Abstract
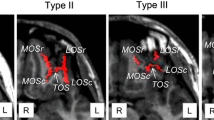
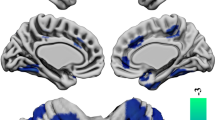
Morphological changes in the orbitofrontal cortex (OFC), such as an altered sulcogyral pattern of the ‘H-shaped’ orbital sulcus and a shallow olfactory sulcus, have been demonstrated in schizophrenia, possibly reflecting deviations in early neurodevelopment. However, it remains unclear whether patients with schizotypal features exhibit similar OFC changes. This magnetic resonance imaging study examined the OFC sulcogyral pattern (Types I, II, III, and IV) and olfactory sulcus morphology in 102 patients with schizophrenia, 47 patients with schizotypal disorder, and 84 healthy controls. The OFC sulcogyral pattern distribution between the groups was significantly different on the right hemisphere, with the schizophrenia patients showing a decrease in Type I (vs controls and schizotypal patients) and an increase in Type III (vs controls) expression. However, the schizotypal patients and controls did not differ in the OFC pattern. There were significant group differences in the olfactory sulcus depth bilaterally (schizophrenia patients < schizotypal patients < controls). Our findings suggest that schizotypal disorder, a milder form of schizophrenia spectrum disorders, partly shares the OFC changes (i.e., altered depth of the olfactory sulcus) with schizophrenia, possibly reflecting a common disease vulnerability. However, altered distribution of the OFC pattern specific to schizophrenia may at least partly reflect neurodevelopmental pathology related to a greater susceptibility to overt psychosis.


Similar content being viewed by others
References
Siever LJ, Kalus OF, Keefe RSE (1993) The boundaries of schizophrenia. Psychiatr Clin North Am 16:217–244
Siever LJ, Davis KL (2004) The pathophysiology of schizophrenia disorders: perspective from the spectrum. Am J Psychiatry 161:398–413
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association Press, Washington, DC
World Health Organization (1992) The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. World Health Organization, Geneva
Fervaha G, Remington G (2013) Neuroimaging findings in schizotypal personality disorder: a systematic review. Prog Neuropsychopharmacol Biol Psychiatry 43:96–107
Hazlett EA, Goldstein KE, Kolaitis JC (2012) A review of structural MRI and diffusion tensor imaging in schizotypal personality disorder. Curr Psychiatry Rep 14:70–78
Rosales RK, Lemay MJ, Yakovley PI (1968) The development and involution of massa intermedia with regard to age and sex. J Neuropathol Exp Neurol 27:166
Takahashi T, Suzuki M, Zhou SY, Nakamura K, Tanino R, Kawasaki Y, Seal ML, Seto H, Kurachi M (2008) Prevalence and length of the adhesio interthalamica in schizophrenia spectrum disorders. Psychiatry Res 164:90–94
Chiavaras MM, Petrides M (2000) Orbitofrontal sulci of the human and macaque monkey brain. J Comp Neurol 422:35–54
Chakirova G, Welch KA, Moorhead TW, Stanfield AC, Hall J, Skehel P, Brown VJ, Johnstone EC, Owens DG, Lawrie SM, McIntosh AM (2010) Orbitofrontal morphology in people at high risk of developing schizophrenia. Eur Psychiatry 25:366–372
Nakamura M, Nestor PG, McCarley RW, Levitt JJ, Hsu L, Kawashima T, Niznikiewicz M, Shenton ME (2007) Altered orbitofrontal sulcogyral pattern in schizophrenia. Brain 130:693–707
Takayanagi Y, Takahashi T, Orikabe L, Masuda N, Mozue Y, Nakamura K, Kawasaki Y, Itokawa M, Sato Y, Yamasue H, Kasai K, Okazaki Y, Suzuki M (2010) Volume reduction and altered sulco-gyral pattern of the orbitofrontal cortex in first-episode schizophrenia. Schizophr Res 121:55–65
Armstrong E, Schleicher A, Omran H, Curtis M, Zilles K (1995) The ontogeny of human gyrification. Cereb Cortex 5:56–63
Chi JG, Dooling EC, Gilles FH (1977) Gyral development of the human brain. Ann Neurol 1:86–93
Kringelbach ML, Rolls ET (2004) The functional neuroanatomy of the human orbitofrontal cortex: evidence from neuroimaging and neuropsychology. Prog Neurobiol 72:341–372
Nguyen AD, Pelavin PE, Shenton ME, Chilakamarri P, McCarley RW, Nestor PG, Levitt JJ (2011) Olfactory sulcal depth and olfactory bulb volume in patients with schizophrenia: an MRI study. Brain Imaging Behav 5:252–261
Takahashi T, Nakamura Y, Nakamura K, Ikeda E, Furuichi A, Kido M, Kawasaki Y, Noguchi K, Seto H, Suzuki M (2013) Altered depth of the olfactory sulcus in first-episode schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 40:167–172
Takahashi T, Nakamura Y, Nakamura K, Nishiyama S, Ikeda E, Furuichi A, Kido M, Noguchi K, Suzuki M (2013) Altered depth of the olfactory sulcus in subjects at risk of psychosis. Schizophr Res 149:186–187
Turetsky BI, Crutchley P, Walker J, Gur RE, Moberg PJ (2009) Depth of the olfactory sulcus: a marker of early embryonic disruption in schizophrenia? Schizophr Res 115:8–11
World Health Organization (1993) The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. World Health Organization, Geneva
Kawasaki Y, Suzuki M, Nohara S, Hagino H, Matsui M, Yamashita I, Takahashi T, Chitnis X, McGuire PK, Seto H, Kurachi M (2004) Structural brain differences in patients with schizotypal disorder and schizophrenia demonstrated by voxel-based morphometry. Eur Arch Psychiatry Clin Neurosci 254:406–414
Suzuki M, Zhou SY, Hagino H, Takahashi T, Kawasaki Y, Nohara S, Yamashita I, Matsui M, Seto H, Kurachi M (2004) Volume reduction of the right anterior limb of the internal capsule in patients with schizotypal disorder. Psychiatry Res 130:213–225
Suzuki M, Zhou SY, Takahashi T, Hagino H, Kawasaki Y, Niu L, Matsui M, Seto H, Kurachi M (2005) Differential contributions of prefrontal and temporolimbic pathology to mechanisms of psychosis. Brain 128:2109–2122
Takahashi T, Suzuki M, Zhou SY, Tanino R, Hagino H, Kawasaki Y, Matsui M, Seto H, Kurachi M (2006) Morphologic alterations of the parcellated superior temporal gyrus in schizophrenia spectrum. Schizophr Res 83:131–143
Andreasen NC, Flaum M, Arndt S (1992) The Comprehensive Assessment of Symptoms and History (CASH): an instrument for assessing diagnosis and psychopathology. Arch Gen Psychiatry 49:615–623
Andreasen NC (1984) The scale for the assessment of negative symptoms (SANS). The University of Iowa, Iowa City
Andreasen NC (1984) The scale for the assessment of positive symptoms (SAPS). The University of Iowa, Iowa City
Takahashi T, Nakamura Y, Nakamura Y, Aleksic B, Takayanagi Y, Furuichi A, Kido M, Nakamura M, Sasabayashi D, Ikeda M, Noguchi K, Kaibuchi K, Iwata N, Ozaki N, Suzuki M (2014) The polymorphism of YWHAE, a gene encoding 14-3-3epsilon, and orbitofrontal sulcogyral pattern in patients with schizophrenia and healthy subjects. Prog Neuropsychopharmacol Biol Psychiatry 51:166–171
Zhou SY, Suzuki M, Hagino H, Takahashi T, Kawasaki Y, Nohara S, Yamashita I, Seto H, Kurachi M (2003) Decreased volume and increased asymmetry of the anterior limb of the internal capsule in patients with schizophrenia. Biol Psychiatry 54:427–436
Bartholomeusz CF, Whittle SL, Montague A, Ansell B, McGorry PD, Velakoulis D, Pantelis C, Wood SJ (2013) Sulcogyral patterns and morphological abnormalities of the orbitofrontal cortex in psychosis. Prog Neuropsychopharmacol Biol Psychiatry 44:168–177
Rombaux P, Grandin C, Duprez T (2009) How to measure olfactory bulb volume and olfactory sulcus depth? B-ENT 5(Suppl 13):53–60
Lavoie S, Bartholomeuz CF, Nelson B, Lin A, McGorry PD, Velakoulis D, Whittle SL, Yung AR, Pantelis C, Wood SJ (2014) Sulcogyral pattern and sulcal count of the orbitofrontal cortex in individuals at ultra high risk for psychosis. Schizophr Res 154:93–99
Lener MS, Wong E, Tang CY, Byne W, Goldstein KE, Blair NJ, Haznedar MM, New AS, Chemerinski E, Chu KW, Rimsky LS, Siever LJ, Koenigsberg HW, Hazlett EA (2014) White matter abnormalities in schizophrenia and schizotypal personality disorder. Schizophr Bull. doi: 10.1093/schbul/sbu093 (in press)
Pantelis C, Yücel M, Wood SJ, Velakoulis D, Sun D, Berger G, Stuart GW, Yung A, Phillips L, McGorry PD (2005) Structural brain imaging evidence for multiple pathological processes at different stages of brain development in schizophrenia. Schizophr Bull 31:672–696
Takahashi T, Wood SJ, Yung AR, Nelson B, Lin A, Yücel M, Phillips LJ, Nakamura Y, Suzuki M, Brewer WJ, Proffitt TM, McGorry PD, Velakoulis D, Pantelis C (2014) Altered depth of the olfactory sulcus in ultra high-risk individuals and patients with psychotic disorders. Schizophr Res 153:18–24
Raine A, Lencz T, Yaralian P, Bihrle S, LaCasse L, Ventura J, Colletti P (2002) Prefrontal structural and functional deficits in schizotypal personality disorder. Schizophr Bull 28:501–513
Andreasen NC, Liu D, Ziebell S, Vora A, Ho BC (2013) Relapse duration, treatment intensity, and brain tissue loss in schizophrenia: a prospective longitudinal MRI study. Am J Psychiatry 170:609–615
Lieberman JA, Tollefson GD, Charles C, Zipursky R, Sharma T, Kahn RS, Keefe RS, Green AI, Gur RE, McEvoy J, Perkins D, Hamer RM, Gu H, Tohen M, HGDH Study Group (2005) Antipsychotic drug effects on brain morphology in first-episode psychosis. Arch Gen Psychiatry 62:361–370
Moncrieff J, Leo J (2010) A systematic review of the effects of antipsychotic drugs on brain volume. Psychol Med 40:1409–1422
Magnotta VA, Andreasen NC, Schultz SK, Harris G, Cizadlo T, Heckel D, Nopoulos P, Flaum M (1999) Quantitative in vivo measurement of gyrification in the human brain: changes associated with aging. Cereb Cortex 9:151–160
Pantelis C, Velakoulis D, Wood SJ, Yücel M, Yung AR, Phillips LJ, Sun DQ, McGorry PD (2007) Neuroimaging and emerging psychotic disorders: the Melbourne ultra-high risk studies. Int Rev Psychiatry 19:371–381
van Haren NE, Schnack HG, Cahn W, van den Heuvel MP, Lepage C, Collins L, Evans AC, Hulshoff Pol HE, Kahn RS (2011) Changes in cortical thickness during the course of illness in schizophrenia. Arch Gen Psychiatry 68:871–880
Sun D, Stuart GW, Jenkinson M, Wood SJ, McGorry PD, Velakoulis D, van Erp TG, Thompson PM, Toga AW, Smith DJ, Cannon TD, Pantelis C (2009) Brain surface contraction mapped in first-episode schizophrenia: a longitudinal magnetic resonance imaging study. Mol Psychiatry 14:976–986
Huttenlocher PR (1979) Synaptic density in human frontal cortex—developmental changes and effects of aging. Brain Res 163:195–205
Sowell ER, Peterson BS, Thompson PM, Welcome SE, Henkenius AL, Toga AW (2003) Mapping cortical change across the human life span. Nat Neurosci 6:309–315
Watanabe H, Nakamura M, Ohno T, Itahashi T, Tanaka E, Ohta H, Yamada T, Kanai C, Iwanami A, Kato N, Hashimoto R (2014) Altered orbitofrontal sulcogyral patterns in adult males with high-functioning autism spectrum disorders. Soc Cogn Affect Neurosci 9:520–528
Whittle S, Bartholomeusz C, Yücel M, Dennison M, Vijayakumar N, Allen NB (2014) Orbitofrontal sulcogyral patterns are related to temperamental risk for psychopathology. Soc Cogn Affect Neurosci 9:232–239
Acknowledgments
This research was supported in part by Grants-in-Aid for Scientific Research (C) (Nos. 22591275, 24591699, 26461739) and Grants-in-Aid for Scientific Research (B) (No. 24390281) from the Japanese Society for the Promotion of Science, Health and Labour Sciences Research Grants (Comprehensive Research on Disability, Health and Welfare, H23-Seishin-Ippan-002 and H23-Seishin-Ippan-009), and Research Grants from the JSPS Asian Core Program and the Research Group For Schizophrenia, Japan. The authors would like to thank Prof. Hideki Origasa (Department of Biostatistics and Clinical Epidemiology, University of Toyama Graduate School of Medicine and Pharmaceutical Sciences) for his support in statistical analyses. We would also like to thank the radiological technologists, especially Mr. Koichi Mori and Mr. Sadanori Ito, who assisted in the MRI data collection at Toyama University Hospital.
Conflict of interest
There are no conflicts of interest for any of the authors including any financial, personal, or other relationships with other people or organizations within three years of beginning the submitted work that could inappropriately influence, or be perceived to influence, our work.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
406_2015_587_MOESM1_ESM.pptx
Scatter plots for the olfactory sulcus depth, age, and intracranial volume (ICV) in each diagnostic group. Only the age among these variables was not normally distributed (Kolmogorov–Smirnov test, p < 0.001), but there was no quadratic (left, p = 0.34; right, p = 0.37) or cubic (left, p = 0.44; right, p = 0.50) correlation between age and sulcus depth (PPTX 469 kb)
Rights and permissions
About this article
Cite this article
Nishikawa, Y., Takahashi, T., Takayanagi, Y. et al. Orbitofrontal sulcogyral pattern and olfactory sulcus depth in the schizophrenia spectrum. Eur Arch Psychiatry Clin Neurosci 266, 15–23 (2016). https://doi.org/10.1007/s00406-015-0587-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-015-0587-z