Abstract
The clinical course of patients undergoing prolonged mechanical ventilation is often complicated by the development of purulent tracheobronchitis. The purpose of this study was to assess whether ventilator-associated hypersecretion is associated with elevated levels of tissue kallikrein (TK) activity. TK can induce marked bronchial inflammation in animal models and TK activity is increased in the airway secretions of symptomatic asthmatics. It has not been studied in conditions with predominantly neutrophilic bronchial secretions, although animal data indicate that neutrophil elastase may stimulate TK activity. We measured TK activity in airway secretions of patients undergoing mechanical ventilation for more than 4 weeks (PMV group) and in two comparator groups: patients with cystic fibrosis, who were colonized with Pseudomonas aeruginosa (CF group) and patients undergoing mechanical ventilation for less than one week who did not have clinical evidence of purulent airway secretions (acute mechanical ventilation, AMV group). We also compared the level of neutrophil elastase (NE) activity, an index of neutrophil activation, in the three patient groups. TK and NE activity in the sol phase were measured by the degradation of chromogenic substrates (DL Val-Leu-Arg pNA and N-Methoxy Succinyl Ala-Ala-Pro-Val pNA, respectively). Intergroup differences in cell counts were not significant. However, TK activity was significantly less in the AMV group than in the PMV and cystic fibrosis patients (Kruskal-Wallis ANOVA, p < 0.05). Elastase activity was significantly greater in the CF group (p < 0.05) than in the other two groups. Compared to patients undergoing short-term mechanical ventilation (AMV group), TK activity was elevated in patients with purulent tracheobronchitis associated with prolonged mechanical ventilation (PMV group). The elevation in TK activity in these patients is comparable to levels in sputum from patients with cystic fibrosis (CF group), although the latter had a significantly higher level of NE activity. The observation of increased TK activity in patients with neutrophilic airway inflammation suggests that TK may play a role in modulating inflammation in ventilator-associated tracheobronchitis and may be worthy of further study to determine its source and significance.
Similar content being viewed by others
Introduction
Tissue kallikrein (TK) is a generic term for a family of serine proteases that cleave kininogen and release bradykinin (BK) and lys-bradykinin [18]. Tissue kallikrein is expressed in many mammalian tissues including submucosal glands, respiratory epithelium [3, 7, 10, 18] and neutrophils [16]. It acts locally in the tissues where it is produced and does not circulate in blood to any appreciable extent. The kinins results from TK activity are capable of inducing vasodilation, increased vascular permeability, edema, and smooth muscle contraction (including smooth muscle in mucous glands) and may play a role in neutrophil migration. Studies in patients with rheumatoid arthritis indicate that levels of TK activity are increased in synovial fluid in this condition and that the source appears to be the neutrophil [16]. Kinins can also alter ion transport in glandular tissue and change the composition of airway secretions [8]. Tissue kallikrein is regulated in a tissue-specific manner, possibly by neural mechanisms [7, 18], and the inflammation and mucosal edema that are mediated by kinin activity can be prolonged [4]. Though clinical studies have demonstrated that TK is increased in the airway secretions of patients with asthma [5] and allergic rhinitis [6], levels that are further increased after antigen challenge, it is not known if elevated TK activity is associated with airway inflammation in which the neutrophil is the predominant cell type. However, animal data indicate that TK activity can be stimulated by neutrophil elastase [14], thus suggesting a possible mechanism by which TK activity could be increased in this population.
The present study was designed to determine if elevated TK activity is associated with the hypersecretion that develops in patients undergoing prolonged mechanical ventilation. The clinical course of such patients is often complicated by the development of tracheobronchitis, manifested clinically by the production of airway secretions that are frequently both copious and purulent [2, 11, 12, 13]. This bronchorrhea complicates the process of weaning from the ventilator both by contributing to atelectasis and by possibly predisposing to nosocomial pneumonia. The etiology of the hypersecretion is poorly understood. Bacterial infection, mechanical irritation of the airway mucosa, impairment of mucociliary and cough clearance and the effects of host inflammatory responses to infection and irritation may all be involved. Treatment of this problem is often unsatisfactory, and the development of effective therapeutic options for this condition will necessitate a clearer understanding of the role of host inflammatory responses.
Because TK could potentially be a significant contributor to the inflammatory process that characterizes tracheobronchitis, we measured TK activity in patients with purulent tracheobronchitis who were undergoing prolonged mechanical ventilation. As comparator groups, we measured TK activity in patients with another condition associated with purulent lower airway secretions (cystic fibrosis patients whose airways had been colonized with Pseudomonas aeruginosa), and in patients who were undergoing mechanical ventilation for less than one week and who did not have clinical evidence of purulent airway secretions. In addition, we compared cell counts and the levels of neutrophil elastase activity, an index of neutrophil activation and a possible stimulus for TK secretion [14] in the airway secretions of these three patient groups.
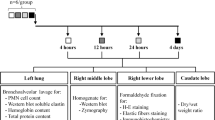
Methods
Subjects Undergoing Prolonged Mechanical Ventilation
Tracheal aspirates were obtained from 22 patients at a long-term ventilator facility. All patients in the study had required ventilatory support for greater than one month and all had undergone tracheostomy within their current hospitalization. Patients ranged in age from 64 to 91 years. All had colonization of the tracheobronchial tree with gram-negative organisms (Pseudomonas aeruginosa, Klebsiella sp., Serratia sp. Enterobacter sp., Acinetobacter sp., Escherichia coli) and/or Staphylococcus aureus and almost all were currently receiving or had received systemic antibiotic therapy within the preceding three weeks. The majority of these patients had complex past medical histories. The most common reasons for their prolonged requirement for mechanical ventilatory support were anoxic encephalopathy, recurrent septicemia, recurrent aspiration pneumonia, cerebrovascular accident, congestive cardiac failure, chronic obstructive pulmonary disease and complications of thoracic and abdominal surgery.
Subjects Undergoing Acute Mechanical Ventilation
Tracheal aspirates were obtained from 13 patients (aged 31–82 years) in a Medical Intensive Care Unit. All had required endotracheal intubation and mechanical ventilatory support for less than one week. Four patients were receiving IV antibiotics at the time that samples were collected. The etiology of respiratory failure in these patients included anoxic encephalopathy, intracranial hemorrhage, cardiac failure, post-coronary artery revascularization, gastrointestinal hemorrhage, meningitis and diabetic ketoacidosis. One patient had experienced a near-drowning event and one had had an exacerbation of chronic obstructive pulmonary disease. No patients had radiographic evidence of pneumonia and none had clinical evidence of purulent secretions.
Subjects with Cystic Fibrosis
Sputum samples were obtained from 12 patients with cystic fibrosis during their scheduled visits to a Cystic Fibrosis Ambulatory Care Clinic. Patients ranged in age from 9 to 32 years and were clinically stable at the time of study. All had chronic colonization of sputum by Pseudomonas aeruginosa and all but two of the patients were on long-term oral antibiotic therapy (ciprofloxacin) at the time of the study. Diagnosis of CF had been based upon a characteristic clinical history and a positive sweat test.
Initial Sample Processing
Sample collection protocols and informed consent procedures were approved by the University of Miami Institutional Review Board. Tracheal aspirates were obtained during scheduled suctioning of mechanically ventilated patients using a previously described method [13, 14]. No saline was instilled and suctioning was performed for 30 sec or until no further secretions could be obtained. Sputum was obtained from CF patients who were instructed to expectorate a sample as free from salivary contamination as possible, into a clean specimen cup. Patients unable to provide sputum spontaneously underwent chest physiotherapy for 20 min and were subsequently able to produce specimens. Upon collection, specimens were placed in an ice-filled container to minimize autolytic activity and were processed within 1 hour.
Total Cell Counts and Differential
Tracheal aspirates were briefly vortexed until of homogeneous appearance. An aliquot was then removed, weighed and diluted with 10 ml of phosphate-buffered saline (PBS). Sputum specimens were examined and plugs were identified, removed and weighed in a manner previously described [13, 14]. As above, these plugs were diluted with 10 ml of PBS. The diluted specimen was first gently shaken (manually) and then pipetted until uniformly dispersed. Total cell count (TCC) was performed on the diluted specimen using a hemocytometer. TCC was expressed as cells per gram of airway secretion. Cell viability was determined by Trypan Blue exclusion. A separate aliquot of the diluted specimen was centrifuged onto a slide using a Cytospin centrifuge and then stained with Diff-Quik (modified Giemsa) for differential cell analysis.
Sol Phase Analysis
The remainder of the whole sputum/aspirate was ultracentrifuged at 50,000 RPM for 1.5 h at 4°C to separate the sol and gel phases. The supernatant (sol phase) was carefully aspirated and stored at −80°C until analyzed; the pellet was discarded.
Assay for Tissue Kallikrein Activity
Detection of tissue kallikrein enzymatic activity utilized the chromogenic substrate DL Val-Leu-Arg pNA (Sigma Chemical Co., St. Louis, Mo.). A sol sample of 50 µl was diluted with 100 µl of Trizma (0.05 M) buffer (pH 8.2). Then, 100 µl of substrate was added and the change in optical density over 1 h was measured at 410 nm in a microtiter plate. Results represent the average of triplicate determinations.
Assay for Human Leukocyte Elastase Activity
A sol sample of 50 µl was diluted with 100 µl of Trizma (0.2 M) buffer (pH8.8). Then, 50 µl of the chromogenic substrate N-Methoxy Succinyl Ala-Ala-Pro-Val pNA (Sigma Chemical Co., St. Louis, MO.) were added and the change in optical density over 1 h was measured at 410 nm in a microtiter plate. Results represent the average of triplicate determinations.
Statistics
For each experiment, data were analyzed using Kruskal-Wallis nonparametric analysis of variance [1]. If the null hypothesis was rejected, then pairwise comparisons were made using Mann-Whitney two-sample tests. Using two-tailed tests, a value of p < 0.05 was considered significant.
Results
Total and Differential Cell Counts
Total and differential cell counts are shown in Table 1. There was no significant difference in total cell counts among the three study groups. Likewise, all groups demonstrated a predominance of neutrophils with no significant differences in percentage of neutrophils among the groups. Percentage cell viabilities (mean ± SE) were 64.7 ± 14.3%, 74.9 ± 18.6% and 83.9 ± 6.4% for patients with cystic fibrosis, patients undergoing prolonged mechanical ventilation and patients undergoing acute mechanical ventilation, respectively.
Tissue Kallikrein Activity
Tissue kallikrein activity is reported in Table 1. It was significantly less in tracheal aspirates from acutely mechanically ventilated patients (median change in optical density units (ΔO.D.u.) = 0.051, p < 0.05 versus other groups) than in either tracheal aspirates from patients undergoing prolonged mechanical ventilation (median ΔO.D.u. = 0.139) or sputum from patients with cystic fibrosis (median ΔO.D.u. = 0.189). There was no significant difference in TK activity between prolonged mechanical ventilation and cystic fibrosis groups.
Elastase Activity
Elastase activity (Table 1) was significantly greater in CF sputum (median ΔO.D.u. = 1.205, p < 0.05) than in tracheal aspirates from patients undergoing either acute or prolonged mechanical ventilation (median ΔO.D.u. = 0.015 and 0.014, respectively). There was no significant difference in elastase activity between the two mechanical ventilation groups.
Discussion
The findings of the present study demonstrate that compared to patients undergoing short-term mechanical ventilation, TK activity is elevated in patients with purulent tracheobronchitis associated with prolonged mechanical ventilation. The elevation in TK activity is comparable to levels measured in sputum from patients with cystic fibrosis whose airways were colonized with Pseudomonas aeruginosa and who had a significantly higher level of NE activity than the patients in the two ventilator groups.
There are a number of possible explanations for differences in TK levels between the acute ventilator patients and the PMV patients. One explanation may be that the TK activity may be an index of inflammation caused by the effects of prolonged intubation (e.g., bacterial colonization and chronic infection, suction trauma, oxygen toxicity, mucociliary dysfunction). Alternatively, the elevation in TK activity may represent a predisposition to develop hypersecretion due to preexisting bronchial disease, and TK activity may be a reflection of preexisting but subclinical submucosal gland dysfunction. A combination of these two factors is also possible and prospective measurement of TK in patients at risk of requiring prolonged mechanical ventilation may be an appropriate way to further clarify this issue. Finally, as suggested above, there may be an unidentified mediator in the sputum of the PMV patients that stimulates TK secretion.
Elevated levels of TK activity were demonstrated in both of the groups with purulent airway secretions (PMV and CF). Despite similar numbers of neutrophils in the secretions of the two groups, NE activity was higher in the secretions of the patients with CF. The finding of increased NE activity in the CF sputum samples, despite similar neutrophil counts, is most likely explained by a higher turnover of neutrophils in the CF patients, resulting in the degranulated NE persisting after the intact neutrophil has ceased to exist. Though animal data indicate that NE can stimulate TK secretion [14], a significant correlation between NE activity and TK activity was not observed in these populations. This could indicate that the neutrophils in the CF secretions had a greater degree of activation and that there may be different stimuli involved in TK and elastase secretion. Alternatively, alginate associated with the strains of mucoid Pseudomonas aeruginosa that occur in CF sputum may have interfered with protease/anti-protease binding and contributed to the detection of free elastase activity in the CF patients’ sputum [17]. While the bacterial protease level may have been greater in the CF samples, the elastase assay was specific for serine proteases and bacterial proteases would not have affected the results.
The secretions obtained from the AMV and PMV group were suctioned directly from the lower airways, thereby minimizing the likelihood of contamination of lower airway secretions with saliva, which is known to contain TK activity [9]. While the CF samples were obtained from sputum collection rather than from direct aspiration of the lower airway secretions, the purulent appearance of the CF sputum facilitated the identification and removal of plugs of purulent lower airway secretions from the specimens, thus reducing the risk of salivary contamination. TK activity has been reported in saliva of patients with CF at levels similar to those seen in healthy volunteers [9].
The source of the detectable TK activity in the airway secretions of the PMV and CF patients is unknown. The enzyme has been reported to be expressed in mammalian respiratory tissues. It is present in the seromucous glands of the human nasal epithelium [3] and in the serous cells of submucosal glands of the guinea pig trachea [18]. Submucosal glands are more prominent in central airways and become hypertrophied in the presence of chronic inflammatory stimuli [15]. Hence, the TK activity may reflect submucosal gland hypertrophy/hypersecretion in the PMV-associated purulent tracheobronchitis and in those with cystic fibrosis. Furthermore, previous studies that have reported increased expression of kinin receptors on glandular epithelium and that have demonstrated the ability of kinins to influence ion transport [8] suggest a possible role for TK in mediating hypersecretion. Kinins are potent local mediators that induce vasodilation, increase vascular permeability and cause edema. Neutrophils can be another source of TK activity. While the number of neutrophils per unit volume of secretions was similar in all groups, the total number of neutrophils present in the sputum of the patients with short-term intubation was less than the PMV and CF groups because the volume of secretions was scant. The observation of increased TK activity in patients with neutrophilic airway inflammation suggests that TK may play a role in modulating inflammation in ventilator-associated tracheobronchitis and may be worthy of further study to determine its source and significance.
References
DG Altman (1991) Practical tests for medical research. Chapman and Hall London 194–197
JG Bartlett LJ Faling S Willey (1978) ArticleTitleQuantitative tracheal bacteriologic and cytologic studies in patients with long-term tracheostomies. Chest 74 635–393 Occurrence Handle1:STN:280:CSaC3cnls1E%3D Occurrence Handle738121
CR Baumgarten R Schwarting G Kunkel (1990) ArticleTitleLocalization of glandular kallikrein in nasal mucosa of allergic and nonallergic individuals. Adv Exp Biol 247B 523–528
LM Chen L Chao RK Mayfield J Chao (1990) ArticleTitleDifferential interactions of human kallikrein binding protein and alpha 1 anti-trypsin with human tissue kallikrein. Biochem J 267 79–84 Occurrence Handle1:CAS:528:DyaK3cXktVantr4%3D Occurrence Handle2327990
SC Christiansen D Proud CG Cochrane (1987) ArticleTitleDetection of tissue kallikrein in the bronchoalveolar lavage fluid of asthmatic subjects. J Clin Invest 79 188–197 Occurrence Handle1:CAS:528:DyaL2sXot12isQ%3D%3D Occurrence Handle3540008
SC Christiansen J Eddleston KM Woessner SS Chambers R Ye ZK Pan BL Zuraw (2002) ArticleTitleUp-regulation of functional kinin B1 receptors in allergic airway inflammation. J Immunol 169 2054–2060 Occurrence Handle1:CAS:528:DC%2BD38XmtFejtr4%3D Occurrence Handle12165532
JA Clements BA Matheson JW Funder (1990) ArticleTitleTissue-specific developmental expression of the human kallikrein gene family in rats. J Biol Chem 265 1077–1081 Occurrence Handle1:CAS:528:DyaK3cXlt1ymsw%3D%3D Occurrence Handle2295600
GM Denning MJ Welsh (1991) ArticleTitlePolarized distribution of bradykinin receptors on airway epithelial cells and independent coupling to second messinger pathways. J Biol Chem 266 12932–12938 Occurrence Handle1:CAS:528:DyaK3MXkvVKiurg%3D Occurrence Handle1649170
ER Hare JA Verpoorte (1985) ArticleTitleComparative studies on salivary kallikrein from cystic fibrosis patients and controls. Pediatric Res 938–943
SR Murray J Chao FK Lun L Chao (1990) ArticleTitleKallikrein multigene families and the regulation of their expression. J Cardivasc Pharmacol 15 S7–S16 Occurrence Handle1:CAS:528:DyaK3cXkslagtLk%3D
MS Niederman RD Ferranti A Zeigler WW Merrill HY Reynolds (1984) ArticleTitleRespiratory infection complicating long-term tracheostomy: the implication of persistent gram-negative tracheobronchial colonization. Chest 85 39–44 Occurrence Handle1:STN:280:BiuD1czlsFA%3D Occurrence Handle6690250
LB Palmer GC Smaldone S Simon TG O’Riordan L Morra (1995) ArticleTitleTracheal aspirates in chronically mechanically ventilated patients: a human model of gram-negative infection and airway inflammation. Chest 106 1326–1332
LB Palmer GC Smaldone SR Simon TG O’Riordan A Cuccia (1998) ArticleTitleAerosolized antibiotics in mechanically ventilated patients. Crit Care Med 26 31–39 Occurrence Handle1:STN:280:DyaK1c%2FovVyitA%3D%3D Occurrence Handle9428540
M Scuri R Forteza I Lauredo JR Sabater Y Botvinnikova L Allegra WM Abraham (2000) ArticleTitleInhaled porcine pancreatic elastase causes bronchoconstriction via a bradykinin-mediated mechanism. J Appl Physiol 89 1397–1402 Occurrence Handle1:CAS:528:DC%2BD3cXotlyltbc%3D Occurrence Handle11007574
A Wanner M Salathe TG O’Riordan (1996) ArticleTitleState of the art. Mucociliary clearance in the airways. Am J Respir Crit Care Med 154 1868–1902 Occurrence Handle1:STN:280:ByiC38rjtVA%3D Occurrence Handle8970383
RJ Williams LM Henderson Y Naidoo B Cassim CJ Elson KD Bhoola (1997) ArticleTitleImmunocytochemical analysis of tissue kallikrein and the kinin moiety in rheumatoid synovial fluid neutrophils. Br J Rheumatol 36 420–425 Occurrence Handle10.1093/rheumatology/36.4.420 Occurrence Handle1:CAS:528:DyaK2sXjvFeitr0%3D Occurrence Handle9159533
QL Ying M Kemme SR Simon (1996) ArticleTitleAlginate, the slime exopolysaccharide of Pseudomonas aeruginosa binds human leukocyte elastase, retards inhibition by a1 proteinase inhibitor, and accelerates inhibition by secretory leukoprotease inhibitor. Am J Respir Cell Mol Biol 15 283–291 Occurrence Handle1:CAS:528:DyaK28XltVaktro%3D Occurrence Handle8703486
BL Zuraw SC Christiansen (1995) Kinins. ST Holgate WW Busse (Eds) Asthma and rhinitis. Blackwell Boston 861–883
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
O’Riordan, T., Weinstein, M., Abraham, W. et al. Elevated Tissue Kallikrein Activity in Airway Secretions from Patients with Tracheobronchitis Associated with Prolonged Mechanical Ventilation . Lung 181, 237–244 (2003). https://doi.org/10.1007/s00408-003-1019-9
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s00408-003-1019-9