Abstract
Purpose
The objective of this study was to compare the efficacy of peritonsillar and glossotonsillar sulcus infiltration with bupivacaine to manage postoperative pain and odynophagia in children undergoing tonsillectomy.
Methods
Fifty children (5–10 years of age) undergoing tonsillectomy due to recurrent tonsillar infections were enrolled in the study and assigned into two groups receiving either pre-incisional peritonsillar (Group 1, n = 25) or glossotonsillar sulcus (Group 2, n = 25) infiltration with 1 mg/kg bupivacaine (0.5%) totaling 5 mL in volume. At different time intervals following arrival to the post-anesthesia care unit (PACU), the participants in each group were evaluated for pain using the modified Children’s Hospital of Eastern Ontario Pain Scale (mCHEOPS) and for odynophagia using a four-point scale (1—none, normal or no difficulty with swallowing, 2—mild, mild difficulty with swallowing, 3—moderate, moderate difficulty with swallowing, and 4—severe, no swallowing or swallowing only with maximal effort). Additional parameters were assessed for 24 h post-surgery, including time to first administration of analgesic, additional analgesic requirements, nausea/vomiting, allergic reaction, and bleeding.
Results
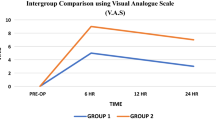
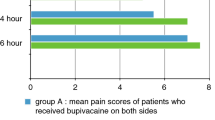
Infiltration of either region with bupivacaine yielded similar analgesic effects at different times following the surgery (P = 0.065). Time to first analgesic treatment and additional analgesic requirements were not significantly different between groups (P = 0.181). Compared to the Group 1, Group 2 was associated with significantly lower odynophagia scores at different times after the surgery (P = 0.020).
Conclusion
Present results indicate that the infiltration of local anesthetics to glossotonsillar sulcus is a safe, practical, and effective pain management intervention without risk of significant side effects for children undergoing tonsillectomy.

Similar content being viewed by others
References
Kasapoglu F, Kaya FN, Tuzemen G, Ozmen OA, Kaya A, Onart S (2011) Comparison of peritonsillarlevobupivacaine and bupivacaine infiltration for post-tonsillectomy pain relief in children: placebo-controlled clinical study. Int J Pediatr Otorhinolaryngol 75:322–326. https://doi.org/10.1016/j.ijporl.2010.11.015
Sun J, Wu X, Meng Y, Jin L (2010) Bupivacaine versus normal saline for relief of post-adenotonsillectomy pain in children: a meta-analysis. Int J PediatrOtorhinolaryngol 74:369–373. https://doi.org/10.1016/j.ijporl.2010.01.004
Wang C, Kundaria S, Fernandez-Miranda J, Duvvuri U (2016) A description of the anatomy of the glossopharyngeal nerve as encountered in transoral surgery. Laryngoscope 126:2010–2015. https://doi.org/10.1002/lary.25706
Lim CM, Mehta V, Chai R, Pinheiro CN, Rath T, Snyderman C, Duvvuri U (2013) Transoral anatomy of the tonsillar fossa and lateral pharyngeal wall: anatomic dissection with radiographic and clinical correlation. Laryngoscope 123:3021–3025. https://doi.org/10.1002/lary.23927
Stelter K, Hempel JM, Berghaus A, Andratschke M, Luebbers CW, Hagedorn H (2009) Application methods of local anaesthetic infiltrations for postoperative pain relief in tonsillectomy: a prospective, randomised, double-blind, clinical trial. Eur Arch Otorhinolaryngol 266:1615–1620. https://doi.org/10.1007/s00405-008-0909-0
Mohamed SK, Ibraheem AS, Abdelraheem MG (2009) Preoperative intravenous dexamethasone combined with glossopharyngeal nerve block: role in pediatric postoperative analgesia following tonsillectomy. Eur Arch Otorhinolaryngol 266:1815–1819. https://doi.org/10.1007/s00405-009-0937-4
Vlok R, Melhuish TM, Chong C, Ryan T, White LD (2017) Adjuncts to local anaesthetics in tonsillectomy: a systematic review and meta-analysis. J Anesth 31:608–616. https://doi.org/10.1007/s00540-017-2310-x
Ju NY, Cui GX, Gao W (2013) Ropivacaine plus dexamethasone infiltration reduces postoperative pain after tonsillectomy and adenoidectomy. Int J Pediatr Otorhinolaryngol 77:1881–1885. https://doi.org/10.1016/j.ijporl.2013.08.037
Karaaslan K, Yilmaz F, Gulcu N, Sarpkaya A, Colak C, Kocoglu H (2008) The effects of levobupivacaine versus levobupivacaine plus magnesium infiltration on postoperative analgesia and laryngospasm in pediatric tonsillectomy patients. Int J Pediatr Otorhinolaryngol 72:675–681. https://doi.org/10.1016/j.ijporl.2008.01.029
Paradise JL, Bluestone CD, Bachman RZ et al (1984) Efficacy of tonsillectomy for recurrent throat infection in severely affected children. Results of parallel randomized and nonrandomized clinical trials. N Engl J Med 310:674–683. https://doi.org/10.1056/NEJM198403153101102
Yenigun A, Et T, Aytac S, Olcay B (2015) Comparison of different administration of ketamine and intravenous tramadol hydrochloride for postoperative pain relief and sedation after pediatric tonsillectomy. J Craniofac Surg 26:21–24. https://doi.org/10.1097/SCS.0000000000001250
Tong Y, Ding XB, Wang X, Ren H, Chen ZX, Li Q (2014) Ketamine peritonsillar infiltration during tonsillectomy in pediatric patients: an updated meta-analysis. Int J Pediatr Otorhinolaryngol 78:1735–1741. https://doi.org/10.1016/j.ijporl.2014.07.036
Unal Y, Pampal K, Korkmaz S, Arslan M, Zengin A, Kurtipek O (2007) Comparison of bupivacaine and ropivacaine on postoperative pain after tonsillectomy in paediatric patients. Int J Pediatr Otorhinolaryngol 71:83–87. https://doi.org/10.1016/j.ijporl.2006.09.005
Maryam H, Amin J, Sedighe V, Vida A (2017) Comparing the effects of peritonsillar infiltration of tramadol before and after the surgery on post-tonsillectomy pain. Eur Arch Otorhinolaryngol 274:2521–2527. https://doi.org/10.1007/s00405-017-4477-z
Grainger J, Saravanappa N (2008) Local anaesthetic for post-tonsillectomy pain: a systematic review and meta-analysis. Clin Otolaryngol 33:411–419. https://doi.org/10.1111/j.1749-4486.2008.01815.x
Molliex S, Haond P, Baylot D, Prades JM, Navez M, Elkhoury Z, Auboyer C (1996) Effect of pre- vs postoperative tonsillar infiltration with local anesthetics on postoperative pain after tonsillectomy. Acta Anaesthesiol Scand 40:1210–1215. https://doi.org/10.1111/j.1399-6576.1996.tb05552.x
Park HP, Hwang JW, Park SH, Jeon YT, Bahk JH, Oh YS (2007) The effects of glossopharyngeal nerve block on postoperative pain relief after tonsillectomy: the importance of the extent of obtunded gag reflex as a clinical indicator. Anesth Analg 105:267–271. https://doi.org/10.1213/01.ane.0000266440.62424.f1
Dahi-Taleghani M, Mousavifard S, Tahmoureszade S, Dabbagh A (2011) Rectal acetaminophen versus peritonsillar infiltration of bupivacaine for postoperative analgesia after adenotonsillectomy in children. Eur Arch Otorhinolaryngol 268:581–584. https://doi.org/10.1007/s00405-010-1434-5
Nikandish R, Maghsoodi B, Khademi S, Motazedian S, Kaboodkhani R (2008) Peritonsillar infiltration with bupivacaine and pethidine for relief of post-tonsillectomy pain: a randomised double-blind study. Anaesthesia 63:20–25. https://doi.org/10.1111/j.1365-2044.2007.05283.x
Weksler N, Nash M, Rozentsveig V, Schwartz JA, Schily M, Gurman GM (2001) Vocal cord paralysis as a consequence of peritonsillar infiltration with bupivacaine. Acta AnaesthesiolScand 45:1042–1044. https://doi.org/10.1034/j.1399-6576.2001.450820.x
Shlizerman L, Ashkenazi D (2005) Peripheral facial nerve paralysis after peritonsillar infiltration of bupivacaine: a case report. Am J Otolaryngol 26:406–407. https://doi.org/10.1016/j.amjoto.2005.02.019
Acknowledgements
We would like to thank our colleagues and the nursing staff at Adana City Training and Research Hospital, Adana, Turkey, for their cooperation and timely help.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethical approval
The study was conducted and completed in accordance with the ethical principles outlined in the Declaration of Helsinki and was approved by the Ethics Committee of Adana City Training and Research Hospital in Adana, Turkey (19-KAEK-382). Written informed consent was obtained from the parent or legal guardian of each participant following a detailed explanation of the study protocol and risks and benefits of participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yücel Ekici, N., Özdoğan, H. Comparing local anesthetic infiltration of the peritonsillar region and glossotonsillar sulcus for post-tonsillectomy pain management. Eur Arch Otorhinolaryngol 277, 255–260 (2020). https://doi.org/10.1007/s00405-019-05668-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05668-2