific studies on physical activity in PD are scarce, and results are conflicting. Here, we quantified daily physical activities in a large cohort of PD patients and another large cohort of matched controls. Moreover, we investigated the influence of disease-related factors on daily physical activities in PD patients. Daily physical activity data of PD patients (n = 699) were collected in the ParkinsonNet trial and of controls (n = 1,959) in the Longitudinal Aging Study Amsterdam (LASA); data were determined using the LAPAQ, a validated physical activity questionnaire. In addition, variables that may affect daily physical activities in PD were recorded, including motor symptoms, depression, disability in daily life, and comorbidity. Patients were physically less active; a reduction of 29% compared to controls (95% CI, 10–44%). Multivariate regression analyses demonstrated that greater disease severity, gait impairment, and greater disability in daily living were associated with less daily physical activity in PD (R 2 = 24%). In this large study, we show that PD patients are about one-third less active compared to controls. While disease severity, gait, and disability in daily living predicted part of the inactivity, a portion of the variance remained unexplained, suggesting that additional determinants may also affect daily physical activities in PD. Because physical inactivity has many adverse consequences, work is needed to develop safe and enjoyable exercise programs for patients with PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with Parkinson’s disease (PD) are likely to experience a decrease in their daily physical activity, because of physical impairments, fatigue, and apathy. Such a sedentary lifestyle is undesirable, because physical inactivity is a risk factor for cardiovascular disease, diabetes mellitus, cognitive impairment, osteoporosis, and depression [40]. Moreover, physical inactivity may worsen various nonmotor symptoms, such as insomnia and constipation.
Thus far, only a few studies have examined physical activity in PD, and the results were inconsistent. Several studies found reduced levels of physical activity, but activity levels were not assessed optimally (either indirectly using visual analogous scales [12], or using activity monitors mounted at the wrist, rather than the leg [37]), or studies were very small [5, 35]. Unexpectedly, two studies found that patients and controls spent comparable amounts of time being active [7, 29].
The determinants of physical activity in PD remain incompletely understood [11]. Generic factors such as age [16], gender [6, 16], and health status [16] are associated with the level of physical activity in healthy adults. Furthermore, depression is a risk factor for developing a sedentary lifestyle [30]. Such factors may also affect exercise behavior in patients with PD. Identifying the determinants of physical activity may help to structure new exercise interventions.
Here, we quantified daily physical activities in a large group of PD patients and analyze the associated determinants, using data from the ParkinsonNet trial (699 patients) [24, 25] and the population-based LASA study (1,959 controls) [10].
Methods
Participants
Patients
The ParkinsonNet trial was a cluster randomized trial involving 699 participants that evaluated community-based professional networks of physiotherapists (ParkinsonNet) [24, 25]. Eligibility criteria for patients were the following: (a) PD according to the UK PDS Brain Bank criteria [13]; (b) living independently in the community; (c) <80 years old; (d) able to complete the questionnaires; (e) MMSE >23; and (f) no severe comorbidity interfering with daily functioning. Stage of the disease was scored according to the original Hoehn and Yahr (H&Y) stages [17]. Most patients (81.6%) had moderate disease severity (i.e., H&Y 2–3; Table 1). Mean age was 68.6 ± 7.7 years, 409 patients were men (58.5%), and average disease duration was 5.3 years. Full ethical approval has been granted for the study. All patients signed informed consent. In the study described here, we used baseline data.
Controls
Controls were derived from the Longitudinal Aging Study Amsterdam (LASA), a prospective study of persons aged 55–85 years old (1995–1996) [10]. This cohort forms a nationally representative sample of the older Dutch population and, thus, creates a good control group. After exclusion of participants older than 80 years, data of 1,959 controls were available for the analyses. Mean age was 65.8 ± 7.0 years and 921 subjects were men (47.0%) (Table 1). Full ethical approval has been granted for the study and all respondents gave informed consent at the start of the study.
Daily physical activity in patients and controls
In both groups, daily physical activity was measured with the LASA Physical Activity Questionnaire (LAPAQ) [33]. The LAPAQ covers frequency and duration of different activities during the previous 2 weeks [33, 39]. Activities covered in the LAPAQ include the following: walking outside, cycling, gardening, light and heavy household activities, and a maximum of two sport activities. To consider different levels of intensity of activities, a metabolic equivalent value (MET) was assigned to each activity to calculate the number of kilocalories spent per day per kilogram of body weight [1]. In addition, types of different activities (‘inside’ and ‘outside the house’) were specified.
The LAPAQ was initially designed as an interview-based physical activity questionnaire; in the LASA study, data were collected this manner. A self-completed version was used in the ParkinsonNet trial. To reduce recall bias, the time window was limited to 1 week. A random sample of the ParkinsonNet trial population (n = 76) completed the questionnaire and was also interviewed similar to the controls. The subgroup was comparable to the total PD population (Table 1).
Disease-related factors associated with daily physical activity in PD
In the ParkinsonNet trial, a wide range of variables were assessed: disease severity (H&Y stages and motor section of the unified Parkinson’s Disease Rating Scale [23]), fear of falling (Falls Efficacy Scale-International [34]), anxiety and depression (Hospital Anxiety and Depression Scale [21]), mobility (timed up and go test [22]), freezing of gait (Freezing of Gait questionnaire [14]), walking speed (6-m walk test), disability in daily life (Self-assessment Parkinson’s Disease Disability Scale [3]), comorbidity (cumulative illness rating scale [26]), and “faller status” (≥1 fall in the preceding year). Patient characteristics included gender, age, education level, and marital status. We studied the influence of these disease-related factors on daily physical activity. We classified six dimensions to analyze all factors: demographics (gender, age, education level, and marital status); health status/disease severity (H&Y, UPDRS, CIRS, and time since diagnosis); walking performance/mobility (TUG, FOGQ, and walking speed); fear of falling, anxiety, and depression (HADS and FES-I); disability in daily life (SPDDS); and faller status.
Analyses
Data of daily physical activity in both groups were summarized with medians and 25th and 75th percentiles. Since the LAPAQ scores were skewed, linear logarithmic transformation was applied for all subsequent analyses. Differences between patients and controls in minutes per day as well as in kilocalories per day were evaluated using linear regression analyses, with adjustment for gender, age, education level, and marital status. Furthermore, linear regression analysis with forward variable selection was performed to study the association between the dimensions mentioned above and daily physical activities. First, we used a stepwise selection procedure to identify additional variables that contributed significantly. In addition, we used a hierarchic approach whereby in each subsequent step of the selection procedure, an F test was performed for each dimension that was not yet in the model. First, the demographic variables were included in the model. The dimension with the smallest p value was then included, provided that it was statistically significant. The selection procedure was stopped when the F test of none of the remaining dimensions was significant. A two-sided p value of <0.05 was considered to indicate statistical significance. In general, selection procedures provide a model, but they do not guarantee that the model is unique. Therefore, we evaluated whether the resulting model was optimal and unique by calculating the explained variance (R 2) for all possible alternative models.
Results
Daily physical activity in PD compared to controls
Patients spent 111 min/day (interquartile range 58–206) on daily physical activity, compared to 150 min for controls (interquartile range 89–232). This amount led to a 29% reduction in patients versus controls (95% CI, 10–44%; p < 0.01). Patients also spent 29% fewer kilocalories during daily physical activity (95% CI, 11–43%; p < 0.01). After adjustment for age, gender, education level, and marital status, the difference between patients and controls was 24% (95% CI, 3–40%; p < 0.05). In contrast to the control group, the patient population included subjects younger than 55 years of age. Therefore, we performed an additional analysis excluding patients younger than 55 years old, which showed comparable results.
In a subanalysis, we specified the nature of activities. Median time spent to ‘outdoor and sports activities’ did not differ between patients and controls (95% CI, 79–150%). However, PD patients spent significantly less time to activities inside the house (62%; 95% CI, 45–83%; p < 0.01).
Disease-related factors associated with daily physical activities in PD
Univariate relationships
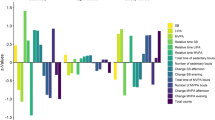
Univariate regression analyses were performed to investigate the relation between the various disease-related factors and daily physical activity in minutes per day (Table 2). All disease-related factors were significantly correlated with daily physical activity, except for ‘time since diagnosis’. Compared to men, women with PD were 80% more active. Furthermore, time spent on daily physical activity decreased significantly with age (−3% for each year) and with disease severity (−3% for each point on the UPDRS). Figure 1 shows that the time spent on daily physical activity decreased when disease severity increased. In addition, patients without falls in the preceding year spent 32% more time on daily activity compared to fallers. Greater fear of falling, comorbidity, and depression and anxiety were associated with less daily physical activity in PD.
Multivariate relationships
Stepwise model selection resulted in a model with four variables: gender, comorbidity, mobility, and disability in daily life (Table 2). This model explained 22% of the variance.
However, when we checked whether this model was unique, we found ten additional models leading to 21% explained variance. In addition, the model with three variables (gender, mobility, and disability in daily life) had an explained variance of 21%. All models with five or more variables explained at least 20% of the variance, whereas the percentage explained variance of the full model was 24%. We evaluated the possible collinearity in the full model. The largest collinearity index was 3.9 and the largest variance inflation factor (VIF) was 2.6. Only SPDDS and FES-I had a VIF exceeding 2.
Multivariate relationships: hierarchic approach
As we could not find a reasonably unique model in the multivariable approach, we used a hierarchic variable selection to identify dimensions which were associated with daily physical activity. Demographic characteristics were first included in the multivariate regression model and explained a small portion of the variance (R 2 = 9%). The subsequent model selection procedure for dimensions of health resulted in a model with the dimensions walking performance/mobility, disability in daily life, and health status/disease severity. These dimensions, in addition to demographics, jointly explained 24% of the variance in LAPAQ scores (Table 3). Adding more dimensions into the model did not increase the explained variance. This final model was not unique: Table 3 shows that various other models yielded only slightly lower R 2.
Discussion
Patients with PD are widely presumed to follow a sedentary lifestyle, due to their physical, cognitive, and emotional impairments. We now provide new evidence to underpin this assumption, based on analyses of time spent on daily physical activity in a large cohort of PD patients and another large cohort of controls. The loss of time spent on activities was most obvious in patients with greater disease severity.
Our results showed that PD patients were 29% less active compared to controls. In a previous study of 24,000 subjects aged 65 years and older, similarly reduced activity levels (by about 23%) were found for patients with a chronic disease such as musculoskeletal disorders and vascular or heart diseases [2]. The 29% reduction observed for PD patients in the present study might even be greater in comparison with healthy controls since our cohort did not include severely affected PD patients [24]. Moreover, the LASA study, which we used as a control group, showed that about 60% of the population had a chronic disease [39]. Direct comparison for comorbidity between the two groups was not possible as the LASA study only recorded broad categories and did not subdivide in specific disorders. Although it would be interesting incorporating fall histories in the analysis, data of fall history was not available for the control group. Future studies are required to investigate the influence of these factors.
It is important to consider the methods used to assess physical activity in the present and other studies. We used a validated interview-based physical activity questionnaire [33], which is a subjective method of measuring physical activity. This might have resulted in an overestimation of the reported physical activity. However, this possible overestimation likely applies equally to both patients and controls, so it is unlikely that this influenced our results. Another possibility is that patients underestimated their activity due to memory problems. However, patients with severe cognitive impairment (MMSE < 24) were excluded, so this is unlikely to explain the physical inactivity observed in PD patients. Other studies circumvented such problems by using objective measures of physical activity; these studies did not find differences between patients and controls [7, 11, 37]. Although these activity monitors have been well validated and shown to be reliable for a range of activities, some specific activities such as gardening and cycling are difficult to quantify [9, 20, 41]. This may be one reason for the discrepancy with our results.
We also investigated the determinants associated with daily physical activity in PD patients. One factor was gender. Univariate regression analysis showed that women with PD were 80% more active than men. This is in contrast with observations in non-PD populations [16]. The LAPAQ assessed a broad range of activities, including walking outside, cycling, gardening, light and heavy household activities, and a maximum of two sport activities. When we removed the household activities from the total activity score, men appeared to be more physically active than women (p < 0.01). The same effect was found in the control group. This suggests that women spent more time to daily activities because the LAPAQ records household activities. Another study found comparable results for older women: two-thirds of them reached recommended levels of physical activity when domestic activities were included in the assessment, but only 21% when these domestic activities were excluded [19].
We also found several additional determinants associated with daily physical activity. Specifically, inactivity in PD was associated with worse walking performance, more disability in daily life, and greater disease severity. These factors identified in this study for PD are comparable to other studies that investigated the determinants of physical inactivity in older persons [2, 6, 32].
Our results concerning the determinants of daily physical activity in PD have to be interpreted with some caution for several reasons. First, the final model was not unique, because various different combinations of determinants yielded almost the same percentage of explained variance. A model with two dimensions (i.e., walking performance and disability in daily life) was as good as a model with three dimensions (additionally including either disease severity, fear of falling, anxiety and depression, or faller status).
Second, in all models, the unexplained variance remained large. Our final model explained 24% of the variance. Adding more variables into the model did not increase the explained variance. This suggests that additional factors are responsible for the variability in LAPAQ scores in PD. Because we secondarily analyzed data from two previous trials, various factors were not investigated. One such factor is fatigue, which may be an independent contributor to physical inactivity in PD [11]. Moreover, social cognitive theories propose that behavioral factors are associated with physical activity [28, 32]. Earlier work showed that a model which included self-efficacy and outcome expectations, explained 64% of the variance in exercise behavior in older adults [28]. Other studies found that (lack of) interest in physical activity, knowledge about the benefits of exercise, and social supports also predicted exercise behavior [8, 28, 32]. In the literature, many other possible determinants have been suggested, ranging from income and socioeconomic status up to seasonal effects [30, 31, 36]. Further work, therefore, remains necessary to identify ‘all’ determinants, as a basis for future therapeutic interventions.
Although we showed that physical inactivity was most obvious in patients with greater disease severity, not all PD patients with advanced disease were completely sedentary. This suggests that even PD patients in later stages of the disease might be stimulated to become more active. Participating in regular physical activity would be particularly useful for PD patients, because exercise may help to prevent cardiovascular events, diabetes mellitus, and osteoporosis [40]. Moreover, in older subjects, physical activity was reported to suppress typical PD symptoms such as depression and cognitive decline [4, 18]. In addition, preclinical evidence in animals with experimental parkinsonism suggests that exercise may directly alter the neurodegenerative process in PD [27]. A meta-analysis found exercise to be effective at improving physical functioning, health-related quality of life, strength, balance, and gait speed for people with PD [15]. It is, therefore, important for PD patients to avoid a sedentary lifestyle. Simply informing people about the health benefits of physical activity is likely insufficient to attain a sustained behavioral change. Motivational aspects are especially important because such behavioral interventions could target motivation to increase levels of physical activity. We are now testing this in the ParkFit trial, a large exercise study involving 586 PD patients randomized to receive a behavioral change program aimed to increase daily physical activity levels. The ParkFit trial uses motivational strategies and personal health coaches to induce a lasting increase in exercise behavior for patients with PD; the first results are expected in 2012 [38].
References
Ainsworth BE, Haskell WL, Leon AS, Jacobs DR Jr, Montoye HJ, Sallis JF, Paffenbarger RS Jr (1993) Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc 25:71–80
Ashe MC, Miller WC, Eng JJ, Noreau L (2009) Older adults, chronic disease and leisure-time physical activity. Gerontology 55:64–72
Biemans MA, Dekker J, van der Woude LH (2001) The internal consistency and validity of the Self-Assessment Parkinson’s Disease Disability Scale. Clin Rehabil 15:221–228
Blumenthal JA, Babyak MA, Moore KA, Craighead WE, Herman S, Khatri P, Waugh R, Napolitano MA, Forman LM, Appelbaum M, Doraiswamy PM, Krishnan KR (1999) Effects of exercise training on older patients with major depression. Arch Intern Med 159:2349–2356
Busse ME, Pearson OR, Van DR, Wiles CM (2004) Quantified measurement of activity provides insight into motor function and recovery in neurological disease. J Neurol Neurosurg Psychiatry 75:884–888
Chad KE, Reeder BA, Harrison EL, Ashworth NL, Sheppard SM, Schultz SL, Bruner BG, Fisher KL, Lawson JA (2005) Profile of physical activity levels in community-dwelling older adults. Med Sci Sports Exerc 37:1774–1784
Chastin SF, Baker K, Jones D, Burn D, Granat MH, Rochester L (2010) The pattern of habitual sedentary behavior is different in advanced Parkinson’s disease. Mov Disord 25:2114–2120
Crombie IK, Irvine L, Williams B, McGinnis AR, Slane PW, Alder EM, McMurdo ME (2004) Why older people do not participate in leisure time physical activity: a survey of activity levels, beliefs and deterrents. Age Ageing 33:287–292
Dahlgren G, Carlsson D, Moorhead A, Hager-Ross C, McDonough SM (2010) Test-retest reliability of step counts with the ActivPAL device in common daily activities. Gait Posture 32:386–390
Deeg DJ, van TT, Smit JH, de Leeuw ED (2002) Attrition in the Longitudinal Aging Study Amsterdam. The effect of differential inclusion in side studies. J Clin Epidemiol 55:319–328
Elbers R, van Wegen EE, Rochester L, Hetherington V, Nieuwboer A, Willems AM, Jones D, Kwakkel G (2009) Is impact of fatigue an independent factor associated with physical activity in patients with idiopathic Parkinson’s disease? Mov Disord 24:1512–1518
Fertl E, Doppelbauer A, Auff E (1993) Physical activity and sports in patients suffering from Parkinson’s disease in comparison with healthy seniors. J Neural Transm Park Dis Dement Sect 5:157–161
Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkinson disease. Arch Neurol 56:33–39
Giladi N, Shabtai H, Simon ES, Biran S, Tal J, Korczyn AD (2000) Construction of freezing of gait questionnaire for patients with Parkinsonism. Parkinsonism Relat Disord 6:165–170
Goodwin VA, Richards SH, Taylor RS, Taylor AH, Campbell JL (2008) The effectiveness of exercise interventions for people with Parkinson’s disease: a systematic review and meta-analysis. Mov Disord 23:631–640
Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A (2007) Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 116:1081–1093
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17:427–442
Lautenschlager NT, Cox KL, Flicker L, Foster JK, van Bockxmeer FM, Xiao J, Greenop KR, Almeida OP (2008) Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease: a randomized trial. JAMA 300:1027–1037
Lawlor DA, Taylor M, Bedford C, Ebrahim S (2002) Is housework good for health? Levels of physical activity and factors associated with activity in elderly women. Results from the British Women’s Heart and Health Study. J Epidemiol Community Health 56:473–478
Masse LC, Fuemmeler BF, Anderson CB, Matthews CE, Trost SG, Catellier DJ, Treuth M (2005) Accelerometer data reduction: a comparison of four reduction algorithms on select outcome variables. Med Sci Sports Exerc 37:S544–S554
Mondolo F, Jahanshahi M, Grana A, Biasutti E, Cacciatori E, Di BP (2006) The validity of the hospital anxiety and depression scale and the geriatric depression scale in Parkinson’s disease. Behav Neurol 17:109–115
Morris S, Morris ME, Iansek R (2001) Reliability of measurements obtained with the Timed “Up & Go” test in people with Parkinson disease. Phys Ther 81:810–818
Movement Disorder Society Task Force on Rating Scales for Parkinson’s Disease (2003) The Unified Parkinson’s Disease Rating Scale (UPDRS): status and recommendations. Mov Disord 18:738–750
Munneke M, Nijkrake MJ, Keus SH, Kwakkel G, Berendse HW, Roos RA, Borm GF, Adang EM, Overeem S, Bloem BR (2010) Efficacy of community-based physiotherapy networks for patients with Parkinson’s disease: a cluster-randomised trial. Lancet Neurol 9:46–54
Nijkrake MJ, Keus SH, Overeem S, Oostendorp RA, Vlieland TP, Mulleners W, Hoogerwaard EM, Bloem BR, Munneke M (2010) The ParkinsonNet concept: development, implementation and initial experience. Mov Disord 25:823–829
Parmelee PA, Thuras PD, Katz IR, Lawton MP (1995) Validation of the Cumulative Illness Rating Scale in a geriatric residential population. J Am Geriatr Soc 43:130–137
Petzinger GM, Walsh JP, Akopian G, Hogg E, Abernathy A, Arevalo P, Turnquist P, Vuckovic M, Fisher BE, Togasaki DM, Jakowec MW (2007) Effects of treadmill exercise on dopaminergic transmission in the 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine-lesioned mouse model of basal ganglia injury. J Neurosci 27:5291–5300
Resnick B, Nigg C (2003) Testing a theoretical model of exercise behavior for older adults. Nurs Res 52:80–88
Rochester L, Jones D, Hetherington V, Nieuwboer A, Willems AM, Kwakkel G, van WE (2006) Gait and gait-related activities and fatigue in Parkinson’s disease: what is the relationship? Disabil Rehabil 28:1365–1371
Roshanaei-Moghaddam B, Katon WJ, Russo J (2009) The longitudinal effects of depression on physical activity. Gen Hosp Psychiatry 31:306–315
Shephard RJ, Aoyagi Y (2009) Seasonal variations in physical activity and implications for human health. Eur J Appl Physiol 107:251–271
Shimada H, Lord SR, Yoshida H, Kim H, Suzuki T (2007) Predictors of cessation of regular leisure-time physical activity in community-dwelling elderly people. Gerontology 53:293–297
Stel VS, Smit JH, Pluijm SM, Visser M, Deeg DJ, Lips P (2004) Comparison of the LASA Physical Activity Questionnaire with a 7-day diary and pedometer. J Clin Epidemiol 57:252–258
Tinetti ME, Richman D, Powell L (1990) Falls efficacy as a measure of fear of falling. J Gerontol 45:239–243
Toth MJ, Fishman PS, Poehlman ET (1997) Free-living daily energy expenditure in patients with Parkinson’s disease. Neurology 48:88–91
Trost SG, Owen N, Bauman AE, Sallis JF, Brown W (2002) Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc 34:1996–2001
van Hilten JJ, Hoogland G, van der Velde EA, Middelkoop HA, Kerkhof GA, Roos RA (1993) Diurnal effects of motor activity and fatigue in Parkinson’s disease. J Neurol Neurosurg Psychiatry 56:874–877
van Nimwegen M, Speelman AD, Smulders K, Overeem S, Borm GF, Backx FJ, Bloem BR, Munneke M (2010) Design and baseline characteristics of the ParkFit study, a randomized controlled trial evaluating the effectiveness of a multifaceted behavioral program to increase physical activity in Parkinson patients. BMC Neurol 10:70
Visser M, Pluijm SM, Stel VS, Bosscher RJ, Deeg DJ (2002) Physical activity as a determinant of change in mobility performance: the Longitudinal Aging Study Amsterdam. J Am Geriatr Soc 50:1774–1781
Warburton DE, Nicol CW, Bredin SS (2006) Health benefits of physical activity: the evidence. CMAJ 174:801–809
Welk GJ (2002) Physical activity assessments for health-related research. Human Kinetics Publishers Inc, Canada
Acknowledgments
The ParkinsonNet trial was supported by ZonMw (947-04-357), the Netherlands Organization for Scientific Research, the Dutch Parkinson’s Disease Society, the National Parkinson Foundation, and De Stichting Robuust. The Longitudinal Aging Study Amsterdam is largely supported by a grant from the Netherlands Ministry of Health Welfare and Sports, Directorate of Nursing Care and Older persons. This study was sponsored by the MJ Fox Foundation and the National Parkinson Foundation. All sources of funding had no further involvement.
Conflict of interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
van Nimwegen, M., Speelman, A.D., Hofman-van Rossum, E.J.M. et al. Physical inactivity in Parkinson’s disease. J Neurol 258, 2214–2221 (2011). https://doi.org/10.1007/s00415-011-6097-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6097-7