Abstract
Purpose
To evaluate the prognostic value of the number of positive lymph nodes (NPLN), the ratio of positive lymph nodes (pLNR), and the logarithmic ratio of positive lymph nodes (LODDS) in patients with parotid gland carcinoma. On this basis, establishing and validating an optimal nomogram.
Methods
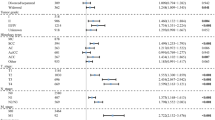
A total of 895 patients with T1-4N1-3M0 parotid gland carcinoma were included in our study from the Surveillance, Epidemiology, and End Results (SEER) database. Patients’ data were randomly assigned to the training cohort and the validation cohort by a ratio of 7:3. Univariate and multivariate COX regression analysis were used to explore the relationship between the study factors and the prognosis of parotid gland carcinoma, including overall survival (OS) and cause-specific survival (CSS). The Akaike Information Criterion (AIC) was used to evaluate model fit. Harrell's concordance index (C-index), integrated discrimination improvement (IDI), and net reclassification index (NRI) were used to evaluate the predictive ability of these models. The decision curve analysis was used to evaluate the clinical benefit of the nomograms compared with the TNM stage.
Results
NPLN, pLNR, and LODDS are independent risk factors for the prognostic of PGC. According to the AIC, C index, IDI, and NRI, the models combined with NPLN and LODDS were the best. The decision curves suggested that our nomograms had good predictive abilities for the prognosis of parotid gland carcinoma.
Conclusion
The two nomograms which contained NPLN and LODDS had the potential to predict OS and CSS in patients with parotid gland carcinoma.





Similar content being viewed by others
Data availability
The data that support the findings of this study are available from SEER database but restrictions apply to the availability of these data, which were used under license for the current study (ID:12111-Nov2021), and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of SEER database.
References:
McGurk M, Renehan A (2001) Controversies in the management of salivary gland disease. Oxford University Press, Oxford
Lewis AG, Tong T, Maghami E (2016) Diagnosis and management of malignant salivary gland tumors of the parotid gland. Otolaryngol Clin N Am 49:343–380
Chang JW, Hong HJ, Ban MJ et al (2015) Prognostic factors and treatment outcomes of parotid gland cancer: a 10-year single-center experience. Otolaryngol Head Neck Surg 153:981–989
Poorten VV, Hart A, Vauterin T et al (2009) Prognostic index for patients with parotid carcinoma: international external validation in a Belgian-German database. Cancer 115:540–550
Stenner M, Molls C, Luers JC et al (2012) Occurrence of lymph node metastasis in early-stage parotid gland cancer. Eur Arch Otorhinolaryngol 269:643–648
Ghosh-Laskar S, Murthy V, Wadasadawala T et al (2011) Mucoepidermoid carcinoma of the parotid gland: factors affecting outcome. Head Neck 33:497–503
Kouka M, Koehler B, Buentzel J et al (2022) Role of intraparotid and neck lymph node metastasis in primary parotid cancer surgery: a population-based analysis. Cancers (Basel) 14:2822
Patel KN, Salunke A, Bhatt S et al (2021) Log ODDS (LODDS) of positive lymph nodes as a predictor of overall survival in squamous cell carcinoma of the penis. J Surg Oncol 123:1836–1844
Li T, Yang Y, Wu W et al (2021) Prognostic implications of ENE and LODDS in relation to lymph node-positive colorectal cancer location. Transl Oncol 14:101190
Gu P, Deng J, Sun Z et al (2021) Superiority of log odds of positive lymph nodes (LODDS) for prognostic prediction after gastric cancer surgery: a multi-institutional analysis of 7620 patients in China. Surg Today 51:101–110
Qian K, Sun W, Guo K et al (2019) The number and ratio of positive lymph nodes are independent prognostic factors for patients with major salivary gland cancer: Results from the surveillance, epidemiology, and End Results dataset. Eur J Surg Oncol 45:1025–1032
Doll KM, Rademaker A, Sosa JA (2018) Practical guide to surgical data sets: surveillance, epidemiology, and end results (SEER) database. JAMA Surg 153:588–589
Camp RL, Dolled-Filhart M, Rimm DL (2004) X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res 10:7252–7259
George B, Seals S, Aban I (2014) Survival analysis and regression models. J Nucl Cardiol 21:686–694
Schober P, Boer C, Schwarte LA (2018) Correlation coefficients: appropriate use and interpretation. Anesth Analg 126:1763–1768
Portet S (2020) A primer on model selection using the Akaike Information Criterion. Infect Dis Model 5:111–128
Leslie WD, Schousboe JT, Lix LM (2016) Towards better use of the net reclassification improvement (NRI) index. Osteoporos Int 27:411–412
Pencina MJ, Fine JP, D’Agostino RB Sr (2017) Discrimination slope and integrated discrimination improvement—properties, relationships and impact of calibration. Stat Med 36:4482–4490
Van Calster B, Wynants L, Verbeek JFM et al (2018) Reporting and interpreting decision curve analysis: a guide for investigators. Eur Urol 74:796–804
Liu Y, Sun M, Xiong Y et al (2022) Construction and validation of prognosis nomogram for metastatic lung squamous cell carcinoma: a population-based study. Technol Cancer Res Treat 21:15330338221132036
Wang P, Song Q, Lu M et al (2022) Establishment and validation of a postoperative predictive model for patients with colorectal mucinous adenocarcinoma. World J Surg Oncol 20:330
Li J, Chen Z, Su K, Zeng J (2015) Clinicopathological classification and traditional prognostic indicators of breast cancer. Int J Clin Exp Pathol 8:8500–8505
Niu X, Fang Q, Liu F (2019) Role of intraparotid node metastasis in mucoepidermoid carcinoma of the parotid gland. BMC Cancer 19:417
Ichikura T, Ogawa T, Chochi K et al (2003) Minimum number of lymph nodes that should be examined for the international union against cancer/American Joint Committee on cancer TNM classification of gastric carcinoma. World J Surg 27:330–333
Sun Z, Zhu GL, Lu C et al (2009) The impact of N-ratio in minimizing stage migration phenomenon in gastric cancer patients with insufficient number or level of lymph node retrieved: results from a Chinese mono-institutional study in 2159 patients. Ann Oncol 20:897–905
Marchet A, Mocellin S, Ambrosi A et al (2007) The ratio between metastatic and examined lymph nodes (N Ratio) is an independent prognostic factor in gastric cancer regardless of the type of lymphadenectomy: results from an italian multicentric study in 1853 patients. Ann Surg 245:543–552
Celen O, Yildirim E, Berberoglu U (2007) Prognostic impact of positive lymph node ratio in gastric carcinoma. J Surg Oncol 96:95–101
Bhattacharyya N, Fried MP (2005) Determinants of survival in parotid gland carcinoma: a population-based study. Am J Otolaryngol 26:39–44
Honda K, Tanaka S, Shinohara S et al (2018) Survival in patients with parotid gland carcinoma—results of a multi-center study. Am J Otolaryngol 39:65–70
Jering M, Mayer M, Thölken R et al (2022) Cancer-specific and overall survival of patients with primary and metastatic malignancies of the parotid gland—a retrospective study. J Cranio-Maxillofac Surg 50:456–461
Funding
1. Special Finance Project of Fujian Province [Grant numbers: 2019B022]. 2. Leading project of Fujian Science and Technology Department [Grant numbers: 2021Y0016]. 3.Innovation Joint Fund of Fujian Science and Technology Department [Grant numbers: 2020Y9085].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest in the work.
Ethical approval
Ethics approval or patient written informed consent were not required because all analyses in our study were performed based on data from the public databases (the SEER database, PubMed, EMBASE, and Cochrane databases).
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, X., Lin, Q., Chen, X. et al. Number of positive lymph nodes combined with the logarithmic ratio of positive lymph nodes predicts long-term survival for patients with node-positive parotid gland carcinoma after surgery: a SEER population-based study. Eur Arch Otorhinolaryngol 280, 2541–2550 (2023). https://doi.org/10.1007/s00405-023-07848-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-07848-7