Abstract
Introduction
Late-onset Pompe disease (LOPD) is characterized by progressive skeletal and respiratory muscle weakness. Little is known about the effect of inspiratory muscle training (IMT) on pulmonary function in subjects with LOPD. The aim of the present study was to investigate the effect of an 8-week IMT program on pulmonary function tests, quality of life, and sleep quality in eight patients with LOPD who were receiving enzyme replacement therapy (ERT).
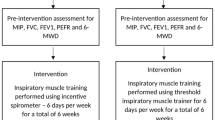
Methods
Before and after the IMT program, spirometric measurements in sitting and supine positions, and measurements of maximum inspiratory and expiratory pressures, peak cough flow, quality of life (assessed using the Nottingham Health Profile), and sleep quality (assessed using the Pittsburgh sleep quality index) were performed.
Results
A significant increase in maximum inspiratory pressure (cmH2O and % predicted) (median [interquartile range]: 30.0 cmH2O [21.5–48] versus 39 cmH2O [31.2–56.5] and 38.3 % [28.1–48.4] versus 50.5 % [37.7–54.9]) was observed after training (p = 0.01). There were no significant changes in the other pulmonary function measurements. With the exception of the social isolation subscore (p = 0.02), quality of life subscores did not change after IMT (p > 0.05). Sleep quality subscores and total scores were similar before and after IMT.
Conclusion
These results suggest that IMT has a positive effect on maximum inspiratory pressure in subjects with LOPD who are under ERT.
Similar content being viewed by others
References
Bembi B, Cerini E, Danesino C et al (2008) Diagnosis of glycogenosis type II. Neurology 71(23 Suppl 2):S4–S11. doi:10.1212/WNL.0b013e31818da91e
Kishnani PS, Steiner RD, Bali D et al (2006) Pompe disease diagnosis and management guideline. Genet Med 8(5):267–288. doi:10.1097/01.gim.0000218152.87434.f3
van der Ploeg AT, Reuser AJ (2008) Pompe’s disease. Lancet (Lond) 372(9646):1342–1353. doi:10.1016/s0140-6736(08)61555-x
Gungor D, Reuser AJ (2013) How to describe the clinical spectrum in Pompe disease? Am J Med Genet A 161(2):399–400. doi:10.1002/ajmg.a.35662
Kishnani PS, Howell RR (2004) Pompe disease in infants and children. J Pediatr 144(5 Suppl):S35–S43. doi:10.1016/j.jpeds.2004.01.053
Vianello A, Semplicini C, Paladini L et al (2013) Enzyme replacement therapy improves respiratory outcomes in patients with late-onset type II glycogenosis and high ventilator dependency. Lung 191(5):537–544. doi:10.1007/s00408-013-9489-x
Hagemans ML, Winkel LP, Van Doorn PA et al (2005) Clinical manifestation and natural course of late-onset Pompe’s disease in 54 Dutch patients. Brain 128(3):671–677. doi:10.1093/brain/awh384
Hagemans ML, Winkel LP, Hop WC et al (2005) Disease severity in children and adults with Pompe disease related to age and disease duration. Neurology 64(12):2139–2141. doi:10.1212/01.wnl.0000165979.46537.56
Winkel LP, Hagemans ML, van Doorn PA et al (2005) The natural course of non-classic Pompe’s disease; a review of 225 published cases. J Neurol 252(8):875–884. doi:10.1007/s00415-005-0922-9
Mellies U, Stehling F, Dohna-Schwake C et al (2005) Respiratory failure in Pompe disease: treatment with noninvasive ventilation. Neurology 64(8):1465–1467. doi:10.1212/01.wnl.0000158682.85052.c0
Mellies U, Ragette R, Schwake C et al (2001) Sleep-disordered breathing and respiratory failure in acid maltase deficiency. Neurology 57(7):1290–1295
Margolis ML, Howlett P, Goldberg R et al (1994) Obstructive sleep apnea syndrome in acid maltase deficiency. Chest 105(3):947–949
Katzin LW, Amato AA (2008) Pompe disease: a review of the current diagnosis and treatment recommendations in the era of enzyme replacement therapy. J Clin Neuromuscul Dis 9(4):421–431. doi:10.1097/CND.0b013e318176dbe4
Mellies U, Lofaso F (2009) Pompe disease: a neuromuscular disease with respiratory muscle involvement. Respir Med 103(4):477–484. doi:10.1016/j.rmed.2008.12.009
Hagemans ML, Janssens AC, Winkel LP et al (2004) Late-onset Pompe disease primarily affects quality of life in physical health domains. Neurology 63(9):1688–1692
Ambrosino N, Confalonieri M, Crescimanno G et al (2013) The role of respiratory management of Pompe disease. Respir Med 107(8):1124–1132. doi:10.1016/j.rmed.2013.03.004
Nici L, Donner C, Wouters E et al (2006) American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med 173(12):1390–1413. doi:10.1164/rccm.200508-1211ST
Jones HN, Moss T, Edwards L et al (2011) Increased inspiratory and expiratory muscle strength following respiratory muscle strength training (RMST) in two patients with late-onset Pompe disease. Mol Genet Metab 104(3):417–420. doi:10.1016/j.ymgme.2011.05.006
Jones HN, Crisp KD, Robey RR et al (2016) Respiratory muscle training (RMT) in late-onset Pompe disease (LOPD): effects of training and detraining. Mol Genet Metab 117(2):120–128. doi:10.1016/j.ymgme.2015.09.003
Holden MK, Gill KM, Magliozzi MR et al (1984) Clinical gait assessment in the neurologically impaired. Reliability and meaningfulness. Phys Ther 64(1):35–40
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories (2002) ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166(1):111–117. doi:10.1164/ajrccm.166.1.at1102
Enright PL, Sherrill DL (1998) Reference equations for the six-minute walk in healthy adults. Am J Respir Crit Care Med 158(5 Pt 1):1384–1387. doi:10.1164/ajrccm.158.5.9710086
Miller MR, Hankinson J, Brusasco V et al (2005) Standardisation of spirometry. Eur Respir J 26(2):319–338. doi:10.1183/09031936.05.00034805
Quanjer PH, Tammeling GJ, Cotes JE et al (1993) Lung volumes and forced ventilatory flows. Eur Respir J 6(Suppl 16):5–40. doi:10.1183/09041950.005s1693
Allen SM, Hunt B, Green M (1985) Fall in vital capacity with posture. Br J Dis Chest 79(3):267–271
Fromageot C, Lofaso F, Annane D et al (2001) Supine fall in lung volumes in the assessment of diaphragmatic weakness in neuromuscular disorders. Arch Phys Med Rehabil 82(1):123–128. doi:10.1053/apmr.2001.18053
American Thoracic Society (2002) ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med 166(4):518–624. doi:10.1164/rccm.166.4.518
Black LF, Hyatt RE (1969) Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis 99(5):696–702
Bianchi C, Baiardi P (2008) Cough peak flows: standard values for children and adolescents. Am J Phys Med Rehabil 87(6):461–467. doi:10.1097/PHM.0b013e318174e4c7
Gauld LM, Boynton A (2005) Relationship between peak cough flow and spirometry in Duchenne muscular dystrophy. Pediatr Pulmonol 39(5):457–460. doi:10.1002/ppul.20151
Hunt SM, McKenna SP, McEwen J et al (1981) The Nottingham Health Profile: subjective health status and medical consultations. Soc Sci Med A 15(3 Pt 1):221–229
Kucukdeveci AA, McKenna SP, Kutlay S et al (2000) The development and psychometric assessment of the Turkish version of the Nottingham Health Profile. Int J Rehabil Res 23(1):31–38
Buysse DJ, Reynolds CF, Monk TH et al (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Agargun MYKH, Anlar O (1996) Pittsburgh Uyku Kalitesi İndeksinin geçerliliği ve güvenilirliği. Türk Psikiyatri Dergisi 7:107–115
Topin N, Matecki S, Le Bris S et al (2002) Dose-dependent effect of individualized respiratory muscle training in children with Duchenne muscular dystrophy. Neuromuscul Disord NMD 12(6):576–583
Koessler W, Wanke T, Winkler G et al (2001) 2 Years’ experience with inspiratory muscle training in patients with neuromuscular disorders. Chest 120(3):765–769
Yeldan I, Gurses HN, Yuksel H (2008) Comparison study of chest physiotherapy home training programmes on respiratory functions in patients with muscular dystrophy. Clin Rehabil 22(8):741–748. doi:10.1177/0269215508091203
Aslan GK, Gurses HN, Issever H et al (2013) Effects of respiratory muscle training on pulmonary functions in patients with slowly progressive neuromuscular disease: a randomized controlled trial. Clin Rehabil 28(6):573–581. doi:10.1177/0269215513512215
Wanke T, Toifl K, Merkle M et al (1994) Inspiratory muscle training in patients with Duchenne muscular dystrophy. Chest 105(2):475–482
Fregonezi GA, Resqueti VR, Guell R et al (2005) Effects of 8-week, interval-based inspiratory muscle training and breathing retraining in patients with generalized myasthenia gravis. Chest 128(3):1524–1530. doi:10.1378/chest.128.3.1524
Jones HN, Crisp KD, Moss T et al (2014) Effects of respiratory muscle training (RMT) in children with infantile-onset Pompe disease and respiratory muscle weakness. J Pediatr Rehabil Med 7(3):255–265. doi:10.3233/prm-140294
Gosselink R (2004) Breathing techniques in patients with chronic obstructive pulmonary disease (COPD). Chron Respir Dis 1(3):163–172
Smith BK, Collins SW, Conlon TJ et al (2013) Phase I/II trial of adeno-associated virus-mediated alpha-glucosidase gene therapy to the diaphragm for chronic respiratory failure in Pompe disease: initial safety and ventilatory outcomes. Hum Gene Ther 24(6):630–640. doi:10.1089/hum.2012.250
Boentert M, Karabul N, Wenninger S et al (2015) Sleep-related symptoms and sleep-disordered breathing in adult Pompe disease. Eur J Neurol 22 (2):369–376, e327. doi:10.1111/ene.12582
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None.
Rights and permissions
About this article
Cite this article
Aslan, G.K., Huseyinsinoglu, B.E., Oflazer, P. et al. Inspiratory Muscle Training in Late-Onset Pompe Disease: The Effects on Pulmonary Function Tests, Quality of Life, and Sleep Quality. Lung 194, 555–561 (2016). https://doi.org/10.1007/s00408-016-9881-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-016-9881-4