Abstract
Background
Axonal degeneration is considered to play a major role in the development of clinical disability in multiple sclerosis (MS). N-AcetylAspartic Acid (NAA) is a neuron-specific marker constantly identified in MR-spectroscopy studies of the normal and MS brain. To our knowledge there are no studies available that evaluated NAA in cerebrospinal fluid (CSF) as a possible marker for disease severity.
Objective
To evaluate CSF concentrations of NAA in MS in relation to disease phenotype, clinical measures of disability and MRI markers of disease burden.
Methods
NAA concentrations were determined in CSF of 46 patients with MS (26 relapsing remitting (RRMS), 12 secondary progressive (SPMS) and 8 primary progressive (PPMS)). Prior to lumbar puncture, MS-patients underwent MRI and clinical examination, including the Expanded Disability Status Scale (EDSS) and the MS Functional Composite (MSFC). Additionally, CSF concentrations of NAA were determined in 12 patients with other neurological diseases (OND).
Results
Median CSF NAA concentration was 0.74 (IQR: 0.59-.94) in RRMS , 0.54 (IQR: 0.35-.73) in SPMS and 0.83 μmol/l (IQR: 0.56-.03) in PPMS patients. SPMS patients had a significantly lower NAA concentration than RRMS patients. NAA concentrations correlated with EDSS (r = )0.37, p = 0.016), MSFC (r = 0.41, p = 0.010), normalised brain volume (r = 0.49, p = 0.001), T2 lesion load (r = )0.35, p = 0.021) and black hole lesion load (r = )0.47, p = 0.002). No differences were observed between OND (median: 0.57 IQR: 0.28-.73) and MS patients.
Conclusion
CSF NAA concentration in MS patients is related to clinical performance and MRI measures of disease burden and may therefore be an important neuron specific marker of disease severity and possibly progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Axonal damage and axonal loss are important features of the pathology of multiple sclerosis (MS), occurring early in the disease course and associated with active inflammatory lesions [2, 13, 17, 26]. Axonal degeneration is not restricted to lesions but is also present in the normal appearing white matter (NAWM), probably due to Wallerian degeneration [12]. The current view is that axonal degeneration plays a major role in the development of persisting disability in MS [27].
A proposed in vivo marker for axonal pathology in MS is N-AcetylAspartic Acid (NAA). NAA is an amino acid synthesized and almost exclusively localised in neurons [3]. Evidence from various studies suggests that NAA is turned over more than once each day by an intercompartimental metabolic cycle between neurons, extracellular fluid and oligodendrocytes [1]. Post-mortem investigation of spinal cords from MS patients has shown that lower tissue concentrations of NAA are related to lower axonal volume. Furthermore, the average NAA concentration per axonal volume may decrease with increasing demyelination and functional impairment of neurons [4]. MR-spectroscopy (MRS) is widely used to determine parenchymal NAA concentrations in vivo. Several MRSstudies have shown a decrease of NAA in MS lesions [7]. Other studies have shown that NAA decrease in lesions and NAWM is related to clinical disability and progressive brain atrophy [10, 9, 11] Some, but not all, studies have shown a decrease of NAA in the NAWM [8, 14, 28, 29]. These findings indicate that NAA is a neuron-specific marker that reflects MSpathology related to clinical functioning. NAA may therefore be a useful biomarker for disease progression in MS.
Methods for measuring NAA in body fluids have been developed for the diagnosis of Canavans’ disease [15]. To our knowledge, there are no studies on NAA-concentrations in cerebrospinal fluid (CSF) of MS patients [24]. The aim of this exploratory study was to evaluate CSF concentrations of NAA in MSpatients in relation to disease phenotype, clinical measures of disability and MRI markers of disease burden.
Materials and methods
Study population
This study is part of an ongoing research project on CSF in MS. Patients were recruited either in response to an appeal in the periodical of the Dutch MS society, or from patients visiting or admitted at our clinic. Patients were requested to voluntarily undergo a lumbar puncture, MRI and clinical testing. All participants gave written informed consent and the local ethics committee approved the study.
CSF samples were collected from a group of 46 MS patients diagnosed according to the Poser criteria [22]. Patients were classified as having a relapsing remitting (RRMS, n = 26), secondary progressive (SPMS, n = 12) or primary progressive (PPMS, n = 8) disease course according to Lublin and Reingold [19]. Prior to lumbar puncture patients underwent clinical examination, including the Expanded Disability Status Scale (EDSS) and the Multiple Sclerosis Functional Composite (MSFC) [6, 18].
The EDSS was performed by trained medical doctors, as were the individual components of the MSFC (25-foot Timed Walk Test (TWT), Nine-Hole Peg Test (9-HPT) and the 3 second Paced Auditory Serial Addition Test (PASAT3)). 43 patients underwent EDSS-examination and 39 patients underwent MSFC-examination. The overall MSFC-score was calculated using a previously published reference population of MS-patients [16]. MRI examination was performed within 23 days of lumbar puncture.
Additionally, CSF was collected from 12 patients presenting with neurological signs and symptoms that warranted a diagnostic lumbar puncture. These patients will from now on be referred to as ‘Other Neurological Diseases’ (OND). In 10 of the OND patients, neurological disease was confirmed or remained suspect on further diagnostic testing.
CSF-analysis
After collection, CSF samples were centrifuged, aliquoted, coded and stored at −80°C. All CSF-samples were analysed in a single session.
NAA was measured using a modified stable isotope dilution Gas Chromatography-Mass Spectrometry (GC-MS) method [15]. In short, 1 nmol [D3]-NAA was added as internal standard to 100 µl of CSF. This was also added to an aqueous standard, to obtain a calibration curve in the range from 0.1 to 2.0 nmol. The samples were acidified with 30 µl HCL (6 mol/l) to pH < 2 and saturated with NaCl. Thereafter the sample was extracted four times with 2 ml of an ethylacetate-2-propanol mixture (v/v 10:1). The collected organic fractions were dried by anhydrous Na2SO4 and subsequently evaporated to dryness at 40°C under a gentle stream of N2. NAA was converted to its di-isopropyl derivative by adding 500 µl isopropanol and 10 µl 6 mol/l HCl and subsequent heating for 1 hour at 120°C. An aliquot of 1 µl of this mixture was analysed by GC-MS. GC-MS analysis of 1 µl of this mixture was performed on an Automass II (ThermoFinnigan) system. The gas chromatographic separation was achieved on a CPSil-88 capillary fused silica column (25 m × 0.25 mm, df = 0.28 µm (Chrompack Int., Middelburg, The Netherlands)), which was directly inserted into the source of the spectrometer. Helium was used as carrier gas with a linear flow of 20 cm/s. The oven temperature was kept at 80°C for 1 min and then raised to 240°C at a rate of 30°C/min. The interface and source temperatures were kept at 240°C. Mass fragmentography was achieved with positive chemical ionisation with ammonia as reagent gas at optimised source pressure. The ions m/z 260 (base peak protonated pseudomolecular ion (M + 1) for NAA-di-isopropyl) and m/z 263 (internal standard [D3]-NAA-di-isopropyl) were monitored. The inter-assay variation for this method was 8% (n = 5) and the intra-assay variation was 2% (n = 10). All samples were analysed within the linear range of the standard curve (0–20 nmol/L).
The concentration of Growth-associated protein 43 (GAP43) was measured in 44 of the 46 CSF samples from MS patients. The results and measurement methods of GAP-43 are described elsewhere [25].
MRI acquisition and analysis
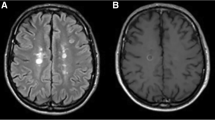
MRI-acquisition was performed at 1.0 Tesla (Siemens, Erlangen, Germany) and consisted of axial pre- and post-contrast T1-weighted (repetition time [TR] = 700 ms, echo time [TE] = 15 ms, 5.5 mm slice thickness) images and T2-weighted ([TR] = 2700 ms, [TE] = 90 ms, 5.5 mm slice thickness) images. MRI was performed within 23 days of CSF collection. Two patients refused to undergo MRI.
T1 hypo intense or black hole lesion load (BHLL), T2 lesion load (T2LL) and gadolinium enhancing lesion load (GADLL) were quantified using home-developed semi-automated seed growing software based on a local thresholding technique presence of sadolinium enhancing lesions was noted.
Normalised brain volume (NBV) was measured on T1-weighted pre-contrast images using Structural Image Evaluation, using Normalisation of Atrophy Cross-sectionally (SIENAX) [23]. A detailed description of SIENAX can be found in the original presenting paper [23]. Two patients were excluded from brain volume analysis, because pre-contrast MRI seans were not available. SIENAX is freely available as part of the FMRIB Software Library (www.fmrib.ox.ac.uk/fsl).
Statistical analysis
All values are given as medians with interquartile range (IQR). Normality of the distribution of all variables was checked. When normality was rejected, non-parametric statistics were used. Group comparisons for patient characteristics and study variables were performed between MS-subtypes, all MS patients and OND, MS subtypes and OND, patients on disease modifying therapy or not and patients with or without contrast enhancing lesions. Generally, p-values smaller than 0.05 were considered statistically significant. Comparisons between two groups were performed using the Mann-Whitney U test or the independent samples t-test, as appropriate. Comparisons between more than 2 groups were performed using the Kruskal-Wallis test. When this test was significant, subsequent pairwise comparisons were done using Mann-Whitney U tests. Correction for multiple comparisons in these post-hoc tests was accomplished by setting the cut-off p-value for statistical significance at 0.05 divided by the number of comparisons. Correlation analysis was performed using either Pearson or Spearman correlations, as appropriate.
Correlations of NAA concentrations in CSF with clinical (EDSS, MSFC), radiological measures (NBV, T2LL, BHLL) and GAP43 concentrations in CSF were performed in the total group of MS-patients and subgroups defined by disease onset. Thus, the relapse onset subgroup consisted of RRMS- and SPMS-patients, and the progressive onset subgroup of PPMS-patients. All statistical analyses were performed using SPSS (version 11.0) statistical software.
Results
Patient characteristics
Differences in patient characteristics (Table 1) between subtypes of MS were as expected. For RRMS and SPMS patients, median time between start date of last relapse and CSF-collection was 13.5 months (IQR: 3.8–41 months), with a minimum of 11 days. Patients did not receive intravenous methylprednisolone for at least 3 months prior to CSF collection. 14 MS patients were on disease modifying therapy at the time of CSFcollection.
NAA concentrations in MS patients
The median CSF concentrations of NAA in MS patients are given in Figure 1.
Concentrations of NAA in MS-subtypes and other neurological diseases (OND). Boxes represent values from the 25th to the 75th percentiles, inner lines represent the median and whiskers show the minimum value. SP patients had a significantly lower NAA than RRMS patients (p = 0.015), as indicated by an asterisk(*)
Between MS subtypes, a significant difference in NAA concentration was observed (p = 0.043). Further analysis revealed that NAA concentration was lower in SPMS patients compared with RRMS patients (p = 0.015). In the total group of MS patients, NAA concentration did not correlate with disease duration (r = )0.18, p = 0.220) or age (r = )0.38, p = 0.801) and did not differ between patients with or without disease modifying therapy (p = 0.779).
NAA concentrations in MS patients compared with OND
NAA concentration did not differ between the OND and the total group of MS patients (p = 0.077), nor between OND and any of the MS subtypes (RRMS, p = 0.033; SPMS, p = 0.932; PPMS, p = 0.082).
Lower NAA concentration in CSF is related to worse clinical functioning
In the total MS group, NAA concentrations correlated negatively with EDSS (r = −0.37, p = 0.016) (Figure 2) and positively with MSFC (r = 0.41, p = 0.010), indicating that worse clinical functioning is associated with lower NAA. The correlation of NAA with EDSS and MSFC increased when relapse onset patients were considered separately (r = −0.49, p = 0.003 and r = 0.50, p = 0.004).
Lower NAA concentration in CSF is related to lower brain volume
NBVs are presented in Table 2. A significant difference in NBV between MS-subtypes (p = 0.006) was observed. SPMS patients had a significantly lower NBV compared with RRMS patients (p = 0.001). In the total MS-group, NAA concentration and NBV correlated positively (r = 0.49, p = 0.001), indicating that lower NAA was associated with lower brain volume (Figure 3). In relapse onset patients, the correlation between NAA and NBV was comparable (r = 0.50, p = 0.002) with the total MS-group.
Lower NAA concentration in CSF is related to higher lesion load
Lesion loads are presented in Table 2. A significant difference in BHLL was observed between subtypes of MS (p = 0.010). As expected, SPMS patients had a higher BHLL than RRMS (p = 0.005) and tended to be higher than PPMS patients (p = 0.016).
In the total MS group, the CSF concentrations of NAA correlated negatively with T2LL (r = −0.35, p = 0.021), indicating that higher T2LL is associated with lower NAA in CSF. In relapse onset patients, correlation between CSF-concentrations of NAA and T2LL (r = −0.34, p = 0.046) was similar.
BHLL correlated with CSF concentrations of NAA in the total group (r = −0.47, p = 0.002). This was also observed in relapse onset patients, though of lower magnitude (r = −0.38, p = 0.026).
10 out of 42 patients had gadolinium enhancing lesions on MRI examination. No significant differences in CSF concentrations of NAA were observed between patients with or without enhancing lesions (p = 0.248). GADLL did not correlate with CSF concentrations of NAA (r = −0.16, p = 0.322).
CSF concentrations of NAA and GAP43 are related
A positive correlation was observed between concentrations of NAA and GAP43 in the total MS group (r = 0.44, p = 0.003), which increased when relapse onset patients were considered separately (r = 0.581, p < 0.001).
Discussion
The major findings in this exploratory study are that, in MS patients, lower NAA concentrations in CSF are related to a later stage of relapse onset MS, more clinical disability, higher lesion load and lower brain volume.
Our findings on CSF NAA are in line with previous MRS studies that showed a relationship between lower parenchymal NAA and more clinical disability as well as lower brain volume [9–11, 20]. We also found that NAA in CSF is lower in patients with higher lesion load, which is in line with the lower NAA concentration in MS lesions measured by MRS [7]. These similarities suggest that NAA in CSF reflects a similar pathological process as is responsible for parenchymal NAA concentrations measured by MRS.
Previous studies have shown that NAA is primarily located in neurons, and that lower parenchymal NAA concentration is related to reduced axonal volume in the spinal cord [1, 4]. Axonal damage has been associated with MS induced lesions [2, 13, 17, 26] T1 hypo intense or black hole lesions are generally considered to represent lesions with severe tissue destruction, including axonal degeneration [5, 26] Brain volume is thought to partly reflect the extent of axonal degeneration in ms although demyelination, oedema and glial cell proliferation may influence brain volume measurements [20]. In view of this, our finding that reduced NAA is related to lower brain volume and higher T2, and especially black hole, lesion volume indicates that NAA in CSF probably reflects axonal degeneration.
Relatively few studies have found a correlation of biomarkers for axonal damage with clinical disability [24]. In this study, CSF concentrations of NAA correlated with EDSS and MSFC, suggesting that NAA in CSF is a biological marker that may have clinical relevance. The strength of the relationship between NAA concentration in CSF and clinical measures may seem modest, there are however factors that may have reduced the magnitude of correlations between biological markers and clinical measures. Firstly, clinical measures have limitations as they incompletely cover the central nervous system and are prone to observerbias. Therefore, clinical measures may not detect all relevant changes in clinical functioning resulting from MS pathology in the central nervous system. Secondly, accumulating pathological changes of the central nervous system may not lead to clinical disability before reaching a critical threshold. Pathological changes that are reflected by NAA concentrations in CSF may therefore not be clinically apparent at the time of CSF withdrawal.
NAA concentrations in CSF were higher in RRMS patients compared with SPMS patients. The finding that disease duration did not correlate with NAA, whereas a difference was observed between RRMS and SPMS patients, is surprising. However, disease severity or stage is not interchangeable with disease duration, since time to conversion to SPMS and the time frame in which disease progression occurs varies. A mechanistic explanation for the difference between RRMS and SPMS, could be that NAA is released into the CSF, possibly as a result of acute axonal damage associated with inflammatory activity in especially RRMS. From this perspective, the lower concentration of NAA in SPMS compared with RRMS patients may reflect a relative decrease in overt inflammatory activity. However, we did not observe a relationship between NAA concentration and the occurrence of contrast enhancing lesions or with the use of disease modifying therapy. In view of the relationships between NAA, NBV and lesion load, the reduced NAA concentration in SPMS compared with RRMS patients could mean that the decrease of NAA in CSF reflects the accumulation of axonal degeneration in a later stage of MS.
For direct comparison with MS patients, we had CSF samples available from 12 patients who underwent a lumbar puncture for diagnostic purposes (OND). We did not observe a significant difference between OND and MS patients or OND and MS subtypes. This finding does not support or invalidates the hypothesis that decrease of NAA reflects axonal degeneration in MS. However, the OND group consisted of patients with a range of neurological signs, symptoms and diagnoses of which the effect on NAA concentration in CSF is not known.
GAP43 is a marker associated with growth cones, synaptic plasticity and synaptic regeneration [21]. Recently, we showed that concentrations of GAP43 can be determined in CSF and are related to brain volume measured on MRI [25]. The relationship we found between NAA and GAP43, suggest that both markers reflect a bond damage in the MS brain.
In conclusion, our findings suggest that NAA in CSF may be a novel neuron-specific marker for disease severity and possibly progression in MS. The results of this explorative study will have to be confirmed in a second, independent and larger patient group that should also be followed longitudinally.
References
Baslow MH (2003) N-acetylaspartate in the vertebrate brain: Metabolism and function. Neurochem Rese 28:941-53
Bitsch A, Schuchardt J, Bunkowski S, Kuhlmann T, Bruck W (2000) Acute axonal injury in multiple sclerosis - Correlation with demyelination and inflammation. Brain 123:1174-183
Bjartmar C, Battistuta J, Terada N, Dupree E, Trapp BD (2002) N-acetylaspartate is an axon-specific marker of mature white matter in vivo: a biochemical and immunohistochemical study on the rat optic nerve. Ann Neurol 51:51-8
Bjartmar C, Kidd G, Mork S, Rudick R, Trapp BD (2000) Neurological disability correlates with spinal cord axonal loss and reduced N-acetyl aspartate in chronic multiple sclerosis patients. Ann Neurol 48:893-01
Bruck W, Bitsch A, Kolenda H, Bruck Y, Stiefel M, Lassmann H (1997) Inflammatory central nervous system demyelination: correlation of magnetic resonance imaging findings with lesion pathology. Ann Neurol 42:783-93
Cutter GR, Baier ML, Rudick RA, Cookfair DL, Fischer JS, Petkau J, Syndulko K, Weinshenker BG, Antel JP, Confavreux C, Ellison GW, Lublin F, Miller AE, Rao SM, Reingold S, Thompson A, Willoughby E (1999) Development of a multiple sclerosis functional composite as a clinical trial outcome measure. Brain 122(Pt 5):871-82
Davie CA, Hawkins CP, Barker GJ, Brennan A, Tofts PS, Miller DH, Mcdonald WI (1994) Serial Proton Magnetic-Resonance Spectroscopy in Acute Multiple-Sclerosis Lesions. Brain 117:49-8
De Stefano N, Guidi L, Stromillo ML, Bartolozzi ML, Federico A (2003) Imaging neuronal and axonal degeneration in multiple sclerosis. Neurol Sci 24:S283–S286
De Stefano N, Iannucci G, Sormani MP, Guidi L, Bartolozzi ML, Comi G, Federico A, Filippi M (2002) MR correlates of cerebral atrophy in patients with multiple sclerosis. J Neurol 249:1072-077
De Stefano N, Matthews PM, Fu LQ, Narayanan S, Stanley J, Francis GS, Antel JP, Arnold DL (1998) Axonal damage correlates with disability in patients with relapsing-remitting multiple sclerosis - Results of a longitudinal magnetic resonance spectroscopy study. Brain 121:1469-477
De Stefano N, Narayanan S, Francis GS, Arnaoutelis R, Tartaglia MC, Antel JP, Matthews PM, Arnold DL (2001) Evidence of axonal damage in the early stages of multiple sclerosis and its relevance to disability. Arch Neurol 58:65-0
Evangelou N, Konz D, Esiri MM, Smith S, Palace J, Matthews PM (2000) Regional axonal loss in the corpus callosum correlates with cerebral white matter lesion volume and distribution in multiple sclerosis. Brain 123(Pt 9):1845-849
Ferguson B, Matyszak MK, Esiri MM, Perry VH (1997) Axonal damage in acute multiple sclerosis lesions. Brain 120:393-99
Fu L, Matthews PM, De Stefano N, Worsley KJ, Narayanan S, Francis GS, Antel JP, Wolfson C, Arnold DL (1998) Imaging axonal damage of normalappearing white matter in multiple sclerosis. Brain 121:103-13
Jakobs C, ten Brink HJ, Langelaar SA, Zee T, Stellaard F, Macek M, Srsnova K, Srsen S, Kleijer WJ (1991) Stable isotope dilution analysis of N-acetylaspartic acid in CSF, blood, urine and amniotic fluid: accurate postnatal diagnosis and the potential for prenatal diagnosis of Canavan disease. J Inherit Metab Dis 14:653-60
Kalkers NF, De Groot V, Lazeron RHC, Killestein J, Ader HJ, Barkhof F, Lankhorst GJ, Polman CH (2000) MS Functional Composite - Relation to disease phenotype and disability strata. Neurology 54:1233-239
Kornek B, Storch MK, Weissert R, Wallstroem E, Stefferl A, Olsson T, Linington C, Schmidbauer M, Lassmann H (2000) Multiple sclerosis and chronic autoimmune encephalomyelitis: a comparative quantitative study of axonal injury in active, inactive, and remyelinated lesions. Am J Pathol 157:267-76
Kurtzke JF (1983) Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 33:1444-452
Lublin FD, Reingold SC (1996) Defining the clinical course of multiple sclerosis: Results of an international survey. Neurology 46:907-11
Miller DH, Barkhof F, Frank JA, Parker GJ, Thompson AJ (2002) Measurement of atrophy in multiple sclerosis: pathological basis, methodological aspects and clinical relevance. Brain 125:1676-695
Oestreicher AB, De Graan PN, Gispen WH, Verhaagen J, Schrama LH (1997) B-50, the growth associated protein-43: modulation of cell morphology and communication in the nervous system. Prog Neurobiol 53:627-86
Poser CM, Paty DW, Scheinberg L, Mcdonald WI, Davis FA, Ebers GC, Johnson KP, Sibley WA, Silberberg DH, Tourtellotte WW (1983) New Diagnostic-Criteria for Multiple-Sclerosis - Guidelines for Research Protocols. Ann Neurol 13:227-31
Smith SM, Zhang YY, Jenkinson M, Chen J, Matthews PM, Federico A, De Stefano N (2002) Accurate, robust, and automated longitudinal and cross-sectional brain change analysis. Neuroimage 17:479-89
Teunissen CE, Dijkstra C, Polman C (2005) Biological markers in CSF and blood for axonal degeneration in multiple sclerosis. Lancet Neurol 4:32-1
Teunissen CE, Dijkstra CD, Jasperse B, Barkhof F, Vanderstichele H, Vanmechelen E, Polman CH, Bo L (2006) Growth-associated protein 43 in lesions and cerebrospinal fluid in multiple sclerosis. Neuropathol Appl Neurobiol 32:318-31
Trapp BD, Peterson J, Ransohoff RM, Rudick R, Mork S, Bo L (1998) Axonal transection in the lesions of multiple sclerosis. N Engl J Med 338:278-85
Trapp BD, Ransohoff R, Rudick R (1999) Axonal pathology in multiple sclerosis: relationship to neurologic disability. Curr Opin Neurol 12:295-02
van Walderveen MAA, Barkhof F, Pouwels PJW, van Schijndel RA, Polman CH, Castelijns JA (1999) Neuronal damage in T1-hypointense multiple sclerosis lesions demonstrated in vivo using proton magnetic resonance spectroscopy. Ann Neurol 46:79-7
Vrenken H, Barkhof F, Uitdehaag BM, Castelijns JA, Polman CH, Pouwels PJ (2005) MR spectroscopic evidence for glial increase but not for neuro-axonal damage in MS normal-appearing white matter. Magn Reson Med 53:256-66
Acknowledgement
We thank W. Giese en U. Holverda for assisting in laboratory measurements, S. de Vries for assisting with MR analysis and the subjects who participated in this study. This study (grant number 97-310 MS) and Dr. C.E. Teunissen (grant number 02-358 bMS) are supported by the Dutch MS Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Jasperse, B., Jakobs, C., Eikelenboom, M.J. et al. N-acetylaspartic acid in cerebrospinal fluid of multiple sclerosis patients determined by gas-chromatography-mass spectrometry. J Neurol 254, 631–637 (2007). https://doi.org/10.1007/s00415-006-0415-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-006-0415-5