Abstract
Free-flap mandibular reconstruction is a highly specialized procedure associated with severe complications necessitating re-interventions and re-hospitalizations. This surgery is expensive in terms of health workers’ time, equipment, medical devices and drugs. Our main objective was to assess the direct hospital cost generated by osseocutaneous free-flap surgery in a multicentric prospective micro-costing study. Direct medical costs evaluated from a hospital perspective were assessed using a micro-costing method from the first consultation with the surgeon until the patient returns home, thus confirming the success or failure of the free-flap procedure. The mean total cost for free-flap intervention was 34,009€ (5151–119,604€), the most expensive item being the duration of hospital bed occupation, representing 30–90% of the total cost. In the event of complications, the mean cost increased by 77.3%, due primarily to hospitalization in ICU and the conventional unit. This surgery is effective and provides good results but remains highly complex and costly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mandibular reconstruction aimed at optimizing function, esthetics and quality of life for patients remains a technical challenge for reconstructive surgeons. Since it was introduced in the late 1960s, osseocutaneous free tissue transfer with titanium plate fixation and microvascularisation has become the gold standard for reconstruction of maxillary and mandibular defects [1–3]. These advances have dramatically changed the approach to, and expectations of, patients afflicted with benign and malignant pathologies affecting the mandible, as well as the palatomaxillary complex [1]. In addition, dental rehabilitation with osseointegrated implants can restore functional mastication, which positively impacts patients’ acceptance of such damaging surgery [2, 4]. Free-flaps have been shown to be reliable, with success rates in the literature approaching 95% [5, 6]. In cancer patients, this reconstruction approach is an effective therapeutic option providing satisfactory overall and specific survival and good tumor control rates and functional outcomes [5, 7]. Moreover, quality of life in such patients is satisfactory in most cases, even after extensive ablative surgery. However, this surgery is complex with an often long and costly operative course [8]. Mandibular reconstruction requires a long surgical procedure by a highly specialized double team and surveillance in the recovery ward or intensive care unit; also, it can be associated with severe complications requiring re-interventions and re-admissions. Inevitably, the cost in terms of health workers, equipment, medical devices and drugs is very high [9]. Our main objective was to assess the direct hospital cost generated by osseocutaneous free-flap surgery in a multicentric prospective micro-costing study.
Patients and methods
Eligibility criteria
Eligibility criteria were as follows: patients aged between 18 and 75 years needing mandibular free-flap reconstruction (fibular, scapular or iliac crest free-flap) for advanced buccopharyngeal cancer; mandibular osteoradionecrosis or mandibular destructive benign tumor; performance status <3, ASA score <4.
Trial design
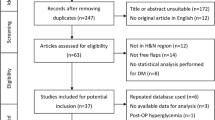
Direct medical costs from diagnosis to initial or re-intervention surgical procedures were estimated using a micro-costing approach. Patients’ clinical pathways for free-flap intervention are described in Fig. 1. Health-care resources for economic assessment were evaluated from a hospital perspective. Costs were calculated by the micro-costing method from the first consultation with the surgeon until the patient returns home, thus confirming the success or failure of the free-flap procedure. Direct medical costs were identified using observational field work and extensive consultations with experienced local medical and surgical staff. The initial field workflow involved interviews with surgeons, anesthetists, chemotherapists, pathologists, radiologists, biologists, pharmacists, nurses and administrative staff designed to determine the items and quantities consumed. Data regarding patients’ clinical pathway, hospital stay, imaging, status of staff (salary data and working time) and all individual items, equipment and drugs were then collated to generate the final aggregated unit costs. For each selected item, all quantities, unit prices and durations were collected where necessary. Costs of adjuvant treatment (radiotherapy, chemotherapy, hormonotherapy) were not included.
Cost evaluation
For each patient, the following items were included in the costing: consultations by specialist physicians, bone and vascular imaging, general information about the main intervention and subsequent re-interventions for immediate and late postoperative complications, operative-room occupation time, type of free-flap (fibular, scapular or iliac crest free-flap), personnel involved (surgeons, anesthetists, operating-room nurses, anesthetists, nurses, students and others), cumulated time (minutes), expensive surgical devices (plates, screws, prostheses, wires, pliers, clamps, catheters), expensive consumables, pre- and post-surgical hospitalization (standard follow-up or more complex follow-up including re-intervention for complications) and type of units and duration of stay.
All fixed costs used in this study are presented in Table 1. The cost of a consultation with a specialist physician is €23. This price is fixed by the French National Health Insurance authorities. Costs of bone or vascular imaging are also fixed by the French National Health Insurance bodies. Personal costs per hour and expensive surgical device costs were provided by the hospital administration by taking the mean cost of all healthcare workers and of equipment, including taxes and fees. In addition, Raft et al. recently showed that indirect operating theater expenses represent 20% of the total expenditure, i.e. about 2€ per minute. This was the figure we used to calculate indirect operating theater expenses in this study [10]. These indirect costs include expenses involved in biomedical engineering, sterilization, pharmacy (drugs), general administrative services, human resource services, hotel service, housekeeping, financial and building structure) [10].
Data management
After an exhaustive inventory of all the data involved in free-flap surgery costs, the clinical data manager of the study devised an electronic case-report form designed to recover all data as soon as possible after the surgical intervention and as close as possible to the real cost, as well as all other clinical, medical and cost-related information relevant to the study.
Statistical analysis
Costs and quantitative data were described by means, standard deviations, medians and ranges. Qualitative data were described by absolute and relative percentages. Each item was evaluated using 2015 prices. All cost data were calculated in Euros. No equipment depreciation was calculated. All statistical analyses were performed using R-3.1.3 for Windows.
Ethical approval
This clinical trial was conducted according to the study protocol, which was approved by the French Comité consultatif sur le traitement de l’information en matière de recherché médicale (C.C.T.I.R.S.) and by our local ethical comitee. All participants provided written informed consent.
Results
Patient characteristics
From February 2009 to September 2011, 108 patients were prospectively included and treated in the 11 French participating centers. The characteristics of included patients are summarized in Table 2. Most patients had fibula free-flap (85%); other patients had iliac or scapular free-flap. More than two-thirds of the patients were male. Most patients had complicating co-morbidities (73%) such as tobacco, alcohol intoxication, cardio-vascular problems or diabetes. Patients showed a good performance status; 20% had an ASA score of 3. Sixty-seven percent of patients had malignant tumor and more than 90% had pT > 2. Twenty percent of patients showed tumor relapse and 25% a radio-necrosis.
Cost before initial intervention
Table 3 shows the number of consultations performed by the patient’s physician and the cost of these consultations before the initial surgery. The mean number of consultation was 5 [SD = 2; range (2–13)] corresponding to an average of 115 € per patient [SD = 43; range (46–299)]. Table 4 shows the number of imaging procedures per patient, with an average of 2 [SD = 1; range (1–7)] for bone imaging and a average of 1 [SD = 1; range (0–4)] for vascular imaging. These procedures represent a mean total cost per patient of 366€ [SD = 168; range (97–966)] for both bone and vascular imaging.
Cost for initial intervention and re-intervention
Table 5 shows duration and cost of the initial free-flap surgery. Nurses and surgeons are the most costly items of expenditure with an average cost of 1651€ and 1519€, respectively. Mean anesthetist cost amounted to 966€ followed by 118€ for nursing assistants. Total hospital staff spending for initial free-flap surgery represented a mean cost of 4112€ [SD: 1258; range (1637–7880)]. The mean total cost per patient for expensive surgical disposable equipment (plates, microplates, screws, wires, clamps, probes, conical drills, prostheses, etc.) was 997€ [SD: 541; range (2–3082)] and 166€ [SD: 152; range (35–334)] for initial intervention and re-intervention, respectively. Thirty-seven patients (34.2%) presented complications after initial surgery; 12 patients (11.1%) presented immediate complications, most of them anastomotic or hemorrhagic (bleeding, thrombosis, hematoma); 31 patients (28.7%) presented late complications including sepsis, partial or total necrosis and complications at bone donor site. Twenty-two patients (20.4%) needed only one re-intervention, and 15 (13.9%) required more than one re-intervention for immediate or late complications with a maximum of five interventions for one patient. Table 6 shows duration and cost of re-intervention for immediate and late complications. Spending on surgeons, anesthetists and nurses showed a mean total of 330€ [SD: 401/range (49–1711)], 349€ [SD: 380/range (32–1659)] and 496€ [SD: 520/range (93–2396)], respectively. An additional 49€ were needed [SD: 58/range (6–190)] for nursing assistants. Mean total expenditure for surgical hospital staff in re-interventions for compromised free-flaps amounted to 1170€ [SD: 1204/range (219–5360)].
Cost for hospitalization
Table 7 shows the length of hospitalization per patient before and after initial intervention and after re-intervention. All patients had hospital stays in conventional units before initial surgery for pre-surgical assessment or immediate preoperative hospitalization for a median of 1.0 day (range 1–35). After initial free-flap intervention, patients spent an average 7.0 days in ICU and 18.0 days in conventional units. After re-intervention for immediate or late complications, patients were re-hospitalized for an average 18.0 days in ICU and 22.0 days in conventional units. Free-flap intervention failed in 14/108 patients (13.0%).
Total cost
In summary, Table 8 shows all analyzed costs in Euros for free-flap surgery. Most of the costs were due to hospitalization in ICUs or conventional units and break down as follows: 4.7% before surgery, 30.77% for post-operative care and 53.07% for immediate and late complications. Figure 2 shows the total cost per patient of a free-flap intervention. Mean total cost was 34,009€ (±24,354€) and median total cost was 27,452€, ranging from 5151 to 119,604€. Of the 108 analyzed patients, the mean cost for initial free-flap intervention was 26,147€ (±11,756) with a median of 25,024, ranging from 4305 to 64,338€. Mean re-intervention cost amounted to 20,217€ (±23,434) with a median of 11,978 ranging from 94 to 100,937€.
Discussion
The clinical efficacy and the complications of mandibular reconstruction and microsurgery are well established. Some authors have reported free-flap success percentages over 95% following careful patient selection [2]. The main goal is to improve, where necessary, patients’ overall and disease-free survival [7]. Secondary objectives are to reestablish the shape of the lower third of the face and to restore functional activities [1]. Complications and postoperative outcomes are also fully described in the scientific literature [5]. Although the clinical and therapeutic aspects of this specific surgical technique are well-documented, cost evaluation has not been performed as thoroughly. Reconstructive microsurgery is very costly and there is a need to justify this use of resources [11]. In France, these procedures are usually performed in non-profit institutions and treatment is entirely financed by the French National Health Insurance system. Our study analyzes only direct hospital costs related to the pre-surgical and post-surgical period and shows that the mean total cost for free-flap intervention was 34,009€ (5151 to 119,604€) and that the major component of resource costs was the hospital bed, which accounted for 30–90% of the total cost. Mean initial intervention costs amounted to 26,147€ (4305 to 64,338€) including five hospitalization days in ICU and 16 days in a conventional unit. However, this cost increased by an average of 20,217€ (94 to 100,937€), or 77.3% of the initial cost, due to immediate and late complications (37 patients, 34.2%), giving rise primarily to more days in ICU (16 extra days) or a conventional unit (14 extra days). In a retrospective study using a very similar calculation to ours, Miller et al. [12] reported an average cost for all patients of 27,000$ with a mean 16 days’ hospital stay (range, 7600–63,000$, 4–30 days). The average cost for aerodigestive tract tumor was 37,400$ with 21 days’ hospitalization. Complications occurred in 28% of cases with 90% happening in aerodigestive tract tumors treated by free-flaps. They showed an average cost of 25,100$ with 10 days’ hospitalization for patients without complications and a cost of 46,400$ with 23 days’ hospitalization for patients with complications resulting in an 85% increase. Another retrospective study by Jones et al. [13] showed an average cost per patient of 35,000$ with the hospital stay constituting a major item. In this latter study, the cost of a patient with no complication was 28,700$ and this cost reached 49,000$ when complications occurred, resulting in a 70.7% increase in the total resource costs, due primarily to an increase in the component resource costs of the ICU. Another study published by Kroll et al. [14] evaluated on 89 patients the cost of head and neck reconstruction using radial forearm free-flap. They calculated a mean cost of 29,397$ (±8894) including a mean hospital stay of 13.3 days (±5.6) and a failure rate of 4.5%. The estimated time in the operating room was calculated at 10.63 h (±1.99). In the present study, it was evaluated at 9.95 h (±2.1).
In our series, we demonstrate that the increase of the average cost per patient stems essentially from complications leading to increased length of hospitalization stay. Several risk factors related to complications have been identified by authors [15]. In order to reduce the cost of mandibular free-flap reconstruction, hospital teams endeavor to increase the success of the procedure and eliminate the risk of local or general complications. We have shown that the most frequent local complications were surgical site infections, flap necrosis, salivary fistulas and hematomas and the most frequent general complications were neuropathy, cardiovascular complications and urinary infection. At the donor site, postoperative complications consisted in infections, hematomas and split thickness skin graft partial losses [5, 8, 16]. Some complication risk factors such as smoking/drinking, nutrition and appropriate reconstructive design and technique can be controlled but certain factors such as patient age and other comorbidities escape control. In addition, it is essential to have a well-trained team from the surgeon performing the microsurgery and the anesthetist to the staff in charge of post-operative care or flap monitoring [15]. Various authors have made further proposals designed to reduce costs associated with microsurgical reconstruction. Jones et al. [13] suggested selection of a very reliable donor flap and synchronous harvesting of the flap by a second team to reduce overall operative time. Careful preoperative assessment of the American Society of Anesthesiologists score can help identify those patients in need of more aggressive postoperative attention. Reduction of the duration of ventilator support can lessen the risk of pulmonary complications. In addition, it is important to transfer the patient as early as possible from the ICU to a standard care unit without compromising flap monitoring or pulmonary care. Tracheostomy decannulation and speech and swallowing therapy could also enable earlier patient discharge. Haddock et al. [17] also suggested improved nursing training and the use of standardized postoperative protocols allowing patients to be monitored postoperatively in non-ICU settings, thereby reducing the costs associated with providing postoperative microsurgical care. Some authors have also shown that the costs incurred in microvascular reconstruction are related to the type and site of the reconstruction, patient comorbidities and also the experience of the physician [13, 15, 18, 19]. Kroll et al. [14] demonstrated that the total resource cost was significantly related to age and ASA status but not to tumor stage, presence of tumor recurrence or preoperative irradiation. Lin et al. [20] showed that high-volume surgeons performing free-flap operations for oral cancer reconstruction incurred significantly lower costs per patient than low-volume surgeons. Complex head and neck reconstruction, redefined by advances in microsurgical technology, is now the treatment of choice for complex head and neck defects [21]. These procedures are laborious, complex and expensive; hence, it is important to compare their cost with the potential improvement in terms of patient quality of life, including functional status, psychological well-being and return to work. Recently, we evaluated long-term quality of life and its predictive factors after oncologic surgery and microvascular reconstruction [2]. Mean time between surgery and quality of life assessment was about 6 years and the percentage of free-flap failures was ~9% due to the clinical characteristics of the patients (high comorbidity levels, tobacco and irradiation). The EORTC QLQ-C30 and EORTC QLQ-H&N35 questionnaires showed patients to be satisfied with 70% global quality of life score and a mean function score of 82.5%, associated with few general symptoms other than fatigue and insomnia. Regarding specific head and neck symptoms, patients had swallowing problems, difficulties with eating in public, restricted mouth opening, dental problems and salivary dysfunction, especially in irradiated patients. Sixty percent of these patients continued working after surgery and 30% of them required changes in their working conditions (shorter working hours and/or qualitative changes). The fixed costs used in our study were calculated as accurately as possible, although certain limiting factors such as missing data or uncollected data might have affected the accuracy of our results. Also, resource costs in the French institutions involved in this study are not necessarily the same as those in other hospitals or countries. Our data reflect the institutional situation only and do not include indirect or social costs.
References
Bak M, Jacobson AS, Buchbinder D, Urken ML (2010) Contemporary reconstruction of the mandible. Oral Oncol 46(2):71–76
Pierre CS, Dassonville O, Chamorey E et al (2014) Long-term quality of life and its predictive factors after oncologic surgery and microvascular reconstruction in patients with oral or oropharyngeal cancer. Eur Arch Otorhinolaryngol 271(4):801–807
Urken ML (2003) Advances in head and neck reconstruction. Laryngoscope 113(9):1473–1476
Pierre CS, Dassonville O, Chamorey E et al (2014) Long-term functional outcomes and quality of life after oncologic surgery and microvascular reconstruction in patients with oral or oropharyngeal cancer. Acta Otolaryngol 134(10):1086–1093
Bozec A, Poissonnet G, Chamorey E et al (2009) Radical ablative surgery and radial forearm free flap (RFFF) reconstruction for patients with oral or oropharyngeal cancer: postoperative outcomes and oncologic and functional results. Acta Otolaryngol 129(6):681–687
Disa JJ, Pusic AL, Hidalgo DH, Cordeiro PG (2001) Simplifying microvascular head and neck reconstruction: a rational approach to donor site selection. Ann Plast Surg 47(4):385–389
Nao EE, Dassonville O, Poissonnet G et al (2011) Ablative surgery and free flap reconstruction for elderly patients with oral or oropharyngeal cancer: oncologic and functional outcomes. Acta Otolaryngol 131(10):1104–1109
Nao EEM, Dassonville O, Chamorey E et al (2011) Head and neck free-flap reconstruction in the elderly. Eur Ann Otorhinolaryngol Head Neck Dis 128(2):47–51
Baujat B, Altabaa K, Meyers M, Wagner I, Leclerc C, Chabolle F (2011) Medicoeconomic study of microsurgical head and neck reconstructions. Eur Ann Otorhinolaryngol Head Neck Dis 128(3):121–126
Raft J, Millet F, Meistelman C (2015) Example of cost calculations for an operating room and a post-anaesthesia care unit. Anaesth Crit Care Pain Med 34(4):211–215
de Bree R, Reith R, Quak JJ, Uyl-de Groot CA, van Agthoven M, Leemans CR (2007) Free radial forearm flap versus pectoralis major myocutaneous flap reconstruction of oral and oropharyngeal defects: a cost analysis. Clin Otolaryngol 32(4):275–282
Miller MJ, Swartz WM, Miller RH, Harvey JM (1991) Cost analysis of microsurgical reconstruction in the head and neck. J Surg Oncol 46(4):230–234
Jones NF, Jarrahy R, Song JI, Kaufman MR, Markowitz B (2007) Postoperative medical complications–not microsurgical complications–negatively influence the morbidity, mortality, and true costs after microsurgical reconstruction for head and neck cancer. Plast Reconstr Surg 119(7):2053–2060
Kroll SS, Evans GR, Goldberg D et al (1997) A comparison of resource costs for head and neck reconstruction with free and pectoralis major flaps. Plast Reconstr Surg 99(5):1282–1286
Setala L, Koskenvuori H, Gudaviciene D, Berg L, Mustonen P (2009) Cost analysis of 109 microsurgical reconstructions and flap monitoring with microdialysis. J Reconstr Microsurg 25(9):521–526
Dassonville O, Poissonnet G, Chamorey E et al (2008) Head and neck reconstruction with free flaps: a report on 213 cases. Eur Arch Otorhinolaryngol 265(1):85–95
Haddock NT, Gobble RM, Levine JP (2010) More consistent postoperative care and monitoring can reduce costs following microvascular free flap reconstruction. J Reconstr Microsurg 26(7):435–439
Heinz TR, Cowper PA, Levin LS (1999) Microsurgery costs and outcome. Plast Reconstr Surg 104(1):89–96
Petruzzelli GJ, Brockenbrough JM, Vandevender D, Creech SD (2002) The influence of reconstructive modality on cost of care in head and neck oncologic surgery. Arch Otolaryngol Head Neck Surg 128(12):1377–1380
Lin CS, Lee HC, Lin CT, Lin HC (2008) The association between surgeon case volume and hospitalization costs in free flap oral cancer reconstruction operations. Plast Reconstr Surg 122(1):133–139
Momeni A, Kattan A, Lee GK (2012) Is microsurgical head and neck reconstruction profitable?: analysis at an academic medical center. Ann Plast Surg 68(4):401–403
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was conducted according to the study protocol, which was approved by the French Comité consultatif sur le traitement de l’information en matière de recherche médicale (C.C.T.I.R.S.) and by our local ethical committee.
Informed consent
All participants provided written informed consent.
Funding
This study was funded by the French National Cancer Institute (InCA, campagne PHRC-STIC 2007).
Conflict of interest
The authors have no conflict of interest to disclose.
Rights and permissions
About this article
Cite this article
Dassonville, O., Bozec, A., Château, Y. et al. Multicenter prospective micro-costing study evaluating mandibular free-flap reconstruction. Eur Arch Otorhinolaryngol 274, 1103–1111 (2017). https://doi.org/10.1007/s00405-016-4360-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4360-3