Abstract
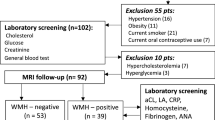
The right-to-left shunts (RLS) and white matter lesions (WMLs) are frequently observed in migraineurs and in patients with ischemic stroke. Previous studies have reported that the burden of WMLs did not increase with the intracardiac right-to-left shunt (RLS) in migraineurs. However, some types of WMLs are known to be associated with RLS in patients with stroke and dementia. The aim of the study was to demonstrate the difference in the size and location of WMLs, according to the existence of RLS in patients with headache. From the prospective headache registry, a total of 425 subjects (age, 30.8 ± 5.1 years; 303 women; 242 migraineurs; 183 patients with tension-type headache (TTH)) were retrospectively reviewed and evaluated for RLS and WMLs using M-mode power transcranial Doppler sonography (mTCD) and brain magnetic resonance imaging scans. We scored WMLs, according to the Rotterdam Scan Study, and assessed the association between RLS presence and the location and size of WMLs. The number of small deep WMLs (dWMLs) and the prevalence of RLS, defined as microembolic signals (MES) ≥11, were higher in patients with migraine (small dWMLs, 6.23 vs. 4.05; RLS, 36.8% vs. 10.9%), compared to patients with TTH. There was no significant difference in the sum of periventricular WML grades or the total volume of dWMLs between TTH and migraine patients. Among the migraineurs, the patients with RLS more frequently had small dWMLs, aura, and heart disease compared to those without RLS. In addition, RLS were also independent predictors for the presence of small dWMLs from the multivariate binary regression analysis (p < 0.01; OR = 3.24; 95%CI 1.56–6.72). Small dWMLs are associated with RLS in young migraineurs. These results imply that paradoxical embolism may cause the small WMLs in some migraineurs.


Similar content being viewed by others
Abbreviations
- dWMLs:
-
Deep white matter lesions
- MESs:
-
Microembolic signals
- mTCD:
-
m-mode power transcranial Doppler sonography
- RLS:
-
Right-to-left shunts
- pvWMLs:
-
Periventricular white matter lesions
- TTH:
-
Tension-type headache
- WMLs:
-
White matter lesions
References
(1994) Practice parameter: the utility of neuroimaging in the evaluation of headache in patients with normal neurologic examinations (summary statement). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 44:1353–1354
Adami A, Rossato G, Cerini R, Thijs VN, Pozzi-Mucelli R, Anzola GP, Del Sette M, Finocchi C, Meneghetti G, Zanferrari C (2008) Right-to-left shunt does not increase white matter lesion load in migraine with aura patients. Neurology 71:101–107
Anzola GP, Magoni M, Guindani M, Rozzini L, Dalla Volta G (1999) Potential source of cerebral embolism in migraine with aura: a transcranial Doppler study. Neurology 52:1622–1625
Anzola GP, Meneghetti G, Zanferrari C, Adami A, Dinia L, Del Sette M (2008) Is migraine associated with right-to-left shunt a separate disease? Results of the SAM study. Cephalalgia 28:360–366
Bokura H, Kobayashi S, Yamaguchi S (1998) Distinguishing silent lacunar infarction from enlarged Virchow-Robin spaces: a magnetic resonance imaging and pathological study. J Neurol 245:116–122
Bousser MG (2004) Estrogens, migraine, and stroke. Stroke 35:2652–2656
Breteler MM, van Swieten JC, Bots ML, Grobbee DE, Claus JJ, van den Hout JH, van Harskamp F, Tanghe HL, de Jong PT, van Gijn J et al (1994) Cerebral white matter lesions, vascular risk factors, and cognitive function in a population-based study: the Rotterdam Study. Neurology 44:1246–1252
Dalla Volta G, Guindani M, Zavarise P, Griffini S, Pezzini A, Padovani A (2005) Prevalence of patent foramen ovale in a large series of patients with migraine with aura, migraine without aura and cluster headache, and relationship with clinical phenotype. J Headache Pain 6:328–330
Del Sette M, Dinia L, Bonzano L, Roccatagliata L, Finocchi C, Parodi RC, Sivori G, Gandolfo C (2008) White matter lesions in migraine and right-to-left shunt: a conventional and diffusion MRI study. Cephalalgia 28:376–382
Djaiani G, Phillips-Bute B, Podgoreanu M, Messier RH, Mathew JP, Clements F, Newman MF (2004) The association of patent foramen ovale and atrial fibrillation after coronary artery bypass graft surgery. Anesth Analg 98:585–589 (table of contents)
Dowson A, Mullen MJ, Peatfield R, Muir K, Khan AA, Wells C, Lipscombe SL, Rees T, De Giovanni JV, Morrison WL, Hildick-Smith D, Elrington G, Hillis WS, Malik IS, Rickards A (2008) Migraine intervention With STARFlex technology (MIST) trial: a prospective, multicenter, double-blind, sham-controlled trial to evaluate the effectiveness of patent foramen ovale closure with STARFlex septal repair implant to resolve refractory migraine headache. Circulation 117:1397–1404
Ferrarini G, Malferrari G, Zucco R, Gaddi O, Norina M, Pini LA (2005) High prevalence of patent foramen ovale in migraine with aura. J Headache Pain 6:71–76
Garg P, Servoss SJ, Wu JC, Bajwa ZH, Selim MH, Dineen A, Kuntz RE, Cook EF, Mauri L (2010) Lack of association between migraine headache and patent foramen ovale: results of a case-control study. Circulation 121:1406–1412
Handke M, Harloff A, Olschewski M, Hetzel A, Geibel A (2007) Patent foramen ovale and cryptogenic stroke in older patients. N Engl J Med 357:2262–2268
Hara H, Virmani R, Ladich E, Mackey-Bojack S, Titus J, Reisman M, Gray W, Nakamura M, Mooney M, Poulose A, Schwartz RS (2005) Patent foramen ovale: current pathology, pathophysiology, and clinical status. J Am Coll Cardiol 46:1768–1776
Kruit MC, van Buchem MA, Hofman PA, Bakkers JT, Terwindt GM, Ferrari MD, Launer LJ (2004) Migraine as a risk factor for subclinical brain lesions. JAMA 291:427–434
Kwon SU, Cho YJ, Koo JS, Bae HJ, Lee YS, Hong KS, Lee JH, Kim JS (2005) Cilostazol prevents the progression of the symptomatic intracranial arterial stenosis: the multicenter double-blind placebo-controlled trial of cilostazol in symptomatic intracranial arterial stenosis. Stroke 36:782–786
Lee SH, Bae HJ, Kwon SJ, Kim H, Kim YH, Yoon BW, Roh JK (2004) Cerebral microbleeds are regionally associated with intracerebral hemorrhage. Neurology 62:72–76
Lee ST, Chu K, Jung KH, Kim DH, Kim EH, Choe VN, Kim JH, Im WS, Kang L, Park JE, Park HJ, Park HK, Song EC, Lee SK, Kim M, Roh JK (2008) Decreased number and function of endothelial progenitor cells in patients with migraine. Neurology 70:1510–1517
Liu JR, Plotz BM, Rohr A, Stingele R, Jansen O, Alfke K (2009) Association of right-to-left shunt with frontal white matter lesions in T2-weighted MR imaging of stroke patients. Neuroradiology 51:299–304
Loevner LA, Shapiro RM, Grossman RI, Overhauser J, Kamholz J (1996) White matter changes associated with deletions of the long arm of chromosome 18 (18q- syndrome): a dysmyelinating disorder? AJNR Am J Neuroradiol 17:1843–1848
Moschiano F, D’Amico D, Di Stefano M, Rocca N, Bussone G (2007) The role of the clinician in interpreting conventional neuroimaging findings in migraine patients. Neurol Sci 28(Suppl 2):S114–S117
Mullen MJ, Hildick-Smith D, De Giovanni JV, Duke C, Hillis WS, Morrison WL, Jux C (2006) BioSTAR Evaluation STudy (BEST): a prospective, multicenter, phase I clinical trial to evaluate the feasibility, efficacy, and safety of the BioSTAR bioabsorbable septal repair implant for the closure of atrial-level shunts. Circulation 114:1962–1967
Purandare N, Oude Voshaar RC, McCollum C, Jackson A, Burns A (2008) Paradoxical embolisation and cerebral white matter lesions in dementia. Br J Radiol 81:30–34
Schwerzmann M, Wiher S, Nedeltchev K, Mattle HP, Wahl A, Seiler C, Meier B, Windecker S (2004) Percutaneous closure of patent foramen ovale reduces the frequency of migraine attacks. Neurology 62:1399–1401
HCCoTIH Society (2004) The international classification of headache disorders (second edition). Cephalalgia 24(Suppl 1):1–160
Vermeer SE, Hollander M, van Dijk EJ, Hofman A, Koudstaal PJ, Breteler MM (2003) Silent brain infarcts and white matter lesions increase stroke risk in the general population: the Rotterdam scan study. Stroke 34:1126–1129
Vernooij MW, van der Lugt A, Ikram MA, Wielopolski PA, Niessen WJ, Hofman A, Krestin GP, Breteler MM (2008) Prevalence and risk factors of cerebral microbleeds: the Rotterdam scan study. Neurology 70:1208–1214
Wilmshurst PT, Nightingale S, Walsh KP, Morrison WL (2000) Effect on migraine of closure of cardiac right-to-left shunts to prevent recurrence of decompression illness or stroke or for haemodynamic reasons. Lancet 356:1648–1651
Woods TD, Harmann L, Purath T, Ramamurthy S, Subramanian S, Jackson S, Tarima S (2010) Small- and moderate-size right-to-left shunts identified by saline contrast echocardiography are normal and unrelated to migraine headache. Chest 138:264–269
Acknowledgments
This study was supported by the Ministry of Health and Welfare (grant No. A090440), Republic of Korea.
Conflict of interest
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, HK., Lee, SY., Kim, SE. et al. Small deep white matter lesions are associated with right-to-left shunts in migraineurs. J Neurol 258, 427–433 (2011). https://doi.org/10.1007/s00415-010-5771-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-010-5771-5