Abstract
Objective
Although existing guidelines have discouraged use of antipsychotics for general clinical high-risk (CHR) individuals, it is unclear if antipsychotics can prevent psychosis in higher-risk population. We aimed to study the comparative real-world effectiveness of antipsychotic treatments for preventing psychosis in higher-risk CHR individuals.
Methods
A total of 300 CHR individuals were identified using the structured interview for prodromal syndromes (SIPS) and followed the participants for 3 years. In total, 228(76.0%) individuals completed baseline assessments using the NAPLS-2 risk calculator (NAPLS-2-RC), and 210(92.1%) completed the follow-up. The sample was further stratified according to risk level. “Higher-risk” was defined based on the NAPLS-2-RC risk score (≥ 20%) and SIPS positive symptom total scores (≥ 10). The main outcome was conversion to psychosis and poor functional outcomes, defined as a global assessment of function (GAF) score lower than 60 at follow-up.
Results
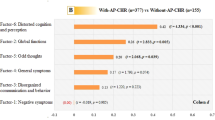
In higher-risk CHR individuals, we found no significant difference in the rate of conversion to psychosis or poor functional outcomes between the antipsychotic and no-antipsychotic groups. Low-risk individuals treated with antipsychotic drugs were more likely exhibit poor functional outcomes compared with the no-antipsychotics group(NAPLS-2-RC estimated risk: χ2 = 8.330, p = 0.004; Positive symptom severity: χ2 = 12.997, p < 0.001). No significant effective factors were identified for prevention of the conversion to psychosis; conversely, CHR individuals who were treated with high dose antipsychotics (olanzapine, aripiprazole) showed a significantly increased risk of poor functional outcomes.
Conclusions
In CHR individuals, antipsychotic treatment should be provided with caution because of the risk of poor functional outcomes. Further, antipsychotic treatment does not appear to prevent onset of psychosis in real‐world settings.



Similar content being viewed by others
References
Allen P, Luigjes J, Howes OD, Egerton A, Hirao K, Valli I, Kambeitz J, Fusar-Poli P, Broome M, McGuire P (2012) Transition to psychosis associated with prefrontal and subcortical dysfunction in ultra high-risk individuals. Schizophr Bull 38:1268–1276
Austin SF, Mors O, Secher RG, Hjorthoj CR, Albert N, Bertelsen M, Jensen H, Jeppesen P, Petersen L, Randers L, Thorup A, Nordentoft M (2013) Predictors of recovery in first episode psychosis: the opus cohort at 10 year follow-up. Schizophr Res 150:163–168
Beck K, Andreou C, Studerus E, Heitz U, Ittig S, Leanza L, Riecher-Rossler A (2019) Clinical and functional long-term outcome of patients at clinical high risk (chr) for psychosis without transition to psychosis: a systematic review. Schizophr Res. https://doi.org/10.1016/j.schres.2018.12.047
Bobo WV, Cooper WO, Stein CM, Olfson M, Graham D, Daugherty J, Fuchs DC, Ray WA (2013) Antipsychotics and the risk of type 2 diabetes mellitus in children and youth. JAMA Psychiat 70:1067–1075
Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, Seidman LJ, Perkins D, Tsuang M, McGlashan T, Heinssen R (2008) Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in north America. Arch Gen Psychiatry 65:28–37
Cannon TD, Yu C, Addington J, Bearden CE, Cadenhead KS, Cornblatt BA, Heinssen R, Jeffries CD, Mathalon DH, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Kattan MW (2016) An individualized risk calculator for research in prodromal psychosis. Am J Psychiatry 173:980–988
Carrion RE, Correll CU, Auther AM, Cornblatt BA (2017) A severity-based clinical staging model for the psychosis prodrome: longitudinal findings from the New York recognition and prevention program. Schizophr Bull 43:64–74
Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, Barale F, Caverzasi E, McGuire P (2012) Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry 69:220–229
Fusar-Poli P, Borgwardt S, Bechdolf A, Addington J, Riecher-Rossler A, Schultze-Lutter F, Keshavan M, Wood S, Ruhrmann S, Seidman LJ, Valmaggia L, Cannon T, Velthorst E, De Haan L, Cornblatt B, Bonoldi I, Birchwood M, McGlashan T, Carpenter W, McGorry P, Klosterkotter J, McGuire P, Yung A (2013) The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiat 70:107–120
Fusar-Poli P, Frascarelli M, Valmaggia L, Byrne M, Stahl D, Rocchetti M, Codjoe L, Weinberg L, Tognin S, Xenaki L, McGuire P (2015) Antidepressant, antipsychotic and psychological interventions in subjects at high clinical risk for psychosis: oasis 6-year naturalistic study. Psychol Med 45:1327–1339
Fusar-Poli P, Smieskova R, Kempton MJ, Ho BC, Andreasen NC, Borgwardt S (2013) Progressive brain changes in schizophrenia related to antipsychotic treatment? A meta-analysis of longitudinal MRI studies. Neurosci Biobehav Rev 37:1680–1691
Fusar-Poli P, Valmaggia L, McGuire P (2007) Can antidepressants prevent psychosis? Lancet 370:1746–1748
Galletly C, Castle D, Dark F, Humberstone V, Jablensky A, Killackey E, Kulkarni J, McGorry P, Nielssen O, Tran N (2016) Royal Australian and New Zealand college of psychiatrists clinical practice guidelines for the management of schizophrenia and related disorders. Aust N Z J Psychiatry 50:410–472
Harrow M, Jobe TH, Faull RN (2012) Do all schizophrenia patients need antipsychotic treatment continuously throughout their lifetime? A 20-year longitudinal study. Psychol Med 42:2145–2155
Hayasaka Y, Purgato M, Magni LR, Ogawa Y, Takeshima N, Cipriani A, Barbui C, Leucht S, Furukawa TA (2015) Dose equivalents of antidepressants: evidence-based recommendations from randomized controlled trials. J Affect Disord 180:179–184
Healey KM, Penn DL, Perkins D, Woods SW, Keefe RSE, Addington J (2018) Latent profile analysis and conversion to psychosis: characterizing subgroups to enhance risk prediction. Schizophr Bull 44:286–296
Ho BC, Andreasen NC, Ziebell S, Pierson R, Magnotta V (2011) Long-term antipsychotic treatment and brain volumes: a longitudinal study of first-episode schizophrenia. Arch Gen Psychiatry 68:128–137
Jones SH, Thornicroft G, Coffey M, Dunn G (1995) A brief mental health outcome scale-reliability and validity of the global assessment of functioning (gaf). Br J Psychiatry 166:654–659
Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L (2004) The brief assessment of cognition in schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res 68:283–297
Kern RS, Gold JM, Dickinson D, Green MF, Nuechterlein KH, Baade LE, Keefe RS, Mesholam-Gately RI, Seidman LJ, Lee C, Sugar CA, Marder SR (2011) The MCCB impairment profile for schizophrenia outpatients: results from the MATRICS psychometric and standardization study. Schizophr Res 126:124–131
Kern RS, Nuechterlein KH, Green MF, Baade LE, Fenton WS, Gold JM, Keefe RS, Mesholam-Gately R, Mintz J, Seidman LJ, Stover E, Marder SR (2008) The MATRICS consensus cognitive battery, part 2: co-norming and standardization. Am J Psychiatry 165:214–220
Kim E, Jang JH, Park HY, Shim G, Hwang JY, Kim SN, Kwon JS (2012) Pharmacotherapy and clinical characteristics of ultra-high-risk for psychosis according to conversion status: a naturalistic observational study. Early Interv Psychiatry 6:30–37
Leucht S, Samara M, Heres S, Davis JM (2016) Dose equivalents for antipsychotic drugs: the DDD method. Schizophr Bull 42(Suppl 1):S90-94
Levine SZ, Leucht S (2012) Early symptom response to antipsychotic medication as a marker of subsequent symptom change: an eighteen-month follow-up study of recent episode schizophrenia. Schizophr Res 141:168–172
Liu CC, Demjaha A (2013) Antipsychotic interventions in prodromal psychosis: safety issues. CNS Drugs 27:197–205
Liu CC, Sheu YH, Wu SY, Lai MC, Hwu HG (2010) Rapid response to antipsychotic treatment on psychotic prodrome: implications from a case series. Psychiatry Clin Neurosci 64:202–206
McGlashan T, Walsh B, Woods S (2010) The psychosis-risk syndrome: handbook for diagnosis and follow-up. Oxford University Press, New York
McGlashan TH, Zipursky RB, Perkins D, Addington J, Miller T, Woods SW, Hawkins KA, Hoffman RE, Preda A, Epstein I, Addington D, Lindborg S, Trzaskoma Q, Tohen M, Breier A (2006) Randomized, double-blind trial of olanzapine versus placebo in patients prodromally symptomatic for psychosis. Am J Psychiatry 163:790–799
McGorry PD, Yung AR, Phillips LJ, Yuen HP, Francey S, Cosgrave EM, Germano D, Bravin J, McDonald T, Blair A, Adlard S, Jackson H (2002) Randomized controlled trial of interventions designed to reduce the risk of progression to first-episode psychosis in a clinical sample with subthreshold symptoms. Arch Gen Psychiatry 59:921–928
Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, McFarlane W, Perkins DO, Pearlson GD, Woods SW (2003) Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull 29:703–715
Miller TJ, McGlashan TH, Rosen JL, Somjee L, Markovich PJ, Stein K, Woods SW (2002) Prospective diagnosis of the initial prodrome for schizophrenia based on the structured interview for prodromal syndromes: preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry 159:863–865
Morrison AP, French P, Walford L, Lewis SW, Kilcommons A, Green J, Parker S, Bentall RP (2004) Cognitive therapy for the prevention of psychosis in people at ultra-high risk: randomised controlled trial. Br J Psychiatry 185:291–297
Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, Essock S, Fenton WS, Frese FJ 3rd, Gold JM, Goldberg T, Heaton RK, Keefe RS, Kraemer H, Mesholam-Gately R, Seidman LJ, Stover E, Weinberger DR, Young AS, Zalcman S, Marder SR (2008) The MATRICS consensus cognitive battery, part 1: test selection, reliability, and validity. Am J Psychiatry 165:203–213
Piskulic D, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, McGlashan TH (2012) Negative symptoms in individuals at clinical high risk of psychosis. Psychiatry Res 196:220–224
Schennach-Wolff R, Seemuller FH, Mayr A, Maier W, Klingberg S, Heuser I, Klosterkotter J, Gastpar M, Hafner H, Sauer H, Schneider F, Gaebel W, Jager M, Moller HJ, Riedel M (2010) An early improvement threshold to predict response and remission in first-episode schizophrenia. Br J Psychiatry 196:460–466
Schmidt SJ, Schultze-Lutter F, Schimmelmann BG, Maric NP, Salokangas RK, Riecher-Rossler A, van der Gaag M, Meneghelli A, Nordentoft M, Marshall M, Morrison A, Raballo A, Klosterkotter J, Ruhrmann S (2015) EPA guidance on the early intervention in clinical high risk states of psychoses. Eur Psychiatry 30:388–404
Shapiro AM, Benedict RH, Schretlen D, Brandt J (1999) Construct and concurrent validity of the Hopkins verbal learning test-revised. Clin Neuropsychol 13:348–358
Shi C, He Y, Cheung EF, Yu X, Chan RC (2013) An ecologically valid performance-based social functioning assessment battery for schizophrenia. Psychiatry Res 210:787–793
Simonsen C, Faerden A, Romm KL, Berg AO, Bjella T, Sundet K, Ueland T, Andreassen O, Melle I (2017) Early clinical recovery in first-episode psychosis: symptomatic remission and its correlates at 1-year follow-up. Psychiatry Res 254:118–125
Tessner KD, Mittal V, Walker EF (2011) Longitudinal study of stressful life events and daily stressors among adolescents at high risk for psychotic disorders. Schizophr Bull 37:432–441
Woods SW, Addington J, Bearden CE, Cadenhead KS, Cannon TD, Cornblatt BA, Mathalon DH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, McGlashan TH (2013) Psychotropic medication use in youth at high risk for psychosis: comparison of baseline data from two research cohorts 1998–2005 and 2008–2011. Schizophr Res 148:99–104
Woods SW, Breier A, Zipursky RB, Perkins DO, Addington J, Miller TJ, Hawkins KA, Marquez E, Lindborg SR, Tohen M, McGlashan TH (2003) Randomized trial of olanzapine versus placebo in the symptomatic acute treatment of the schizophrenic prodrome. Biol Psychiatry 54:453–464
Woods SW, Martin A, Spector SG, McGlashan TH (2002) Effects of development on olanzapine-associated adverse events. J Am Acad Child Adolesc Psychiatry 41:1439–1446
Woods SW, Tully EM, Walsh BC, Hawkins KA, Callahan JL, Cohen SJ, Mathalon DH, Miller TJ, McGlashan TH (2007) Aripiprazole in the treatment of the psychosis prodrome: an open-label pilot study. Br J Psychiatry Suppl 51:s96-101
Yung AR, McGorry PD (1996) The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull 22:353–370
Zhang T, Li H, Tang Y, Niznikiewicz MA, Shenton ME, Keshavan MS, Stone WS, McCarley RW, Seidman LJ, Wang J (2018) Validating the predictive accuracy of the napls-2 psychosis risk calculator in a clinical high-risk sample from the sharp (shanghai at risk for psychosis) program. Am J Psychiatry 175:906–908
Zhang T, Li H, Woodberry KA, Seidman LJ, Chow A, Xiao Z, Wang J (2015) Interaction of social role functioning and coping in people with recent-onset attenuated psychotic symptoms: a case study of three Chinese women at clinical high risk for psychosis. Neuropsychiatr Dis Treat 11:1647–1654
Zhang T, Li H, Woodberry KA, Seidman LJ, Zheng L, Li H, Zhao S, Tang Y, Guo Q, Lu X, Zhuo K, Qian Z, Chow A, Li C, Jiang K, Xiao Z, Wang J (2014) Prodromal psychosis detection in a counseling center population in china: an epidemiological and clinical study. Schizophr Res 152:391–399
Zhang T, Li HJ, Woodberry KA, Xu LH, Tang YY, Guo Q, Cui HR, Liu XH, Chow A, Li CB, Jiang KD, Xiao ZP, Seidman LJ, Wang JJ (2017) Two-year follow-up of a Chinese sample at clinical high risk for psychosis: timeline of symptoms, help-seeking and conversion. Epidemiol Psychiatr Sci 26:287–298
Zheng L, Wang J, Zhang T, Li H, Li C, Jiang K (2012) The Chinese version of the sips/sops: a pilot study of reliability and validity. Chin Ment Health J 26:571–576
Acknowledgements
This study was supported by Ministry of Science and Technology of China, National Key R&D Program of China (2016YFC1306800), National Natural Science Foundation of China (82171544, 81901832), Science and Technology Commission of Shanghai Municipality (19441907800, 19ZR1445200, 17411953100, 16JC1420200, No.2018SHZDZX01, 19410710800, 19411969100, 19411950800), Shanghai Clinical Research Center for Mental Health (19MC1911100) and The Clinical Research Center at Shanghai Mental Health Center (CRC2018ZD01, CRC2018ZD04, CRC2018YB01 and CRC2019ZD02), Project of the Key Discipline Construction, Shanghai 3-Year Public Health Action Plan (GWV-10.1-XK18).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None of the authors had a conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, T., Wang, J., Xu, L. et al. Further evidence that antipsychotic medication does not prevent long-term psychosis in higher-risk individuals. Eur Arch Psychiatry Clin Neurosci 272, 591–602 (2022). https://doi.org/10.1007/s00406-021-01331-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-021-01331-2