Abstract
Purpose
To investigate the correlation between the time to locoregional recurrence and survival in T1–T2 oropharyngeal squamous-cell carcinoma (OPSCC) patients.
Methods
A retrospective, single-site study of patients with T1–T2 OPSCC treated with curative intent between 2000 and 2015 who had a locoregional recurrence without distant metastases. Patients without a disease-free interval (i.e., persistent macroscopic disease after the end of treatment and a time to locoregional recurrence of less than 3 months) were excluded. The endpoint considered was overall survival (OS).
Results
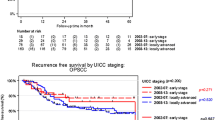
Out of 602 T1–T2 OPSCC patients, 121 patients had a locoregional recurrence and they were, hence, analyzed. All of the patients were heavy-smokers, with a consumption of more than 20 pack-years. The recurrence was local in 59.5%, regional in 27.3%, and both local and regional in 13.2% of the patients. The median time to locoregional recurrence and median OS was 15 months and 44 months, respectively. The time to locoregional recurrence was correlated with OS (p < 0.0001). In multivariate analyses, factors associated with survival were an initial N0–N2a versus N2b–N3 nodal staging and a 12-month threshold for the time to locoregional recurrence.
Conclusions
Locoregional control in T1–T2 OPSCC is not only a qualitative prognostic factor but also a quantitative prognostic factor of survival. A time to locoregional recurrence of less than 12 months was correlated with an unfavorable prognosis.



Similar content being viewed by others
References
Hunter KD, Parkinson EK, Harrison PR (2005) Profiling early head and neck cancer. Nat Rev Cancer 5(2):127–135. https://doi.org/10.1038/nrc1549
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68(1):7–30. https://doi.org/10.3322/caac.21442
Khalid MB, Ting P, Pai A, Russo JL, Bakst R, Chai RL, Teng MS, Genden EM, Miles BA (2018) Initial presentation of human papillomavirus-related head and neck cancer: a retrospective review. Laryngoscope. https://doi.org/10.1002/lary.27296
Turner MT, Byrd JK, Ferris RL (2016) Current role of surgery in the management of oropharyngeal cancer. J Oncol Pract 12(11):1176–1183. https://doi.org/10.1200/JOP.2016.015263
Chen AY, Zhu J, Fedewa S (2014) Temporal trends in oropharyngeal cancer treatment and survival: 1998–2009. Laryngoscope 124(1):131–138. https://doi.org/10.1002/lary.24296
Goodwin WJ (2000) Salvage surgery for patients with recurrent squamous cell carcinoma of the upper aerodigestive tract: when do the ends justify the means?. Laryngoscope 110(93):1–18. https://doi.org/10.1097/00005537-200003001-00001
Agra IM, Carvalho AL, Pontes E, Campos OD, Ulbrich FS, Magrin J, Kowalski LP (2003) Postoperative complications after en bloc salvage surgery for head and neck cancer. Arch Otolaryngol Head Neck Surg 129(12):1317–1321. https://doi.org/10.1001/archotol.129.12.1317
Kostrzewa JP, Lancaster WP, Iseli TA, Desmond RA, Carroll WR, Rosenthal EL (2010) Outcomes of salvage surgery with free flap reconstruction for recurrent oral and oropharyngeal cancer. Laryngoscope 120(2):267–272. https://doi.org/10.1002/lary.20743
Philouze P, Peron J, Poupart M, Pujo K, Buiret G, Ceruse P (2017) Salvage surgery for oropharyngeal squamous cell carcinomas: a retrospective study from 2005 to 2013. Head Neck 39(9):1744–1750. https://doi.org/10.1002/hed.24827
Jayaram SC, Muzaffar SJ, Ahmed I, Dhanda J, Paleri V, Mehanna H (2016) Efficacy, outcomes, and complication rates of different surgical and nonsurgical treatment modalities for recurrent/residual oropharyngeal carcinoma: a systematic review and meta-analysis. Head Neck 38(12):1855–1861. https://doi.org/10.1002/hed.24531
Kao SS, Ooi EH (2018) Survival outcomes following salvage surgery for oropharyngeal squamous cell carcinoma: systematic review. J Laryngol Otol 132(4):299–313. https://doi.org/10.1017/S0022215117000998
Agra IM, Carvalho AL, Ulbrich FS, de Campos OD, Martins EP, Magrin J, Kowalski LP (2006) Prognostic factors in salvage surgery for recurrent oral and oropharyngeal cancer. Head Neck 28(2):107–113. https://doi.org/10.1002/hed.20309
Zafereo ME, Hanasono MM, Rosenthal DI, Sturgis EM, Lewin JS, Roberts DB, Weber RS (2009) The role of salvage surgery in patients with recurrent squamous cell carcinoma of the oropharynx. Cancer 115(24):5723–5733. https://doi.org/10.1002/cncr.24595
Kim J, Kim S, Albergotti WG, Choi PA, Kaplan DJ, Abberbock S, Johnson JT, Gildener-Leapman N (2015) Selection of ideal candidates for surgical salvage of head and neck squamous cell carcinoma: effect of the Charlson-Age Comorbidity Index and oncologic characteristics on 1-year survival and hospital course. JAMA Otolaryngol Head Neck Surg 141(12):1059–1065. https://doi.org/10.1001/jamaoto.2015.2158
Hamoir M, Holvoet E, Ambroise J, Lengele B, Schmitz S (2017) Salvage surgery in recurrent head and neck squamous cell carcinoma: oncologic outcome and predictors of disease-free survival. Oral Oncol 67:1–9. https://doi.org/10.1016/j.oraloncology.2017.01.008
Stell PM (1991) Time to recurrence of squamous cell carcinoma of the head and neck. Head Neck 13(4):277–281
Liu SA, Wong YK, Lin JC, Poon CK, Tung KC, Tsai WC (2007) Impact of recurrence interval on survival of oral cavity squamous cell carcinoma patients after local relapse. Otolaryngol Head Neck Surg 136(1):112–118. https://doi.org/10.1016/j.otohns.2006.07.002
Ho AS, Kraus DH, Ganly I, Lee NY, Shah JP, Morris LG (2014) Decision making in the management of recurrent head and neck cancer. Head Neck 36(1):144–151. https://doi.org/10.1002/hed.23227
Omura G, Saito Y, Ando M, Kobayashi K, Ebihara Y, Yamasoba T, Asakage T (2014) Salvage surgery for local residual or recurrent pharyngeal cancer after radiotherapy or chemoradiotherapy. Laryngoscope 124(9):2075–2080. https://doi.org/10.1002/lary.24695
Lacau St Guily J, Rousseau A, Baujat B, Perie S, Schultz P, Barry B, Dufour X, Malard O, Pretet JL, Clavel C, Birembaut P, Franceschi S, Papillophar G (2017) Oropharyngeal cancer prognosis by tumour HPV status in France: the multicentric Papillophar study. Oral Oncol 67:29–36. https://doi.org/10.1016/j.oraloncology.2017.01.012
Huang SH, Xu W, Waldron J, Siu L, Shen X, Tong L, Ringash J, Bayley A, Kim J, Hope A, Cho J, Giuliani M, Hansen A, Irish J, Gilbert R, Gullane P, Perez-Ordonez B, Weinreb I, Liu FF, O’Sullivan B (2015) Refining American Joint Committee on Cancer/Union for International Cancer Control TNM stage and prognostic groups for human papillomavirus-related oropharyngeal carcinomas. J Clin Oncol 33(8):836–845. https://doi.org/10.1200/JCO.2014.58.6412
Liskamp CP, Janssens GO, Bussink J, Melchers WJ, Kaanders JH, Verhoef CG (2016) Adverse effect of smoking on prognosis in human papillomavirus-associated oropharyngeal carcinoma. Head Neck 38(12):1780–1787. https://doi.org/10.1002/hed.24516
Hong AM, Martin A, Chatfield M, Jones D, Zhang M, Armstrong B, Lee CS, Harnett G, Milross C, Clark J, Elliott M, Smee R, Corry J, Liu C, Porceddu S, Rees G, Rose B (2013) Human papillomavirus, smoking status and outcomes in tonsillar squamous cell carcinoma. Int J Cancer 132(12):2748–2754. https://doi.org/10.1002/ijc.27956
Maxwell JH, Kumar B, Feng FY, Worden FP, Lee JS, Eisbruch A, Wolf GT, Prince ME, Moyer JS, Teknos TN, Chepeha DB, McHugh JB, Urba SG, Stoerker J, Walline HM, Kurnit DM, Cordell KG, Davis SJ, Ward PD, Bradford CR, Carey TE (2010) Tobacco use in human papillomavirus-positive advanced oropharynx cancer patients related to increased risk of distant metastases and tumor recurrence. Clin Cancer Res 16(4):1226–1235. https://doi.org/10.1158/1078-0432.CCR-09-2350
Lin BM, Wang H, D’Souza G, Zhang Z, Fakhry C, Joseph AW, Drake VE, Sanguineti G, Westra WH, Pai SI (2013) Long-term prognosis and risk factors among patients with HPV-associated oropharyngeal squamous cell carcinoma. Cancer 119(19):3462–3471. https://doi.org/10.1002/cncr.28250
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Formal consent for participation has been given by patients.
Rights and permissions
About this article
Cite this article
Caula, A., Boukhris, M., Guerlain, J. et al. Correlation between the duration of locoregional control and survival in T1–T2 oropharyngeal cancer patients. Eur Arch Otorhinolaryngol 276, 1161–1166 (2019). https://doi.org/10.1007/s00405-019-05293-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05293-z