Abstract
Ketamine exerts its rapid antidepressant effects via modulation of the glutamatergic system. While numerous imaging studies have investigated the effects of ketamine on a functional macroscopic brain level, it remains unclear how altered glutamate metabolism and changes in brain function are linked. To shed light on this topic we here conducted a multimodal imaging study in healthy volunteers (N = 23) using resting state fMRI and proton (1H) magnetic resonance spectroscopy (MRS) to investigate linkage between metabolic and functional brain changes induced by ketamine. Subjects were investigated before and during an intravenous ketamine infusion. The MRS voxel was placed in the pregenual anterior cingulate cortex (pgACC), as this region has been repeatedly shown to be involved in ketamine’s effects. Our results showed functional connectivity changes from the pgACC to the right frontal pole and anterior mid cingulate cortex (aMCC). Absolute glutamate and glutamine concentrations in the pgACC did not differ significantly from baseline. However, we found that stronger pgACC activation during ketamine was linked to lower glutamine concentration in this region. Furthermore, reduced functional connectivity between pgACC and aMCC was related to increased pgACC activation and reduced glutamine. Our results thereby demonstrate how multimodal investigations in a single brain region could help to advance our understanding of the association between metabolic and functional changes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last 2 decades, ketamine has become an important research tool to investigate rapid antidepressant mechanisms of action [1]. It has been repeatedly shown that antidepressant effects of ketamine occur within 24 h after a single dose [2]. On the one hand, this allows for the study of antidepressant mechanisms, as it enables to establish a direct link between the drug and its effects. But on the other, the molecular and systemic changes ketamine induces in the central nervous system are notoriously complex and it is a matter of ongoing research to pin down which of these changes bring forward the antidepressant effects. Despite many unanswered questions, there is a broad consensus that the antidepressant effects of ketamine are linked to changes in the glutamatergic system [3], and there is evidence that altered glutamatergic signaling leads to intercellular signaling cascades that induce synaptic plasticity, which has been associated with ketamine’s antidepressant effects in behavioral animal models [4]. Furthermore, a considerable amount of imaging studies investigated the effects of ketamine on functional brain activations and networks in humans [5]. Although the results of this research have not yet converged, and no clear antidepressant mechanism of action has been identified, some interesting themes and involved brain regions, such as the anterior cingulate cortex [6], have emerged. However, evidence remains sparse how ketamine-induced molecular changes in the glutamatergic system are linked to macroscopic functional activation and network changes in the human brain.
Considering the important role of glutamate (Glu) in synaptic transmission and plasticity, perturbation of the glutamatergic system is considered one of the factors involved in the pathophysiology of depression, while Glu modulation may induce rapid relief of depressive symptoms [7,8,9]. Glutamate is synthesized in the presynaptic terminal from glutamine (Gln), and then released into the synaptic cleft. Astrocytes provide the primary mechanism for clearance from the synaptic cleft, by means of uptake by amino acid transporters. Once in the astrocyte, Glu is converted to Gln by the Gln synthetase. Gln is then released into the extracellular space for uptake into the excitatory and the inhibitory neurons, where it is converted back to Glu via glutaminase. This is referred to as the glutamate/glutamine cycle [10]. Astrocytic pathology and subsequent alterations in this cycle have been implicated in the physiology of depression [9, 11] with astrocyte-related reductions in conversion of Glu to Gln leading to downstream Glu reduction [12]. Proton (1H) magnetic resonance spectroscopy (MRS) is the only non-invasive method able to directly measure glutamate and glutamine levels in vivo. In some MRS studies, elevated Gln and Glu levels have been linked to depression, while other studies reported reduced concentrations of both Gln and Glu [13,14,15,16,17,18]. As it is difficult to separate Glu clearly from its precursor and metabolite, Gln, the two compounds are often measured together as Glx and accordingly, inconsistent alterations in Glx have also been reported in depression [19,20,21,22,23]. Thus, based on the current stage of research, it remains unclear how exactly perturbation of the glutamatergic system and depression are linked. A more detailed understanding of this relationship would be helpful to pin down the antidepressant mechanisms of rapid-acting glutamatergic antidepressants such as ketamine. Furthermore, baseline metabolite levels in depressed patients could be established as an indicator of treatment response to medication targeting glutamatergic receptors [24].
Several lines of investigation have shown that ketamine increases prefrontal Glu levels through NMDA receptor inhibition and subsequent AMPA receptor activation [25,26,27]. Interestingly, the pregenual anterior cingulate cortex (pgACC) has been found to exhibit above average AMPA receptors and below average NMDA receptor densities (compared with whole cingulate cortex) [28] and regional variations of Glu and Gln concentrations have been shown to follow these receptor fingerprints [29]. Abdallah et al. [30] reported that ketamine increases prefrontal glutamate–glutamine cycling, thereby providing the most direct evidence in humans that ketamine increases glutamate release in the prefrontal cortex. Changes in the pgACC occur within the first 30 min after the start of the ketamine infusion, which supports the idea that the Glu burst happens quite early [31]. Accordingly, several 1H-MRS investigations noted increased glutamatergic metabolite levels in healthy volunteers [25, 26] and increased Glx levels in depressed subjects [31] during acute ketamine administration; the ratio of Gln to Glu was also found to be increased 24 h after acute ketamine administration in healthy volunteers [32]. Nevertheless, other investigations found no significant changes in Glu measurements 1 h post-ketamine infusion in healthy volunteers [33], or three and 48 h later in depressed subjects [34]; variations in voxel location, timing of the scan, imaging parameters, and sample size may explain these discrepant findings. Evans et al. [35] reported that ketamine did not affect Glu or Gln levels in the pgACC in depressed subjects 24 h post-ketamine infusion and that antidepressant response was not predicted by baseline levels. On the other hand, there are reports of a prediction of treatment response by baseline levels of glutamatergic metabolites as well as of an association between lower Glx response to acute ketamine administration and antidepressant response [36, 37].
As of today, a relatively large number of imaging studies have investigated the effects of ketamine in the human brain [5]. Although results do not converge into a clear pattern of effects yet, several findings have been replicated in independent studies. The anterior cingulate cortex (ACC), and especially the pre- and subgenual subdivisions, have been repeatedly implicated in the effects of ketamine [6]. The pregenual ACC (pgACC) plays an important role in emotional processing and establishing mood states [38, 39], and abnormal pgACC activity has been implicated in depressive pathology [40, 41]. Furthermore, ketamine-induced changes in functional connectivity between the right lateral PFC and the sgACC have been linked to the reduction of depressive symptoms [42], which could indicate restored prefrontal cognitive control over emotional processing. Thus, it is likely that ketamine-induced alterations in pgACC and sgACC activity are linked to relief of depressive symptoms. However, despite the extensive study of ketamine using brain imaging in healthy and depressed human subjects, the exact antidepressant mechanism of ketamine remains unclear. Investigating the relationship between ketamine induced metabolic and functional brain changes via multimodal brain imaging is a promising approach to advance our understanding of how ketamine exerts its rapid antidepressant effects.
To the best of our knowledge, the link between ketamine-induced alterations in glutamatergic signaling, and altered functional activation, and connectivity has only been investigated in two previous studies. One of these, however, focused on changes 1 h and 24 h after ketamine administration [43] and reported that altered Gln/Glu concentration 24 h after ketamine was associated with increased functional connectivity within the default mode network (DMN). The study by Kraguljac et al. [44] reported neurometabolite levels and functional connectivity during ketamine infusion, however, focused on the hippocampus which is not part of the neural circuitry of depression and furthermore did not distinguish between Glu and Gln.
Based on prior work demonstrating that changes in glutamatergic neurotransmission in pgACC, a region implicated both in the effects of ketamine and in emotional processing, occur early after the start of the ketamine infusion, our study aimed to investigate acute effects of ketamine on pgACC spontaneous activity, functional connectivity, and Gln/Glu metabolite concentration using a multimodal imaging approach.
Methods
Participants
The study was performed at the University of Zurich by the Department for Psychiatry, Psychotherapy and Psychosomatics (Psychiatry University Hospital Zurich) and the Institute for Biomedical Engineering (ETH Zürich). Twenty-three healthy subjects (n = 23, mean age, 25.5; 12 males) participated in the MRI study. Resting state fMRI data were available for the entire sample (N = 23). Complete MRS data were available for a sub-sample of N = 16 participants. MRS data of five subjects had to be excluded because of an error in the MRS sequence. Additionally, MRS data of two subjects could not be analyzed because of a missing high-resolution 3D T1 weighted sequence, which was needed for tissue signal correction. All subjects underwent a medical examination and psychiatric interview based on the Brief Psychiatric Rating Scale (BPRS; [45]) and the Hamilton Rating Scale for Depression (HAMD; [46]). Only medication-free subjects that were healthy according to the physical examination, electrocardiogram, and blood and urine analyses were included in the study. Exclusion criteria were a history of psychiatric/neurological diseases, drug abuse, concurrent medication, cardiovascular disease, anemia, thyroid disease, any somatic disease affecting drug metabolism and excretion (e.g., renal or liver disease), MR exclusion criteria, pregnancy and left-handedness.
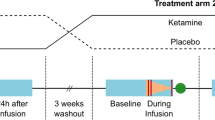
Study design
Subjects completed two separate MRI sessions on a Philips Achieva 3T whole-body MR unit. The first session served as physiological baseline and subjects were not infused with any (pharmacological) agent. In the second session, S-ketamine (Ketanest, Pfizer, Zurich, Switzerland) was administered as an intravenous bolus of 0.12 mg/kg approximately 25 min prior to the MRI, followed by a continuous infusion of 0.25 mg/kg/h during the entire MR scanning period. During the acquisition of resting state, subjects were told to lie still in the scanner with their eyes closed. The functional images were collected in 10 min runs (200 volumes). The interval between the two sessions was 3 days on average.
Data acquisition and analyses
Resting state fMRI
The functional images were acquired with a sensitivity-encoded single-shot echo-planar imaging sequence (SENSE-sshEPI) [47] in 10 min runs (200 vol). Following acquisition parameters were used: TE = 35 ms; field of view (FOV) = 22 cm, acquisition matrix = 80 × 80 interpolated to 128 × 128, TR 3000 ms, flip angle 82°, voxel size = 2.75 × 2.75 × 4 mm, 32 contiguous axial slices (placed along the anterior–posterior commissure plane) and sensitivity-encoded acceleration factor R = 2.0).
Three-dimensional T1-weighted anatomical scans were obtained for structural reference for both, placebo and ketamine conditions individually (T1 3D FFE sequence: TR/TE = 9.3/4.6 ms, flip angle = 8°, 160 sagittal slices, FOV 240 × 240 mm, voxel size 1 × 1 × 1 mm).
Resting state fMRI data were analyzed in MATLAB (VersionR2018b) using SPM12 and the CONN toolbox (Version 20b; [48]). Preprocessing of fMRI data included removal of the first five scans, motion correction (realignment and unwarping), slice-timing correction, automatic detection of artifactual scans (ART-based scrubbing; 97th percentile), normalization to MNI space (structural target resolution: 1 mm, function target resolution: 2 mm), and spatial smoothing (8 mm). During the denoising step in CONN single-subject linear regression analyses were performed to remove the effects of head motion (12 total motion covariates: 6 motion parameters plus temporal derivatives), physiological artifacts (10 total CompCor eigenvariates: 5 each from eroded WM and CSF masks), and artifactual scans. The resulting residual BOLD time series were band-pass filtered (0.01–0.1 Hz). Spontaneous neural activity was calculated using fractional amplitude of low frequency fluctuations (fALFF) as implemented in the CONN toolbox [49]. The pgACC ROI used for the functional imaging analysis was created based on previous publications (MNI coordinates: 0, 42, 2; diameter: 10 mm; [50, 51]).
MRS
The high-resolution 3D T1 was used to plan the MRS acquisition and calculate the tissue composition of the voxel. Spectra were acquired with a maximum echo-sampled J-resolved PRESS sequence (JPRESS; [52]) including second-order B0 shimming with VAPOR water suppression [53] and outer volume suppression (OVS) and inner volume saturation (IVS) [54, 55]. The voxel size was 25 × 18 × 20 mm3 (AP × LR × FH). JPRESS was implemented as two-dimensional echo time series with a minimum echo time (TE) of 30 ms and repetition time (TR) of 1600 ms. 100 echo steps (step size = 2 ms) with 8 water suppressed signal averages (NSA) per echo step and non-water suppressed reference were acquired covering the range from 30 to 228 ms with a total number of signal averages of 800 (acquisition time: 24 min). The 2D technique allows disentangling of the signals of overlaying metabolite resonances by encoding the chemical shift information in the first dimension and the J-coupling information in the second dimension. Therefore, the signals of usually overlapping (in 1D) metabolites such as Glutamine (Gln) and Glutamate (Glu) can be identified independently.
The MRS data were analyzed with ProFit2 (Prior-knowledge Fitting) including 18 metabolites [56]. The basis set consisted of 18 metabolites including Glu, Gln and GABA. A chemical shift range was covered in the first dimension from 0.5 to 4 ppm and in the second dimension from − 0.4 to 0.4. Processing steps included a Hankel singular value decomposition (HSVD) water filter, eddy current, and zero- and first-phase correction. Artefact inspection for bad water suppression, line shape distortion or ghosting was conducted visually. The amount of water signal measured in the non-water suppressed reference acquisition was used as internal reference. In addition, with a custom-written MATLAB script tissue composition correction (CSF, WM, GM) was conducted to report metabolite concentration values with respect to internal water [57]. Results from the MRS analysis for one representative subject are shown in Fig. 1.
MRS analyses. A Representative spectroscopy voxel placement in the pregenual anterior cingulate cortex (sagittal view). B Representative one-dimensional projections of the 2D JPRESS data: The measured data (blue), the fitted spectrum (red) and the baseline (orange) are shown for the first (left rows; (i)] and second timepoint (right rows, (iv)]. In addition, the individual signal contribution envelope of Glutamate (ii) and (v) and Glutamine (iii) and (vi) is shown at the first and second time point. C Representative two-dimensional JPRESS data: The acquired spectrum (i), the fitted spectrum (ii) and the fit error (residuum, iii) are shown including the signal contributions of glutamate (iv) and glutamine (v). The common and distinct frequency pattern is shown to help disentangle the signal from Glu and Gln
Statistical analysis
For the whole-brain fMRI analyses the results were considered significant at the voxel-level p < 0.001, at the whole-brain level, cluster-corrected at p-FDR < 0.05. For some exploratory analysis and visualization purposes, we used a voxel threshold of p < 0.05. This liberal voxel threshold was penalized with a strict cluster correction level of p-FDR < 0.001. Correlations between imaging modalities were calculated using Pearson’s correlation coefficient (alpha level = 0.05). For each modality, combination results were FDR corrected. However, uncorrected results are reported as well, and marked as such.
Results
Spontaneous brain activation
The whole-brain analysis of spontaneous brain activation revealed stronger activation of the left anterior insula, and deactivation in the right lingual gyrus and the right occipital pole under ketamine (Fig. 2A, Table 1). The exploratory analysis revealed a clear picture of activation in multiple prefrontal brain regions, and deactivation in multiple posterior brain regions (Fig. 2B). The ROI analysis in the pgACC revealed no significant change between baseline activations and activations during the ketamine infusion (t(22) = − 1.38, p = 0.18). On the descriptive level, pgACC activations were increased during ketamine (M = 0.13, SD = 0.51) compared to baseline (M = − 0.05, SD = 0.51).
Resting state functional connectivity
The analysis of resting state functional connectivity (rsFC) changes during ketamine revealed increased rsFC from the pgACC seed to the right frontal pole, and decreased rsFC to the anterior mid cingulate cortex (aMCC), the left superior frontal gyrus, and the left superior parietal lobe, (Fig. 3, Table 2).
Altered resting state functional connectivity during ketamine of the pgACC seed region. Increased activation is shown in red color, decreased activation is shown in blue color. A Activation changes with standard settings for cluster-based inference. B Activation changes with exploratory settings for cluster-based inference
Metabolite concentration
The analysis of glutamate signaling in the pgACC revealed no significant changes for Glu, Gln, and the Gln/Glu ratio. However, a trend towards increased Glu concentration during ketamine was observed. On the descriptive level, metabolite concentrations were increased for Glu and decreased for Gln and the Gln/Glu ratio (Table 3).
Activity changes in pgACC linked to altered metabolite concentration
Correlation analyses (Pearson’s correlation coefficient) between pgACC activity changes and changes in metabolite concentration showed a significant association for Gln (r = − 0.54, p = 0.033) and the Gln/Glu ratio (r = − 0.59, p = 0.017). Increased activity in the pgACC during ketamine was linked to lower Gln concentration in the pgACC and to a lower Gln/Glu ratio (Fig. 4). No significant relationship was observed for Glu (r = 0.17, p = 0.52).
FC changes of the pgACC linked to altered metabolite concentration
Exploratory correlation analyses were carried out with the four clusters that showed rsFC changes to the pgACC seed region (cp. Table 2). It was tested whether these rsFC changes were linked to changes in pgACC activity, or changes in metabolite concentration. A relationship was observed between pgACC activation and reduced rsFC to the aMCC (r = − 0.45, p = 0.032, Fig. 5A). Furthermore, a marginally significant relationship was observed between Gln levels and pgACC-aMCC connectivity (r = 0.48, p = 0.062, Fig. 5B).
Discussion
In this multimodal imaging study, we investigated acute effects of ketamine on spontaneous brain activation, functional connectivity, and metabolism in the glutamatergic system. In particular, we investigated how changes in the individual imaging modalities were interrelated to gain a better understanding of how molecular and macroscopic brain changes induced by ketamine are linked. We focused our analysis on the pregenual anterior cingulate cortex (pgACC) because ketamine-induced brain changes have been repeatedly reported in this region, and the specific receptor profile of this region suggests that the antidepressant mechanism of ketamine might be linked to metabolic changes in this region.
ROI analysis in the pgACC showed no significant change between baseline activation and activation during the ketamine infusion. While previous reports are rather consistent regarding decreased activation in the sgACC during a ketamine infusion [58,59,60], evidence for pgACC is less clear [6]. Downey et al. [61] found increased activation during ketamine in a region at the border between the pgACC and the sgACC, and Javitt et al. [62] found widespread frontal activation that included the pgACC during ketamine. These findings suggest that ketamine-induced activity changes in the pgACC and sgACC could point into opposite directions. Further, regarding spontaneous brain activations during ketamine, the whole-brain analysis conducted in our study showed increases in the left anterior insula and decreases in occipital regions. Ketamine-induced activation of the insula has also been previously reported in healthy subjects [60, 63]. The insula is a central node of the salience network (SN) and thought to mediate interpretation of sensory information that contributes to emotional states [64]. Furthermore, strong connectivity to nodes of the anterior DMN underlines the insula’s hypothesized role in switching between the DMN and executive control network (ECN; [65, 66]). Thus, increased activation of the insula during ketamine might be linked to switching from DMN to activation of other networks. This is line with previous findings suggesting that the antidepressant effects of ketamine are linked to reduced activity in brain networks related to self-referential processing [5]. Interestingly, a noticeably clear pattern of frontal activation, and posterior deactivation was observed when a more liberal statistical voxel threshold was applied. Strong frontal activation patterns induced by ketamine correspond to “hyperfrontality” reported in several previous studies and might be related to altered interpretation of visual and spatial information about the external and internal reality [67,68,69,70].
Stronger functional connectivity (FC) during ketamine was observed between the pgACC and the right frontal pole. FC between the right frontal pole and the subgenual ACC has previously been linked to the antidepressant effects of ketamine 24 h after the infusion [42] and might reflect the restoration of cognitive control over aberrant emotion processing in limbic structures [5, 71]. Decreased FC was observed between the pgACC and the anterior mid cingulate cortex (aMCC), a region implicated in cognitive aspects of motor control [72], and the experience of negative affect and pain [73]. As the pgACC is involved in the subjective experience of affect [6], its decoupling from the aMCC might be linked to altered processing of emotion. The decoupling from a region involved in motor control might also be linked to the feeling of disembodiment, which is a core feature of the subjective experience during a ketamine infusion [74].
No absolute changes in metabolic Glu, Gln, and Gln/Glu concentrations were observed, but there was a trend towards Glu increases during ketamine and descriptively Gln and Gln/Glu were reduced during ketamine. The lack of significance could be due to the rather small sample size in our study, but it should be noted that on the descriptive level the results regarding Glu are consistent with previous findings and support the idea that changes in glutamatergic neurotransmission happen quite early after the start of the ketamine infusion [31, 60]. Increased Glu concentration after ketamine has been linked to NMDA receptor inhibition and subsequent AMPA receptor activation [25,26,27]. Since the pgACC exhibits above average AMPA and below average NMDA receptor densities [28], the Glu response to a single subanesthetic dose of ketamine may be associated with the histoarchitectonical receptor fingerprint of this brain region.
Regarding cross-modality associations, our results showed that increased pgACC activation was linked to lower Gln concentration and a lower Gln/Glu ratio in the pgACC. Gln is seen as the non-neuroactive precursor and metabolite in the glutamate–glutamine cycle, enabling the right amount of physiological Glu neuron firing [75]. Some studies in depressed subjects reported increased Gln levels [11, 30, 76, 77] as well as lower baseline Gln predicting better clinical outcome [78]. Along that line, a recent study by Milak et al. [36] demonstrated that the lower the Glx response to ketamine, the better the antidepressant response. Activity in pgACC during emotional and cognitive tasks not only predicts antidepressant response to ketamine [79, 80], but the pgACC is currently the best supported candidate for a general neuroimaging biomarker for antidepressant response [81]. It has been proposed that an increased activity state of the pgACC may represent its treatment-responsive mode and be specifically important for clinical effects of rapid-acting glutamatergic drugs such as ketamine [61, 81, 82]. Therefore, our findings might indicate that acute ketamine administration increases pgACC activity, which would correspond to a treatment-responsive mode in depressed subjects. This might be accompanied by a surge of Glu, but initially lower Glu conversion in glial cells, resulting in a decreased Gln concentration as well as a lower Gln/Glu ratio [16]. Though speculative, in depressed patients, these changes might then eventually trigger the antidepressant effects of ketamine that occur within the first hours after a single dose of ketamine. Findings by Li et al. [32] indicate a reversal of this pattern 24 h after ketamine, i.e., an increased Gln/ Glu ratio in the pgACC, which might reflect secondary effects. To our knowledge, this is the first study reporting linkage between ketamine-induced changes in glutamatergic metabolites and spontaneous activation in the same region. While Li et al. [43] reported an association of glutamatergic metabolites and FC within the DMN as well as between FC and spontaneous brain activation at 1 h and 24 h after ketamine, they did not investigate the acute stage and did not report on all cross-modality associations.
Several other studies have reported positive associations, BOLD responses and glutamatergic metabolite concentrations [83, 84]; however, a recent systematic review reports no coherent relationship between glutamate and BOLD activation [83]. One possible reason for this could be that the majority of studies did not separate Glu and Gln due to methodological difficulties, but rather report the two compounds together as Glx. Our finding points out the importance of detailed investigations of both compounds to better understand the effects of ketamine on the glutamatergic system, since Glx measurement might obscure important findings that are linked to only one of the metabolites.
Our results also suggest that lower Gln concentration and stronger spontaneous activation of the pgACC during ketamine might be associated with reduced functional connectivity to the aMCC. While the FC result has been discussed above, this result suggests that both altered activation and metabolism are also linked to this change in FC. It is intriguing to speculate about the directionality of the relationships in this triangle, however, due to the purely correlative nature of this analysis such inferences cannot be made. It could be hypothesized that altered glutamatergic signaling in the pgACC brings forward changes in functional activations, and connectivity (and not the other way around). To investigate this hypothesis, upcoming studies could include a condition in which glutamatergic signaling is blocked by another compound such as Lamotrigine.
The main limitation of this study is the rather small sample size, and the results reported here must be replicated in larger cohorts. However, the reported effect sizes in the correlation analyses suggest meaningful results, and the scatterplots show that effects are not driven by outliers. Furthermore, to shed some more light on ketamine’s effect on glutamatergic neurotransmission, future studies should not only include a control group, but also an experimental group where Glu signaling is inhibited.
In conclusion, our results demonstrate how multimodal investigations in a single brain region could help to advance our understanding of how metabolic changes in the glutamatergic system are linked to changes in functional activations and connectivity.
References
Coyle CM, Laws KR (2015) The use of ketamine as an antidepressant: a systematic review and meta-analysis. Hum Psychopharmacol Clin Exp 30:152–163
Conley AA, Norwood AEQ, Hatvany TC, Griffith JD, Barber KE (2021) Efficacy of ketamine for major depressive episodes at 2, 4, and 6-weeks post-treatment: a meta-analysis. Psychopharmacology 238:1737–1752
Krystal JH, Sanacora G, Duman RS (2013) Rapid-acting glutamatergic antidepressants: the path to ketamine and beyond. Biol Psychiatry 73:1133–1141
Li N, Lee B, Liu R-J, Banasr M, Dwyer JM, Iwata M et al (2010) mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. Science 329:959–964
Ionescu DF, Felicione JM, Gosai A, Cusin C, Shin P, Shapero BG et al (2018) Ketamine-associated brain changes: a review of the neuroimaging literature. Harv Rev Psychiatry 26:320–339
Alexander L, Jelen LA, Mehta MA, Young AH (2021) The anterior cingulate cortex as a key locus of ketamine’s antidepressant action. Neurosci Biobehav Rev 127:531–554
Abdallah CG, Averill LA, Krystal JH (2015) Ketamine as a promising prototype for a new generation of rapid-acting antidepressants. Ann N Y Acad Sci 1344:66–77
Lener MS, Niciu MJ, Ballard ED, Park M, Park LT, Nugent AC et al (2017) Glutamate and gamma-aminobutyric acid systems in the pathophysiology of major depression and antidepressant response to ketamine. Biol Psychiatry 81:886–897
Sanacora G, Treccani G, Popoli M (2012) Towards a glutamate hypothesis of depression. Neuropharmacology 62:63–77
Rothman DL, De Feyter HM, Graaf RA, Mason GF, Behar KL (2011) 13C MRS studies of neuroenergetics and neurotransmitter cycling in humans. NMR Biomed 24:943–957
Godlewska BR, Masaki C, Sharpley AL, Cowen PJ, Emir UE (2018) Brain glutamate in medication-free depressed patients: a proton MRS study at 7 Tesla. Psychol Med 48:1731–1737
Rajkowska G, Stockmeier CA (2013) Astrocyte pathology in major depressive disorder: insights from human postmortem brain tissue. Curr Drug Targets 14:1225–1236
Arnone D, Mumuni AN, Jauhar S, Condon B, Cavanagh J (2015) Indirect evidence of selective glial involvement in glutamate-based mechanisms of mood regulation in depression: meta-analysis of absolute prefrontal neuro-metabolic concentrations. Eur Neuropsychopharmacol 25:1109–1117
Benson KL, Bottary R, Schoerning L, Baer L, Gonenc A, Eric Jensen J et al (2020) 1H MRS measurement of cortical GABA and glutamate in primary insomnia and major depressive disorder: relationship to sleep quality and depression severity. J Affect Disord 274:624–631
Luykx JJ, Laban KG, van den Heuvel MP, Boks MPM, Mandl RCW, Kahn RS et al (2012) Region and state specific glutamate downregulation in major depressive disorder: a meta-analysis of 1H-MRS findings. Neurosci Biobehav Rev 36:198–205
Shirayama Y, Takahashi M, Osone F, Hara A, Okubo T (2017) Myo-inositol, glutamate, and glutamine in the prefrontal cortex, hippocampus, and amygdala in major depression. Biol Psychiatry Cogn Neurosci Neuroimaging 2:196–204
Walter M, Henning A, Grimm S, Schulte RF, Beck J, Dydak U et al (2009) The relationship between aberrant neuronal activation in the pregenual anterior cingulate, altered glutamatergic metabolism, and anhedonia in major depression. Arch Gen Psychiatry 66:478
Wise T, Taylor MJ, Herane-Vives A, Gammazza AM, Cappello F, Lythgoe DJ et al (2018) Glutamatergic hypofunction in medication-free major depression: secondary effects of affective diagnosis and relationship to peripheral glutaminase. J Affect Disord 234:214–219
Bond DJ, Lim KO (2014) C13 magnetic resonance spectroscopy and glutamate metabolism in mood disorders: current challenges, potential opportunities. Am J Psychiatry 171:1240–1242
Godfrey KEM, Gardner AC, Kwon S, Chea W, Muthukumaraswamy SD (2018) Differences in excitatory and inhibitory neurotransmitter levels between depressed patients and healthy controls: a systematic review and meta-analysis. J Psychiatr Res 105:33–44
Li M, Metzger CD, Li W, Safron A, van Tol M-J, Lord A et al (2014) Dissociation of glutamate and cortical thickness is restricted to regions subserving trait but not state markers in major depressive disorder. J Affect Disord 169:91–100
Moriguchi S, Takamiya A, Noda Y, Horita N, Wada M, Tsugawa S et al (2019) Glutamatergic neurometabolite levels in major depressive disorder: a systematic review and meta-analysis of proton magnetic resonance spectroscopy studies. Mol Psychiatry 24:952–964
Yüksel C, Öngür D (2010) Magnetic resonance spectroscopy studies of glutamate-related abnormalities in mood disorders. Biol Psychiatry 68:785–794
Murrough JW, Abdallah CG, Mathew SJ (2017) Targeting glutamate signalling in depression: progress and prospects. Nat Rev Drug Discov 16:472–486
Rowland LM, Bustillo JR, Mullins PG, Jung RE, Lenroot R, Landgraf E et al (2005) Effects of ketamine on anterior cingulate glutamate metabolism in healthy humans: a 4-T proton MRS study. Am J Psychiatry 162:394–396
Stone JM, Dietrich C, Edden R, Mehta MA, De Simoni S, Reed LJ et al (2012) Ketamine effects on brain GABA and glutamate levels with 1H-MRS: relationship to ketamine-induced psychopathology. Mol Psychiatry 17:664–665
Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI et al (2016) NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Nature 533:481–486
Palomero-Gallagher N, Vogt BA, Schleicher A, Mayberg HS, Zilles K (2009) Receptor architecture of human cingulate cortex: evaluation of the four-region neurobiological model. Hum Brain Mapp 30:2336–2355
Dou W, Palomero-Gallagher N, van Tol M-J, Kaufmann J, Zhong K, Bernstein H-G et al (2013) Systematic regional variations of GABA, glutamine, and glutamate concentrations follow receptor fingerprints of human cingulate cortex. J Neurosci 33:12698–12704
Abdallah CG, De Feyter HM, Averill LA, Jiang L, Averill CL, Chowdhury GMI et al (2018) The effects of ketamine on prefrontal glutamate neurotransmission in healthy and depressed subjects. Neuropsychopharmacology 43:2154–2160
Milak MS, Proper CJ, Mulhern ST, Parter AL, Kegeles LS, Ogden RT et al (2016) A pilot in vivo proton magnetic resonance spectroscopy study of amino acid neurotransmitter response to ketamine treatment of major depressive disorder. Mol Psychiatry 21:320–327
Li M, Demenescu LR, Colic L, Metzger CD, Heinze H-J, Steiner J et al (2017) Temporal dynamics of antidepressant ketamine effects on glutamine cycling follow regional fingerprints of AMPA and NMDA receptor densities. Neuropsychopharmacology 42:1201–1209
Taylor MJ, Tiangga ER, Mhuircheartaigh RN, Cowen PJ (2012) Lack of effect of ketamine on cortical glutamate and glutamine in healthy volunteers: a proton magnetic resonance spectroscopy study. J Psychopharmacol (Oxf) 26:733–737
Valentine GW, Mason GF, Gomez R, Fasula M, Watzl J, Pittman B et al (2011) The antidepressant effect of ketamine is not associated with changes in occipital amino acid neurotransmitter content as measured by [1H]-MRS. Psychiatry Res Neuroimaging 191:122–127
Evans JW, Lally N, An L, Li N, Nugent AC, Banerjee D et al (2018) 7T 1H-MRS in major depressive disorder: a Ketamine Treatment Study. Neuropsychopharmacology 43:1908–1914
Milak MS, Rashid R, Dong Z, Kegeles LS, Grunebaum MF, Ogden RT et al (2020) Assessment of relationship of ketamine dose with magnetic resonance spectroscopy of Glx and GABA responses in adults with major depression: a randomized clinical trial. JAMA Netw Open 3:e2013211
Salvadore G, van der Veen JW, Zhang Y, Marenco S, Machado-Vieira R, Baumann J et al (2012) An investigation of amino-acid neurotransmitters as potential predictors of clinical improvement to ketamine in depression. Int J Neuropsychopharmacol 15:1063–1072
Drevets WC, Savitz J, Trimble M (2008) The subgenual anterior cingulate cortex in mood disorders. CNS Spectr 13:663–681
Pizzagalli DA (2011) Frontocingulate dysfunction in depression: toward biomarkers of treatment response. Neuropsychopharmacology 36:183–206
Godlewska BR, Browning M, Norbury R, Igoumenou A, Cowen PJ, Harmer CJ (2018) Predicting treatment response in depression: the role of anterior cingulate cortex. Int J Neuropsychopharmacol 21:988–996
Pizzagalli DA, Webb CA, Dillon DG, Tenke CE, Kayser J, Goer F et al (2018) Pretreatment rostral anterior cingulate cortex theta activity in relation to symptom improvement in depression: a randomized clinical trial. JAMA Psychiat 75:547–554
Gärtner M, Aust S, Bajbouj M, Fan Y, Wingenfeld K, Otte C et al (2019) Functional connectivity between prefrontal cortex and subgenual cingulate predicts antidepressant effects of ketamine. Eur Neuropsychopharmacol 29:501–508
Li M, Woelfer M, Colic L, Safron A, Chang C, Heinze H-J et al (2020) Default mode network connectivity change corresponds to ketamine’s delayed glutamatergic effects. Eur Arch Psychiatry Clin Neurosci 270:207–216
Kraguljac NV, Frölich MA, Tran S, White DM, Nichols N, Barton-McArdle A et al (2017) Ketamine modulates hippocampal neurochemistry and functional connectivity: a combined magnetic resonance spectroscopy and resting-state fMRI study in healthy volunteers. Mol Psychiatry 22:562–569
Rhoades HM, Overall JE (1988) The semistructured BPRS interview and rating guide. Psychopharmacol Bull 24:101–104
Hamilton M (1980) Rating depressive patients. J Clin Psychiatry 41:21–24
Schmidt CF, Degonda N, Luechinger R, Henke K, Boesiger P (2005) Sensitivity-encoded (SENSE) echo planar fMRI at 3T in the medial temporal lobe. Neuroimage 25:625–641
Whitfield-Gabrieli S, Nieto-Castanon A (2012) Conn: a functional connectivity toolbox for correlated and anticorrelated brain networks. Brain Connect 2:125–141
Zou Q-H, Zhu C-Z, Yang Y, Zuo X-N, Long X-Y, Cao Q-J et al (2008) An improved approach to detection of amplitude of low-frequency fluctuation (ALFF) for resting-state fMRI: fractional ALFF. J Neurosci Methods 172:137–141
Grimm S, Ernst J, Boesiger P, Schuepbach D, Boeker H, Northoff G (2011) Reduced negative BOLD responses in the default-mode network and increased self-focus in depression. World J Biol Psychiatry 12:627–637
Hartling C, Metz S, Pehrs C, Scheidegger M, Gruzman R, Keicher C et al (2021) Comparison of four fMRI paradigms probing emotion processing. Brain Sci 11:525
Schulte RF, Lange T, Beck J, Meier D, Boesiger P (2006) Improved two-dimensional J-resolved spectroscopy. NMR Biomed 19:264–270
Hock A, Fuchs A, Boesiger P, Kollias SS, Henning A (2013) Electrocardiogram-triggered, higher order, projection-based B0 shimming allows for fast and reproducible shim convergence in spinal cord 1H MRS. NMR Biomed 26:329–335
Edden RAE, Barker PB (2007) Spatial effects in the detection of γ-aminobutyric acid: improved sensitivity at high fields using inner volume saturation. Magn Reson Med 58:1276–1282
Henning A, Schär M, Kollias SS, Boesiger P, Dydak U (2008) Quantitative magnetic resonance spectroscopy in the entire human cervical spinal cord and beyond at 3T. Magn Reson Med 59:1250–1258
Fuchs A, Boesiger P, Schulte RF, Henning A (2014) ProFit revisited. Magn Reson Med 71:458–468
Gasparovic C, Song T, Devier D, Bockholt HJ, Caprihan A, Mullins PG et al (2006) Use of tissue water as a concentration reference for proton spectroscopic imaging. Magn Reson Med 55:1219–1226
Deakin JFW, Lees J, McKie S, Hallak JEC, Williams SR, Dursun SM (2008) Glutamate and the neural basis of the subjective effects of ketamine: a pharmaco-magnetic resonance imaging study. Arch Gen Psychiatry 65:154
Doyle OM, De Simoni S, Schwarz AJ, Brittain C, O’Daly OG, Williams SCR et al (2013) Quantifying the attenuation of the ketamine pharmacological magnetic resonance imaging response in humans: a validation using antipsychotic and glutamatergic agents. J Pharmacol Exp Ther 345:151–160
Stone JM, Kotoula V, Dietrich C, De Simoni S, Krystal JH, Mehta MA (2015) Perceptual distortions and delusional thinking following ketamine administration are related to increased pharmacological MRI signal changes in the parietal lobe. J Psychopharmacol (Oxf) 29:1025–1028
Downey D, Dutta A, McKie S, Dawson GR, Dourish CT, Craig K et al (2016) Comparing the actions of lanicemine and ketamine in depression: key role of the anterior cingulate. Eur Neuropsychopharmacol 26:994–1003
Javitt DC, Carter CS, Krystal JH, Kantrowitz JT, Girgis RR, Kegeles LS et al (2018) Utility of imaging-based biomarkers for glutamate-targeted drug development in psychotic disorders: a randomized clinical trial. JAMA Psychiat 75:11–19
Höflich A, Hahn A, Küblböck M, Kranz GS, Vanicek T, Windischberger C et al (2015) Ketamine-induced modulation of the thalamo-cortical network in healthy volunteers as a model for schizophrenia. Int J Neuropsychopharmacol 18:pyv040
Craig A (2003) Interoception: the sense of the physiological condition of the body. Curr Opin Neurobiol 13:500–505
Goulden N, Khusnulina A, Davis NJ, Bracewell RM, Bokde AL, McNulty JP et al (2014) The salience network is responsible for switching between the default mode network and the central executive network: replication from DCM. Neuroimage 99:180–190
Sridharan D, Levitin DJ, Menon V (2008) A critical role for the right fronto-insular cortex in switching between central-executive and default-mode networks. Proc Natl Acad Sci 105:12569–12574
Dawson N, Morris BJ, Pratt JA (2013) Subanaesthetic ketamine treatment alters prefrontal cortex connectivity with thalamus and ascending subcortical systems. Schizophr Bull 39:366–377
Holcomb HH, Lahti AC, Medoff DR, Cullen T, Tamminga CA (2005) Effects of noncompetitive NMDA receptor blockade on anterior cingulate cerebral blood flow in volunteers with schizophrenia. Neuropsychopharmacology 30:2275–2282
Lahti AC, Weiler MA, Medoff DR, Tamminga CA, Holcomb HH (2005) Functional effects of single dose first- and second-generation antipsychotic administration in subjects with schizophrenia. Psychiatry Res Neuroimaging 139:19–30
Vollenweider FX, Leenders KL, Øye I, Hell D, Angst J (1997) Differential psychopathology and patterns of cerebral glucose utilisation produced by (S)- and (R)-ketamine in healthy volunteers using positron emission tomography (PET). Eur Neuropsychopharmacol 7:25–38
Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C et al (2005) Deep brain stimulation for treatment-resistant depression. Neuron 45:651–660
Hoffstaedter F, Grefkes C, Caspers S, Roski C, Palomero-Gallagher N, Laird AR et al (2014) The role of anterior midcingulate cortex in cognitive motor control: evidence from functional connectivity analyses. Hum Brain Mapp 35:2741–2753
Tolomeo S, Christmas D, Jentzsch I, Johnston B, Sprengelmeyer R, Matthews K et al (2016) A causal role for the anterior mid-cingulate cortex in negative affect and cognitive control. Brain 139:1844–1854
Vlisides PE, Bel-Bahar T, Nelson A, Chilton K, Smith E, Janke E et al (2018) Subanaesthetic ketamine and altered states of consciousness in humans. Br J Anaesth 121:249–259
Gras G, Porcheray F, Samah B, Leone C (2006) The glutamate-glutamine cycle as an inducible, protective face of macrophage activation. J Leukoc Biol 80:1067–1075
Hasler G, Buchmann A, Haynes M, Müller ST, Ghisleni C, Brechbühl S et al (2019) Association between prefrontal glutamine levels and neuroticism determined using proton magnetic resonance spectroscopy. Transl Psychiatry 9:170
Jollant F, Near J, Turecki G, Richard-Devantoy S (2017) Spectroscopy markers of suicidal risk and mental pain in depressed patients. Prog Neuropsychopharmacol Biol Psychiatry 73:64–71
Clark DL, MacMaster FP, Brown EC, Kiss ZHT, Ramasubbu R (2020) Rostral anterior cingulate glutamate predicts response to subcallosal deep brain stimulation for resistant depression. J Affect Disord 266:90–94
Salvadore G, Cornwell BR, Colon-Rosario V, Coppola R, Grillon C, Zarate CA et al (2009) Increased anterior cingulate cortical activity in response to fearful faces: a neurophysiological biomarker that predicts rapid antidepressant response to ketamine. Biol Psychiatry 65:289–295
Salvadore G, Cornwell BR, Sambataro F, Latov D, Colon-Rosario V, Carver F et al (2010) Anterior cingulate desynchronization and functional connectivity with the amygdala during a working memory task predict rapid antidepressant response to ketamine. Neuropsychopharmacology 35:1415–1422
Godlewska BR (2020) Neuroimaging as a tool for individualized treatment choice in depression: the past, the present and the future. Curr Behav Neurosci Rep 7:32–39
Abdallah CG, Adams TG, Kelmendi B, Esterlis I, Sanacora G, Krystal JH (2016) Ketamine’s mechanism of action: a path to rapid-acting antidepressants. Depress Anxiety 33:689–697
Kiemes A, Davies C, Kempton MJ, Lukow PB, Bennallick C, Stone JM et al (2021) GABA, glutamate and neural activity: a systematic review with meta-analysis of multimodal 1H-MRS-fMRI studies. Front Psychiatry. 12:644315
Vijayakumari AA, Thomas B, Menon RN, Kesavadas C (2018) Association between glutamate/glutamine and blood oxygen level dependent signal in the left dorsolateral prefrontal region during verbal working memory. NeuroReport 29:478–482
Acknowledgements
This work was funded by the European Commission (Grant number H2020–634541) and by Boehringer Ingelheim Pharma GmbH & Co. KG. The authors wish to thank Luisa Bönke, Marvin Sören Meiering and David Weigner for their support in the bibliography update. Simone Grimm has served as a consultant to and received research support from Boehringer Ingelheim Pharma.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gärtner, M., Weigand, A., Scheidegger, M. et al. Acute effects of ketamine on the pregenual anterior cingulate: linking spontaneous activation, functional connectivity, and glutamate metabolism. Eur Arch Psychiatry Clin Neurosci 272, 703–714 (2022). https://doi.org/10.1007/s00406-021-01377-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-021-01377-2