Abstract
Purpose
Skeletal muscle mass (SMM) loss and sarcopenia have been identified as risk factors for postoperative complications. The aim of this study was to investigate the relationship between pharyngocutaneous fistula (PCF) formation after total laryngectomy (TL) and SMM assessed from a computed tomography image of the 3rd cervical vertebra (C3).
Methods
Retrospective study of 86 male patients who underwent TL between 2013 and 2019 in a single institution. We excluded women from the analysis due to our limited sample. SMM was determined from cross-sectional muscle area (CSMA) measurement at C3 using the ImageJ software. Results were compared with those for the skeletal muscle mass index (SMMI) calculated from the estimated measure at 3rd lumbar vertebra (L3).
Results
PCF formation occurred in 21/86 patients. According to the CSMA at a C3 cut-off of 35.5cm2, of 18 patients (20.9%) with low SMM, 9 developed PCFs (50.0%). Among patients with normal SMM (n = 68, 79.1%), 12 developed PCFs (17.6%). The CSMA at C3 was the only variable significantly associated with PCF risk, which was 4.7 times greater in patients with low SMM (p = 0.007). Sarcopenia was more frequent in underweight patients (p = 0.0001), patients undergoing extended surgeries (p = 0.003), or presenting preoperative anaemia (p = 0.009) or hypoalbuminemia (p = 0.027).
Conclusion
Measuring the CSMA at C3 obtained results equivalent to those obtained by calculating the SMMI at L3, suggesting that direct SMM assessment from C3 is a useful approach to evaluating PCF formation risk after TL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For some advanced laryngeal and hypopharyngeal tumours, total laryngectomy (TL) is the initial treatment or a salvage treatment after local recurrence. A postoperative complication of TL is the formation of a pharyngocutaneous fistula (PCF). While several observational studies and meta-analyses review predisposing factors for PCF formation [1,2,3,4,5], there is currently no consensus as to which of those factors is the most predictive. In a study performed in our hospital [6], factors identified as being significantly related to PCF formation were the extent of surgery and the presence of postoperative haemoglobin levels below 99 g/L.
A growing concern regarding the nutritional status of patients with cancer highlights sarcopenia as a risk factor for treatment-associated complications [7,8,9,10,11,12]. Sarcopenia, defined by the European Working Group on Sarcopenia in Older People (EWGSOP) [13] as progressive and generalized skeletal muscle impairment, is diagnosed by objectifying decreased muscle strength and altered quantity or quality of muscle tissue. Patients with head and neck carcinomas (HNSCC) frequently lose muscle mass due to the metabolic characteristics of their tumour, to its location at the level of the upper airway and digestive tract, and to important sequelae or toxicities produced by treatments [14]. The reported prevalence of sarcopenia in patients with HNSCC varies widely, from as low as 6% [15] to as high as 77% [9].
Of several techniques described to evaluate sarcopenia, cervical computed tomography (CT), a component of routine tumour staging studies, has been proposed as especially useful for patients with HNSCC [16]. From CT images obtained at the level of the 3rd cervical vertebra (C3), muscle tissue can be accurately quantified so as to determine body composition. Since Swartz et al. [16] demonstrated that skeletal muscle mass (SMM) measured at C3 is proportional to muscle mass measured at the 3rd lumbar vertebra (L3)—the standard location for quantifying SMM—that formula has been used in most studies of sarcopenia in patients with HNSCC to estimate the cross-sectional muscle area (CSMA) at L3 from the area measured at C3 [7, 10, 11, 17,18,19,20]. A skeletal muscle mass index (SMMI) is then obtained by dividing the L3 area by the squared height of the patient.
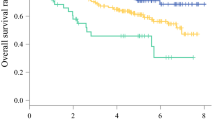
However, use of the Swartz et al. [16] formula is complicated in routine clinical practice. According to the reviewed literature, only Jung et al. [21] have evaluated diminished SMM based on measurements at C3; in that study, which included 305 patients with advanced HNSCC in different locations, grouped according to treatment (surgical vs radiotherapy ± chemotherapy), survival was analysed according to the CSMA at the C3 level, with the authors observing that patients with a CSMA at C3 of less than 56.3 cm2 had poorer overall survival.
There is no consensus on what cut-off point should be used to define low SMM, but it is probably necessary to set a specific cut-off point for each sex due to differences in muscle constitution. Prado et al. [22], whose sex-specific cut-offs for defining sarcopenia have been used multiple times in the literature [9, 23,24,25], found the mean CSMA at L3 value to be higher in obese men than in obese women (180.2 cm2 and 125.1 cm2, respectively). In our institution, our female population undertaking a TL is limited; therefore, we decided to exclude women from this study.
The aim of the present study was to analyse the relationship between low SMM, as determined from the CSMA measured directly from a CT scan slice of C3, and postoperative PCF formation in male patients treated with TL.
Materials and methods
The study followed the ethical standards of the latest version of the Helsinki Declaration, and was evaluated and authorized by our hospital’s Clinical Research Ethics Committee [reference 19/126 (OBS)]. Given the retrospective nature of the study, the informed consent of the patients included in the study was not considered necessary.
Patient description
We retrospectively reviewed all TL procedures performed consecutively between 2013 and 2019 in our hospital. For 105 of the 113 patients who underwent TL, preoperative cervical CT images were available that allowed an evaluation of the SMM. We only included patients with an available imaging test 2 months prior to the surgery (median 34.5 days, range 2–61 days); therefore, 6 patients were excluded. We excluded 13 women who underwent a TL during the study period. In total, 86 male patients were included, most of them treated with simple TL (n = 67), extended TL with pharyngectomy without reconstruction (n = 11), and extended TL with pharyngectomy and reconstruction with a pectoralis major flap (n = 8). All eight patients undergoing flap reconstruction had been implanted with a salivary bypass tube.
Surgery was the initial treatment in 43 cases (50.0%), and was salvage treatment in 31 cases (36.0%): 13 (41.9%) after radiotherapy; 2 (6.5%) after surgery and radiotherapy; 13 (41.9%) after chemo-radiotherapy; and 3 (9.7%) after bioradiotherapy. In the remaining 12 cases (14.0%), the surgical indication was resection of a second tumour located in the larynx or hypopharynx of patients previously treated with radiotherapy. Of the 86 included patients, 43 (50.0%) had received radiotherapy prior to surgery, and in 74 patients (86.1%), surgical treatment included neck dissection, unilaterally in 12 cases (14.0%) and bilaterally in 62 cases (72.1%).
All patients received antibiotic prophylaxis, usually with amoxicillin–clavulanic acid: 2 g administered 30 min before surgery, and 1 g administered every 4 h during surgery. Patients allergic to penicillin were administered the combination clindamycin 900 mg + gentamicin 5 mg/kg. Enteral nutrition by nasogastric tube was initiated on the 1st postoperative day. If no wound complications occurred, oral intake was started on the 7th postoperative day in non-irradiated patients, and on the 12th postoperative day in patients who had previously received radiotherapy or undergone pectoralis major flap reconstruction.
Data analysis
A fistula was defined as any clinical suspicion of salivary leak confirmed by oral administration of methylene blue dye. When a PCF was confirmed, the initial treatment was conservative management involving antibiotic therapy, continuation of enteral nutrition, and daily local wound care. In cases that did not respond adequately to conservative management, pectoralis major flap reconstruction was considered on a case-by-case basis [26].
The following patient-related variables were assessed: sex; age; alcohol use; tobacco use; diabetes mellitus; and American Society of Anesthesiologists (ASA) physical status. Patients were classified into 1 of 3 categories according to their use of alcohol and tobacco, as follows: no use; moderate use (< 20 cigarettes/day and/or < 80 g alcohol/day); or heavy use (≥ 20 cigarettes/day or ≥ 80 g alcohol/day). The body mass index (BMI) was calculated for each patient, with patients grouped according to the World Health Organization (WHO) classification [27] as follows: underweight (< 18.5 kg/m2); normo-overweight (18.5–29.9 kg/m2); or obese (> 30 kg/m2). Also evaluated were the following variables: tumour extension and location; previous radiotherapy or chemo-radiotherapy; surgery type; automatic suture use; neck dissection; voice prosthesis placement; preoperative and postoperative haemoglobin levels (according to WHO [28] anaemia criteria); and preoperative albumin and protein levels. Table 1 summarizes the patient characteristics.
CSMA measurements
All images, in Digital Imaging and Communications in Medicine (DICOM) format, were anonymized by a person not involved in the study, for analysis by a single researcher (MC), who had previously received training guided by the Radiodiagnosis Department.
The CSMA was measured from CT or positron emission tomography (PET-CT) images obtained in the 3 months prior to surgery. Images were analysed using Image J (software v1.44p) [29] and Fiji accessories [30]. The axial slice corresponding to C3 was selected following Swartz et al.’s [16] guidelines, i.e., axial C3 slices were scrolled through in the caudo-cranial direction and selected was the first slice that fully showed the vertebral arch, the transverse processes, and the spinous process. The CSMA was evaluated for the prevertebral and nuchal musculature and sternocleidomastoid muscles. In patients with pathological lymph nodes infiltrating part of the musculature to be evaluated, a theoretical line was drawn to delimit the lymph node, and possible infiltrated muscle tissue was excluded as non-viable. The CSMA was defined as the sum of the areas of each muscle bundle (right and left sternocleidomastoid and perivertebral musculature) at the C3 level.
Intraobserver and interobserver validation studies of 10 CT images were based on a repeat analysis and an analysis by a different investigator (CR), respectively. Correlation coefficients were 0.95 or greater for measurements at the C3 level. Figure S1 (supplementary material) shows the correlations obtained in the validation studies.
Statistical analysis
SPSS version 17.0 was used for data analysis. Results were considered to be statistically significant at p < 0.05.
A recursive partitioning analysis (RPA) using the classification and regression tree (CRT) method was used to obtain a cut-off point to categorize the continuous CSMA variable (independent variable) according to PCF formation (dependent variable). Patients with CSMA values below the cut-off obtained with the RPA were considered sarcopenic.
A univariate analysis of PCF formation was performed for each evaluated variable, including the CSMA categories obtained in the RPA, using either the Chi-square test or Fisher’s exact test depending on the application conditions. A multivariate analysis was performed with a logistic regression model, considering PCF as the dependent variable, and the remaining variables as independent variables. We excluded of the multivariate analysis the preoperative albumin and protein levels due to a lack of data for 40 and 42 patients, respectively. The patient who made no use of alcohol or tobacco (n = 1) was included in the moderate alcohol/tobacco use group.
To validate our results, the study was repeated, this time measuring the CSMA at L3 using the Swartz et al. [16] formula and calculating the SMMI.
CSMA values were analysed according to the different clinical variables using the Student’s t test or the analysis of variance (ANOVA) test. Correlation between continuous variables was evaluated using Pearson’s correlation coefficient.
Results
PCF and sarcopenia
A total of 21 patients (24.4%) developed PCFs after TL. Considering PCF formation as the dependent variable, the RPA cut-off point for the CSMA at C3 was 35.5 cm2. According to this threshold value, 18 patients (20.9%) presented low SMM, and of these, 9 patients (50.0%) developed PCFs; of the 68 patients with a normal SMM (79.1%), 12 (17.6%) developed PCFs. The risk of PCF formation was thus 4.67 times greater in low SMM patients than in patients with normal SMM (95% CI 1.53–14.23; p = 0.007).
Table 2 shows the percentage of patients with PCF formation according to the different analysed variables. Apart from the CSMA at C3, tumour location, surgery type, and suture type proved to be significantly related to PCF formation. Thus, PCF frequency was greater for hypopharyngeal tumours (63.6%) than for supraglottic tumours (20.8%) or glottic tumours (17.6%) (p = 0.008); for extended TL with pharyngectomy (52.6%) than for simple TL (16.4%) (p = 0.002); and for manual suture (32.1%) than for automatic suture (10.0%) (p = 0.023).
Table 3 shows the results of the multivariate study, considering PCF formation as the dependent variable and the remaining variables as independent variables. The results show that the CSMA at C3 was the only variable that was significantly associated with PCF risk: the hazard ratio (HR) for PCF formation in patients with a CSMA at C3 of ≤ 35.5 cm2 was 9.88 times greater than for patients with a CSMA at C3 of > 35.5 cm2 (95% CI: 1.40–69.73; p = 0.022).
The study was repeated using the standard Swartz et al. [16] approach to measuring sarcopenia, based on C3-to-L3 conversion of the CSMA and calculating the SMMI by dividing the obtained value by the squared patient height. The RPA cut-off point based on the SMMI value and PCF formation was 47.7 cm2/m2; accordingly, 46.5% (n = 40) of patients had decreased SMM, and of these, 37.5% (n = 15) developed PCFs, compared to 13.0% of 46 patients with normal SMM. PCF risk was 4.00 times greater in patients with low SMM than in patients with normal SMM (95% CI 1.37–11.67; p = 0.011). Table S1 (supplementary material) shows the multivariate analysis results, with the evaluation of SMM according to the SMMI included as an independent variable; as was the case for the CSMA at C3, the only variable that was significantly associated with PCF risk was low SMM. This risk was 8.5 times greater for patients with an SMMI of ≤ 47.7 cm2/m2 than for patients with an SMMI of > 47.7 cm2/m2 (95% CI 1.22–59.36; p = 0.031).
Patients with low SMM
Table 4 shows the proportion of patients with low SMM measured according to the CSMA at C3 for each studied variable. Table S2 (supplementary material) shows values for the CSMA at C3 expressed as the mean (SD) for each variable.
Differences were observed according to BMI, surgery extension, the use of automatic suture, and preoperative anaemia and hypoalbuminemia. As for BMI, the higher the value, the greater the observed CSMA at C3 (p = 0.0001); based on the WHO BMI classification, 87.5% of underweight, 17.5% of normo-overweight, and 0.0% of obese patients were observed to have low SMM (p = 0.0001). Patients with extended surgeries suffered more SMM depletion than patients with simple TL (47.4% versus 13.4%, p = 0.003). In the group of patients in which an automatic suture was used, the prevalence of SMM depletion was lower than in patients sutured manually (3.3% versus 30.4%).
Also, patients with preoperative anaemia presented more risk of low SMM, observed in 38.5% of those patients compared to 13.3% for patients without anaemia (p = 0.009). Even though the available data regarding preoperative albumin levels were limited, 50.0% of patients with values below 35 g/L presented low SMM, while for patients with normal values, it was of 15.6% (p = 0.027). No differences were observed regarding patients with low SMM as a function of previous radiotherapy treatment (p = 0.112).
Discussion
Low SMM prevalence
In our study of the relationship between low SMM and PCF formation after treatment with TL in male patients, SMM was evaluated considering the CSMA calculated from CT slices obtained at the C3 level. We found, on the basis of direct measurement of the CSMA at C3 and a cut-off point of 35.5 cm2, that 20.9% of our patients presented low SMM.
In preliminary phases of this study, we observed that the 13 women in our cohort had lower mean CSMA at C3 values than men (30.22 cm2 vs 41.02 cm2; p = 0.0001) (Figure S2—supplementary material). Given the small number of female patients, it was not possible for us to establish a specific cut-off for women, so we excluded those patients from the study.
Calculating a sex-specific cut-off for men allowed a more restrictive cut-off point to be obtained, which probably is more appropriate for the identification of patients at a higher PCF risk, as, from the perspective of—possibly costly and individualized—prevention, it would seem to be more effective to select a small number of patients at clearly higher risk.
There is little literature on the incidence of SMM depletion determined directly at the C3 level, as the standard procedure is to calculate the SMMI at L3 from measurements made at C3 (the formula proposed by Swartz et al. [16]). However, because C3-to-L3 conversion formulas are complicated to use in routine practice, we evaluated the relationship with sarcopenia of the CSMA measured directly at C3. Jung et al. [21] have demonstrated, for patients with HNSCC, that direct CSMA measurement at C3 is a good predictor of overall survival; however, to our knowledge, no other studies evaluate PCF risk according to this determination of sarcopenia.
Our cut-off point was based on PCF formation. Considering the cut-off points most commonly used in the literature [7, 22], the proportion of our cohort presenting low SMM would be 80.2% according to Prado [22] (cut-offs of 52.4 cm2/m2 for men and 38.5 cm2/m2 for women), but only 22.1% according to Wendrich [7] (a cut-off of 43.2 cm2/m2). Those cut-off values vary greatly, because they were obtained on the basis of different dependent variables. The study by Prado et al. [22], carried out with a cohort of obese patients who had lung or gastrointestinal tract tumours, focused on determining a threshold that would define a significant association between decreased muscle mass and mortality in such patients, while the study by Wendrich et al. [7], performed in patients with HNSCC, aimed at obtaining a cut-off point related to the dose-limiting toxicity of chemotherapy.
Low SMM as a PCF risk factor
Of the 86 patients evaluated in our study, 21 (24.4%) developed PCFs. The univariate analysis showed that low SMM was significantly associated with PCF formation (p = 0.011). Corroborating our results for a previous study [6], the other variables associated with PCF formation were tumour location and surgery type, specifically, hypopharyngeal tumours (p = 0.008) and extended TL with pharyngectomy (p = 0.002), respectively. Suture type was another variable associated with PCF formation in the univariate analysis, as manual suture implied a significant PCF risk. Note, however, that we consider this finding to be a consequence of selection bias, as only patients with endolaryngeal tumours treated with simple TL—with a lower a priori PCF risk [31]—were considered candidates for automatic suture closure.
In line with the findings of other authors [9, 32,33,34,35,36], we found no significant relationship between BMI and PCF risk. However, for their multicentre study, Lansaat et al. [3] reported that the PCF rate was 2.7 times higher in underweight patients (BMI < 18 kg/m2) compared to normal weight patients, and Lebo et al. [1] similarly reported a higher PCF rate for underweight patients. Nonetheless, we agree with Prado et al. [22] argument that, since the BMI does not indicate the composition of each weight unit, the information it provides is incomplete. Exemplifying this argument are the C3 images for two patients in our study shown in Fig. 1: while both patients had the same BMI of 23 kg/m2, on the basis of their CSMA values of 29.4 cm2 (image A) and 43.9 cm2 (image B), they are classifiable as low SMM and normal SMM patients, respectively.
Images at the 3rd cervical vertebra corresponding to 2 patients with the same body mass index of 23 kg/m2. The red areas included in the manually designed yellow regions of interest corresponding to perivertebral musculature (labelled as 1 for nuchal and 2 for prevertebral muscles) and sternocleidomastoid muscles (labelled 3 and 4) are added to obtain the cross-sectional muscle area. The cross-sectional muscle areas of 29.4 cm2 in image A and 44 cm2 in image B would classify the patients as having low skeletal muscle mass and normal skeletal muscle mass, respectively
The multivariate analysis indicated that low SMM was the only variable that was significantly related to PCF risk, 9.88 times greater for patients with a CSMA of ≤ 35.5 cm2 than for patients with a CSMA of > 35.5 cm2 (p = 0.022). When CSMA was included in the multivariate analysis as an independent variable, the relationship that we identified in a previous study [6], namely, between the extent of surgery and PCF risk, no longer held; this finding would indicate that sarcopenia measured directly at C3 is, of the analysed variables, the most important predictor of PCF risk. It should be noted that the cut-off point used in the RPA was obtained specifically considering PCF formation as the dependent variable. The use of the same variable as a determinant cut-off to segregate the sample and as the dependent variable in the multivariate model is subject to bias. Therefore, studies need to be carried out to validate the paper of low SMM in patients treated with a laryngectomy.
Other authors have found SMM depletion to be associated with PCF formation in patients treated with TL [9, 10]. Achim et al. [9] analysed the CSMA at L3 for 70 patients treated with TL, finding that patients with sarcopenia developed 7.5 times more complications than patients without sarcopenia (95% CI 1.56–36.4), and also that PCF incidence was 32% greater in patients with low SMM (95% CI 1.13–1.53). For 235 patients treated with TL, Bril et al. [10] used the cut-off point proposed by Wendrich et al. [7] (43.2 cm2/m2) for CSMA at C3 converted to SMMI at L3, observing that SMM was reduced in 46.4% of cases, and also that patients with low SMM compared to patients with normal muscle mass more frequently developed PCFs (34.9% vs 20.6%; p = 0.02) and more frequently required surgical repair (p = 0.05).
Low SMM incidence as a risk factor for PCF was determined to be equivalent for our direct measurement of the CSMA at C3 and for the standard method of C3-to-L3 conversion and SMMI calculation. Our results would therefore suggest that measurement of the CSMA at C3 is a valid method for evaluating muscle mass, and therefore low SMM, in patients with HNSCC, while having the advantage of being a direct measurement that avoids the use of conversion formulas.
Patients with low SMM
A relationship was observed between BMI and the CSMA at C3. Analysing percentages according to the WHO [27] BMI classification, we observed that low SMM was far more frequent (87.5%) in underweight patients (BMI < 18.5 kg/m2), and no low SMM cases (0.0%) were assessed in obese patients (BMI > 30 kg/m2). Corroborating our results, Cho et al. [37] reported a higher proportion of underweight patients in their depleted SMM group than in their normal SMM group (17% vs 4%; p < 0.001).
We found that the depleted SMM rate was higher in patients with extended surgeries. We attribute this finding to a higher tumour stage that requires complex surgeries including pharyngectomies with or without reconstruction. In turn, we believe that patients with advanced tumour stages present sarcopenia as a reflection of suboptimal nutritional status and tumour-related metabolic changes, such as preoperative anaemia or hypoalbuminemia. The increased rate of low SMM in patients sutured manually might be a consequence to the selection bias occurred, because automatic suture is only performed in patients with endolaryngeal tumours.
The main limitation of our study is that, given its retrospective nature, we were unable to evaluate the impact of certain variables that could influence PCF formation, such as weight loss, a history of tracheotomy [32], or perioperative transfusions [1, 4, 33, 38]. Another important limitation was the reduced number of patients and its heterogeneity in treatment strategy, which may lead to a selection bias. We were also unable to evaluate our patients’ muscle strength, a key aspect of sarcopenia diagnosis according to the EWGSOP [13].
Further studies need to be carried to validate the relationship between the CSMA at C3 and post-TL PCF formation, and to define cut-off points with a greater prognostic capacity.
Conclusions
On the basis of a definition of low SMM associated with PCF formation, 20.9% of our cohort had preoperative SMM depletion as determined from the CSMA at C3. Our multivariate study of risk factors for PCF indicated low SMM to be the only independent risk factor: such patients had a near tenfold increased risk of PCF formation. The fact that measuring the CSMA at C3 obtained results similar to those obtained by calculating the SMMI at L3 would suggest that direct SMM assessment from C3 is a useful approach to evaluating post-TL PCF.
References
Lebo NL, Caulley L, Alsaffar H, Corsten MJ, Johnson-Obaseki S (2017) Peri-operative factors predisposing to pharyngocutaneous fistula after total laryngectomy: analysis of a large multi- institutional patient cohort. J Otolaryngol Head Neck Surg 23:46–54. https://doi.org/10.1186/s40463-017-0233-z
Liang JW, Li ZD, Li SC, Fang FQ, Zhao YJ, Li YG (2015) Pharyngocutaneous fistula after total laryngectomy: a systematic review and meta-analysis of risk factors. Auris Nasus Larynx 42(5):353–359. https://doi.org/10.1016/j.anl.2015.04.002
Lansaat L, van der Noort V, Bernard SE, Eerenstein SEJ, Plaat BEC, Langeveld TAPM, Lacko M, Hilgers FJM, de Bree R, Takes RP, van den Brekel MWM (2018) Predictive factors for pharyngocutaneous fistulization after total laryngectomy: a Dutch Head and Neck Society audit. Eur Arch Otorhinolaryngol 275(3):783–794. https://doi.org/10.1007/s00405-017-4861-8
Dedivitis RA, Aires FT, Cernea CR, Brandão LG (2015) Pharyngocutaneous fistula after total laryngectomy: Systematic review of risk factors. Head Neck 37(11):1691–1697. https://doi.org/10.1002/hed.23804
Hasan Z, Dwivedi RC, Gunaratne DA, Virk SA, Palme CE, Riffat F (2017) Systematic review and meta-analysis of the complications of salvage total laryngectomy. Eur J Surg Oncol 43(1):42–51. https://doi.org/10.1016/j.ejso.2016.05.017
Casasayas M, Sansa A, García-Lorenzo J, López M, Orús C, Peláez X, Quer M, León X (2019) Pharyngocutaneous fistula after total laryngectomy: multivariate analysis of risk factors and a severity-based classification proposal. Eur Arch Oto-Rhino-Laryngol 276(1):143–151. https://doi.org/10.1007/s00405-018-5200-4
Wendrich AW, Swartz JE, Bril SI, Wegner I, De GA, Smid EJ, De BR, Pothen AJ (2017) Low skeletal muscle mass is a predictive factor for chemotherapy dose-limiting toxicity in patients with locally advanced head and neck cancer. Oral Oncol 71:26–33. https://doi.org/10.1016/j.oraloncology.2017.05.012
Bozkurt G, Elhassan HA, Mahmutoğlu AS, Çelebi İ, Mcleod RWJ, Soytaş P, Erol ZN, Sözen E (2018) Neck Muscle Mass Index as a predictor of post-laryngectomy wound complications. Ann Otol Rhinol Laryngol 127(11):841–847. https://doi.org/10.1177/0003489418798660
Achim V, Bash J, Mowery A, Guimaraes AR, Li R, Schindler J, Wax M, Andersen P, Clayburgh D (2017) Prognostic indication of sarcopenia for wound complication. JAMA Otolaryngol Head Neck Surg 143(12):1159–1165. https://doi.org/10.1001/jamaoto.2017.0547
Bril SI, Pezier TF, Tijink BM, Janssen LM, Braunius WW, de Bree R (2019) Preoperative low skeletal muscle mass as a risk factor for pharyngocutaneous fistula and decreased overall survival in patients undergoing total laryngectomy. Head Neck 41(6):1745–1755. https://doi.org/10.1002/hed.25638
Huiskamp LFJ, Chargi N, Devriese LA, de Jong PA, de Bree R (2020) The predictive and prognostic value of low skeletal muscle mass for dose-limiting toxicity and survival in head and neck cancer patients receiving concomitant cetuximab and radiotherapy. Eur Arch Otorhinolaryngol 277(10):2847–2858. https://doi.org/10.1007/s00405-020-05972-2
Willemsen ACH, Hoeben A, Lalisang RI, Van Helvoort A, Wesseling FWR, Hoebers F, Baijens LWJ, Schols AMWJ (2020) Disease-induced and treatment-induced alterations in body composition in locally advanced head and neck squamous cell carcinoma. J Cachexia Sarcopenia Muscle 11(1):145–159. https://doi.org/10.1002/jcsm.12487
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, Schneider SM, Sieber CC, Topinkova E, Vandewoude M, Visser M, Zamboni M, Bautmans I, Baeyens JP, Cesari M, Cherubini A, Kanis J, Maggio M, Martin F, Michel JP, Pitkala K, Reginster JY, Rizzoli R, Sánchez-Rodríguez D, Schols J (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48(1):16–31. https://doi.org/10.1093/ageing/afy169
Chamchod S, Fuller CD, Mohamed ASR, Sc M, Grossberg A, Messer JA, Heukelom J, Gunn GB, Kantor ME, Ba HE, Garden AS, Rosenthal DI (2016) Quantitative body mass characterization before and after head and neck cancer radiotherapy : a challenge of height-weight formulae using computed tomography measurement. Oral Oncol 61:62–69. https://doi.org/10.1016/j.oraloncology.2016.08.012
Jung AR, Roh JL, Kim JS, Kim SB, Choi SH, Nam SY, Kim SY (2019) Prognostic value of body composition on recurrence and survival of advanced-stage head and neck cancer. Eur J Cancer 116:98–106. https://doi.org/10.1016/j.ejca.2019.05.006
Swartz JE, Pothen AJ, Wegner I, Smid EJ, Swart KMA, De BR, Leenen LPH, Grolman W (2016) Feasibility of using head and neck CT imaging to assess skeletal muscle mass in head and neck cancer patients. Oral Oncol 62:28–33. https://doi.org/10.1016/j.oraloncology.2016.09.006
Zwart AT, van der Hoorn A, van Ooijen PMA, Steenbakkers RJHM, de Bock GH, Halmos GB (2019) CT-measured skeletal muscle mass used to assess frailty in patients with head and neck cancer. J Cachexia Sarcopenia Muscle 10(5):1060–1069. https://doi.org/10.1002/jcsm.12443
Chargi N, Bril SI, Emmelot-Vonk MH, de Bree R (2019) Sarcopenia is a prognostic factor for overall survival in elderly patients with head-and-neck cancer. Eur Arch Otorhinolaryngol 276(5):1475–1486. https://doi.org/10.1007/s00405-019-05361-4
Ganju RG, Morse R, Hoover A, Tennapel M, Lominska CE (2019) The impact of sarcopenia on tolerance of radiation and outcome in patients with head and neck cancer receiving chemoradiation. Radiother Oncol 137:117–124. https://doi.org/10.1016/j.radonc.2019.04.023
van Rijn-Dekker MI, van den Bosch L, van den Hoek JGM, Bijl HP, van Aken ESM, van der Hoorn A, Oosting SF, Halmos GB, Witjes MJH, van der Laan HP, Langendijk JA, Steenbakkers RJHM (2020) Impact of sarcopenia on survival and late toxicity in head and neck cancer patients treated with radiotherapy. Radiother Oncol 147:103–110. https://doi.org/10.1016/j.radonc.2020.03.014
Jung AR, Roh JL, Kim JS, Choi SH, Nam SY, Kim SY (2019) Efficacy of head and neck computed tomography for skeletal muscle mass estimation in patients with head and neck cancer. Oral Oncol 95:95–99. https://doi.org/10.1016/j.oraloncology.2019.06.009
Prado CM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, Baracos VE (2008) Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol 9(7):629–635. https://doi.org/10.1016/S1470-2045(08)70153-0
Grossberg A, Chamchod S, Fuller C, Mohamed A, Heukelom J, Eichelberger H, Kantor M, Hutcheson K, Gunn G, Garden A, Frank S, Phan J, Beadle B, Skinner H, Morrison W, Rosenthal D (2016) Association of body composition with survival and locoregional control of radiotherapy-treated head and neck squamous cell carcinoma. JAMA Oncol 2(6):782–789. https://doi.org/10.1001/jamaoncol.2015.6339
Fattouh M, Chang GY, Ow TJ, Shifteh K, Rosenblatt G, Patel VM, Smith RV, Prystowsky MB, Schlecht NF (2020) Association between pretreatment obesity, sarcopenia, and survival in patients with head and neck cancer. Head Neck 41(3):707–714. https://doi.org/10.1002/hed.25420.ASSOCIATION
Stone L, Olson B, Mowery A, Krasnow S, Jiang A, Li R, Schindler J, Wax MK, Andersen P, Marks D, Achim V, Clayburgh D (2019) Association between sarcopenia and mortality in patients undergoing surgical excision of head and neck cancer. JAMA Otolaryngol Head Neck Surg 145(7):647–654. https://doi.org/10.1001/jamaoto.2019.1185
Sumarroca A, Rodríguez-Bauzà E, Lop-Gros J, García J, López M, Quer M, León X (2018) Repair of post-laryngectomy pharyngocutaneous fistulas using a pectoralis major flap. Braz J Otorhinolaryngol 85(3):351–356. https://doi.org/10.1016/j.bjorl.2018.03.002
World Health Organization (2000) Obesity: preventing and managing the global epidemic
World Health Organization (2011) Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System. 2011 (WHO/NMH/NHD/MNM/11.1). http://www.who.int/vmnis/indicators/haemoglobin.pdf (accessed [date])
Schneider CA, Rasband WS, Eliceiri KW (2012) NIH Image to ImageJ: 25 years of image analysis. Nat Methods 9(7):671–675
Schindelin J, Arganda-Carreras I, Frise E, Kaynig V, Longair M, Pietzsch T, Preibisch S, Rueden C, Saalfeld S, Schmid B, Tinevez J-Y, White DJ, Hartenstein V, Eliceiri K, Tomancak P, Cardona A (2012) Fiji: an open-source platform for biological-image analysis. Nat Methods 9:676–682. https://doi.org/10.1038/nmeth.2019
Sansa-Perna A, Casasayas-Plass M, Rovira-Martínez C, López-Vilas M, García-Lorenzo J, Quer-Agusti M, León-Vintró X (2020) Pharyngeal closure after a total laryngectomy: mechanical versus manual technique. J Laryngol Otol 134(7):626–631. https://doi.org/10.1017/S0022215120001371
Benson EM, Hirata RM, Thompson CB, Ha PK, Fakhry C, Saunders JR, Califano JA, Arnaoutakis D, Levine M, Tang M, Neuner G, Messing BP, Blanco RGF (2015) Pharyngocutaneous fistula after total laryngectomy: a single-institution experience, 2001–2012. Am J Otolaryngol Head Neck Med Surg 36(1):24–31. https://doi.org/10.1016/j.amjoto.2014.08.017
Kim DY, Roh JL, Choi JW, Choi SH, Nam SY, Kim SY (2014) Risk factors and survival outcomes for patients with anastomotic leakage after surgery for head and neck squamous cell carcinoma. Clin Exp Otorhinolaryngol 7(1):36–41. https://doi.org/10.3342/ceo.2014.7.1.36
Virtaniemi JA, Kumpulainen EJ, Hirvikoski PP, Johansson RT, Kosma V-M (2001) The incidence and etiology of postlaryngectomy pharyngocutaneous fistulae. Head Neck 23(1):29–33. https://doi.org/10.1002/1097-0347(200101)23:1%3c29::AID-HED5%3e3.0.CO;2-P
Palomar-Asenjo V, Sarroca Capell E, Tobías Gómez S, Pérez Hernández I, Palomar-García V (2008) Pharyngocutaneous fistula following total laryngectomy. A case-control study of risk factors implicated in its onset. Acta Otorrinolaringol Espanola 59(10):480–484
Cavalot AL, Gervasio CF, Nazionale G, Albera R, Bussi M, Staffieri A, Ferrero V, Cortesina G (2000) Pharyngocutaneous fistula as a complication of total laryngectomy: review of the literature and analysis of case records. Otolaryngol Head Neck Surg 123(5):587–592. https://doi.org/10.1067/mhn.2000.110617
Cho Y, Kim JW, Keum KC, Lee CG, Jeung HC (2018) Prognostic significance of sarcopenia with inflammation in patients with head and neck cancer who underwent definitive chemoradiotherapy. Front Oncol 22(8):457. https://doi.org/10.3389/fonc.2018.00457
Erdag MA, Arslanoglu S, Onal K, Songu M, Tuylu AO (2013) Pharyngocutaneous fistula following total laryngectomy: multivariate analysis of risk factors. Eur Arch Otorhinolaryngol 270(1):173–179. https://doi.org/10.1007/s00405-012-2111-7
Funding
Open Access Funding provided by Universitat Autonoma de Barcelona. This work was supported by grants from the State R + D + I Plan of the Instituto de Salud Carlos III (FIS PI19/01661) and European Regional Development Fund (A Way to Build Europe).
Author information
Authors and Affiliations
Contributions
All authors have contributed in the writing or editing of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest to the work submitted for publication.
Availability of data and materials
Data are available from the hospital software, SAP.
Code availability
Not applicable.
Ethics approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional, regional, and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study was authorized by our hospital’s Clinical Research Ethics Committee [reference 19/126 (OBS)].
Informed consent to participate
For this type of study, formal consent was not required.
Consent for publication
For this type of study, formal consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Casasayas, M., García-Lorenzo, J., Gómez-Ansón, B. et al. Low skeletal muscle mass assessed directly from the 3rd cervical vertebra can predict pharyngocutaneous fistula risk after total laryngectomy in the male population. Eur Arch Otorhinolaryngol 279, 853–863 (2022). https://doi.org/10.1007/s00405-021-07127-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-07127-3