Abstract
Purpose
Compare awake evaluation (modified Mallampati score—MMs, Müller maneuver—MM) to drug-induced sleep endoscopy (DISE) findings according to NOHL (nose–oropharynx–hypopharynx–larynx) classification in moderate-to-severe OSAHS patients.
Methods
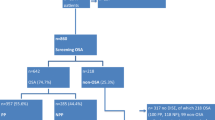
43 moderate-to-severe OSAHS patients referred to our ENT department were enrolled over a 2-year period. In this observational prospective study, each patient was evaluated by the same ENT team both in wakefulness and during pharmacologically induced sleep. Level and severity of the obstruction were described.
Results
The comparison of degree of collapsibility was statistically significative only at hypopharyngeal level: 41.8% of the patients showed a hypopharyngeal obstruction in wakefulness whereas 88.3% in DISE (p = 0.000). Laryngeal level was found in 18.6% patients during awake examination, conversely DISE demonstrated laryngeal obstruction in 4.6%. DISE identified significantly higher incidence of multilevel collapses (p = 0.001). However, the incidence of oropharyngeal obstruction in patients classified as MMs I and II was significantly higher in DISE compared to MM (p = 0.021).
Conclusion
DISE is the best predictor of hypopharyngeal obstruction, whereas MM underestimates the severity of the collapse at this level. DISE is more reliable than MM to identify the obstruction in patients with MMs score I and II.
Similar content being viewed by others
Availability of data and materials
Data are available upon reasonable request to the corresponding author.
Code availability
N/A.
References
Lee W, Nagubadi S, Kryger MH, Mokhlesi B (2008) Epidemiology of obstructive sleep apnea: a population-based perspective. Expert Rev Respir Med 2(3):349–364
Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR (2008) Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 31(8):1079–1085
McNicholas WT, Bonsigore MR, Management Committee of EU COST ACTION B26 (2007) Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J 29(1):156–178 (Erratum in: Eur Respir J. 2007 Mar;29(3):614. Bonsignore, M R [corrected to Bonsigore, M R])
Chung F, Memtsoudis SG, Ramachandran SK, Nagappa M, Opperer M, Cozowicz C, Patrawala S, Lam D, Kumar A, Joshi GP, Fleetham J, Ayas N, Collop N, Doufas AG, Eikermann M, Englesakis M, Gali B, Gay P, Hernandez AV, Kaw R, Kezirian EJ, Malhotra A, Mokhlesi B, Parthasarathy S, Stierer T, Wappler F, Hillman DR, Auckley D (2016) Society of anesthesia and sleep medicine guidelines on preoperative screening and assessment of adult patients with obstructive sleep apnea. Anesth Analg 123(2):452–473
Giles TL, Lasserson TJ, Smith BJ, White J, Wright J, Cates CJ (2006) Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev 1:CD001106. https://doi.org/10.1002/14651858.CD001106.pub2 (Update in: Cochrane Database Syst Rev. 2006;(3):CD00110)
Haniffa M, Lasserson TJ, Smith I (2004) Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnoea. Cochrane Database Syst Rev 4:CD003531. https://doi.org/10.1002/14651858.CD003531.pub2 (update in: Cochrane Database Syst Rev. 2009;(4):CD003531)
Rotenberg BW, Vicini C, Pang EB, Pang KP (2016) Reconsidering first-line treatment for obstructive sleep apnea: a systematic review of the literature. J Otolaryngol Head Neck Surg 45:23
Mulholland GB, Jeffery CC, Ziai H, Hans V, Seikaly H, Pang KP, Rotenberg BW (2019) Multilevel palate and tongue base surgical treatment of obstructive sleep apnea: a systematic review and meta-analysis. Laryngoscope 129:1712–1721
Ryu HH, Kim CH, Cheon SM, Bae WY, Kim SH, Koo SK, Kim MS, Kim BJ (2015) The usefulness of cephalometric measurement as a diagnostic tool for obstructive sleep apnea syndrome: a retrospective study. Oral Surg Oral Med Oral Pathol Oral Radiol 119(1):20–31
Fujita S (1994) Pharyngeal surgery for obstructive sleep apnea and snoring In: Fairbanks DNF (ed) Snoring and Obstructive Sleep Apnea, II edn. Raven Press, New York, pp 77–95
Friedman M, Ibrahim H, Bass L (2002) Clinical staging for sleep-disordered breathing. Otolaryngol Head Neck Surg 127(1):13–21
Friedman M, Hamilton C, Samuelson CG, Lundgren ME, Pott T (2013) Diagnostic value of the Friedman tongue position and Mallampati classification for obstructive sleep apnea: a meta-analysis. Otolaryngol Head Neck Surg 148(4):540–547
Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B, Freiberger D, Liu PL (1985) A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J 32(4):429–434
Friedman M, Tanyeri H, La Rosa M, Landsberg R, Vaidyanathan K, Pieri S, Caldarelli D (1999) Clinical predictors of obstructive sleep apnea. Laryngoscope 109:1901–1907
Sher AE, Thorpy MJ, Spielman AJ, Shprintzen RJ, Burack B, Mcgregor PA (1985) Predictive value of Müller maneuver in selection of patients for uvulopalatopharyngoplasty. Laryngoscope 95:1483–1487
Croft C, Pringle M (1991) Sleep nasendoscopy: a technique of assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol Allied Sci 16:504–509
Pringle MB, Croft CB (1991) A comparison of sleep nasendoscopy and the muller manoeuvre. Clin Otolaryngol Allied Sci 16:559–562
Hewitt RJD, Dasgupta A, Singh A et al (2009) Is sleep nasendoscopy a valuable adjunct to clinical examination in the evaluation of upper airway obstruction? Eur Arch Otorhinolaryngol 266:691–697
Blumen MB, Latournerie V, Bequignon E et al (2005) Are the obstruction sites visualized on drug-induced sleep endoscopy reliable? Sleep Breath 19:1021–1026
Certal VF, Pratas R, Guimarães L, Lugo R, Tsou Y, Camacho M, Capasso R (2016) Awake examination versus DISE for surgical decision making in patients with OSA: a systematic review. Laryngoscope 126:768–774
De Vito A, Carrasco Llatas M, Vanni A, Bosi M, Braghiroli A, Campanini A, de Vries N, Hamans E, Hohenhorst W, Kotecha BT, Maurer J, Montevecchi F, Piccin O, Sorrenti G, Vanderveken OM, Vicini C (2014) European position paper on drug-induced sedation endoscopy (DISE). Sleep Breath 18(3):453–465
De Vito A, Carrasco Llatas M, Ravesloot MJ, Kotecha B, De Vries N, Hamans E, Maurer J, Bosi M, Blumen M, Heiser C, Herzog M, Montevecchi F, Corso RM, Braghiroli A, Gobbi R, Vroegop A, Vonk PE, Hohenhorst W, Piccin O, Sorrenti G, Vanderveken OM, Vicini C (2018) European position paper on drug-induced sleep endoscopy: 2017 update. Clin Otolaryngol 43(6):1541–1552
Dijemeni E, D’Amone G, Gbati I (2017) Drug-induced sedation endoscopy (DISE) classification systems: a systematic review and meta-analysis. Sleep Breath 21(4):983–994
Carrasco-Llatas M, Matarredona-Quiles S, De Vito A, Chong KB, Vicini C (2019) Drug-induced sleep endoscopy: technique, indications, tips and pitfalls. Healthcare (Basel) 7(3):93
Vicini C, De Vito A, Benazzo M, Frassineti S, Campanini A, Frasconi P, Mira E (2012) The nose oropharynx hypopharynx and larynx (NOHL) classification: a new system of diagnostic standardized examination for OSAHS patients. Eur Arch Otorhinolaryngol 269(4):1297–1300
Berry RB, Brooks R, Gamaldo CE, Harding SM, Lloyd RM, Marcus CL, Vaughn BV for the American Academy of Sleep Medicine (2015) The AASM manual for the scoring of sleep and associated events: rules, terminology and Technical Specifications, Version 2.2. American Academy of Sleep Medicine, Darien, Illinois. http://www.aasmnet.org
Lin H-C, Friedman M, Chang H-W, Gurpinar B (2008) The efficacy of multilevel surgery of the upper airway in adults with obstructive sleep apnea/hypopnea syndrome. Laryngoscope 118:902–908
Soares D, Folbe AJ, Yoo G, Badr MS, Rowley JA, Lin HS (2013) Drug-induced sleep endoscopy vs awake Müller’s maneuver in the diagnosis of severe upper airway obstruction. Otolaryngol Head Neck Surg 148(1):151–156
Cavaliere M, Russo F, Iemma M (2013) Awake versus drug-induced sleep endoscopy: evaluation of airway obstruction in obstructive sleep apnea/hypopnoea syndrome. Laryngoscope 123:2315–2318
Fernández-Julián E, García-Pérez MÁ, García-Callejo J, Ferrer F, Martí F, Marco J (2014) Surgical planning after sleep versus awake techniques in patients with obstructive sleep apnea. Laryngoscope 124:1970–1974
Yegïn Y, Çelik M, Kaya KH, Koç AK, Kayhan FT (2017) Comparison of drug-induced sleep endoscopy and Müller’s maneuver in diagnosing obstructive sleep apnea using the VOTE classification system. Braz J Otorhinolaryngol 83(4):445–450
Zerpa Zerpa V, Carrasco Llatas M, Agostini Porras G, Dalmau GJ (2015) Drug-induced sedation endoscopy versus clinical exploration for the diagnosis of severe upper airway obstruction in OSAHS patients. Sleep Breath 19(4):1367–1372
Van de Perck E, Vroegop AV, Op de Beeck S, Dieltjens M, Verbruggen AE, Van de Heyning PH, Braem MJ, Vanderveken OM (2021) Awake endoscopic assessment of the upper airway during tidal breathing: definition of anatomical features and comparison with drug-induced sleep endoscopy. Clin Otolaryngol 46(1):234–242
Wang W-M, Hsu Y-B, Lan M-Y, Yang M-C, Huang T-T, Liu C-J, Lan M-C (2018) The relationship between modified Mallampati score, Müller’s maneuver and drug-induced sleep endoscopy regarding retrolingual obstruction. Ann Otol Rhinol Laryngol 127(7):463–469
Suratt PM, McTier RF, Wilhoit SC (1988) Upper airway muscle activation is augmented in patients with obstructive sleep apnea compared with that in normal subjects. Am Rev Respir Dis 137(4):889–894
Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP (2010) Pathophysiology of sleep apnea. Physiol Rev 90(1):47–112
Shteamer JW, Dedhia RC (2017) Sedative choice in drug-induced sleep endoscopy: a neuropharmacology-based review. Laryngoscope 127:273–279
Delakorda M, Ovsenik N (2019) Epiglottis shape as a predictor of obstruction level in patients with sleep apnea. Sleep Breath 23:311–317
Catalfumo F, Golz A, Westerman S, Gilbert L, Joachims H, Goldenberg D (1998) The epiglottis and obstructive sleep apnoea syndrome. J Laryngol Otol 112(10):940–943
Torre C, Camacho M, Liu SY-C, Huon L-K, Capasso R (2016) Epiglottis collapse in adult obstructive sleep apnea: a systematic review. Laryngoscope 126:515–523
Kavcic P, Koren A, Koritnik B, Fajdiga I, Groselj LD (2015) Sleep magnetic resonance imaging with electroencephalogram in obstructive sleep apnea syndrome. Laryngoscope 125:1485–1490
den Herder C, van Tinteren H, de Vries N (2005) Sleep endoscopy versus modified Mallampati score in sleep apnea and snoring. Laryngoscope 115:735–739
Aktas O, Erdur O, Cirik AA, Kayhan FT (2015) The role of drug-induced sleep endoscopy in surgical planning for obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 272:2039–2043
Lin HY, Lin YC, Hsu YS, Shih LC, Nelson T, Chang WD, Tsou YA (2020) Comparison of findings between clinical examinations and drug-induced sleep endoscopy in patients with obstructive sleep apnea syndrome. Int J Environ Res Public Health 17(17):6041
Carrasco-Llatas M, Zerpa-Zerpa V, Dalmau-Galofre J (2017) Reliability of drug-induced sedation endoscopy: interobserver agreement. Sleep Breath 21(1):173–179
Vroegop AV, Vanderveken OM, Wouters K, Hamans E, Dieltjens M, Michels NR, Hohenhorst W, Kezirian EJ, Kotecha BT, de Vries N, Braem MJ, Van de Heyning PH (2013) Observer variation in drug-induced sleep endoscopy: experienced versus nonexperienced ear, nose, and throat surgeons. Sleep 36(6):947–953
Kezirian EJ, White DP, Malhotra A, Ma W, McCulloch CE, Goldberg AN (2010) Interrater reliability of drug-induced sleep endoscopy. Arch Otolaryngol Head Neck Surg 136(4):393–397
Rodriguez-Bruno K, Goldberg AN, McCulloch CE, Kezirian EJ (2009) Test–retest reliability of drug-induced sleep endoscopy. Otolaryngol Head Neck Surg 140(5):646–651
Bartier S, Blumen M, Chabolle F (2020) Is image interpretation in drug-induced sleep endoscopy that reliable? Sleep Breath 24(2):677–685
Koutsourelakis I, Safiruddin F, Ravesloot M, Zakynthinos S, de Vries N (2012) Surgery for obstructive sleep apnea: Sleep endoscopy determinants of outcome. Laryngoscope 122:2587–2591
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization: [IB, LG]. Methodology: [IB, LG]. Formal analysis and investigation: [IB, MO, MM, MM]. Writing—original draft preparation: [IB]. Writing—review and editing: [IB, MO, LG]. Supervision: [GR, LG].
Corresponding author
Ethics declarations
Conflict of interest
All authors declare they have no conflict of interest.
Ethics approval
N/A.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bindi, I., Ori, M., Marchegiani, M. et al. Diagnosis of upper airways collapse in moderate-to-severe OSAHS patients: a comparison between drug-induced sleep endoscopy and the awake examination. Eur Arch Otorhinolaryngol 279, 2167–2173 (2022). https://doi.org/10.1007/s00405-021-07184-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-07184-8