Abstract
Background
The standard procedure most frequently used for ovarian tissue cryopreservation (OTC) is slow freezing, while vitrification has been proposed as promising alternative and has built an impressive catalog of success in fertility laboratories regarding cryopreservation of oocytes and embryos.
Methods
We developed and evaluated a high-throughput protocol for vitrification of human ovarian tissue suitable for clinical processing. Follicular viability was assessed via calcein staining prior and after cryopreservation analyzing ovarian tissue of a cohort of 30 patients.
Results
We found no significant differences regarding follicular viability between slow frozen and vitrified cortex tissue samples 24 h after thawing and rapid warming. Follicular viability of thawed and rapid warmed samples was not significantly different in comparison to fresh samples, indicating high proportions of follicular survival rates with both methods.
Conclusions
High-throughput vitrification is a promising option in a clinical setting. More research is required to determine the status of other tissue-specific quality indicators potentially influencing on autotransplantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In summary, our results indicate that rapid vertical vitrification of ovarian tissue may be equivalent to slow freezing in terms of follicular viability while offering a cost efficient alternative to conventional slow freezing procedures. |
Introduction
Cryopreservation of human oocytes and embryos is a well-established routine method. In many IVF clinics, slow freezing has been superseded by vitrification due to superior survival rates [1,2,3,4] accompanied by considerable technical simplification. Additionally, with slow frozen cells, it was shown that applying rapid warming gives superior results compared to standard thawing protocols in terms of survival rates [5,6,7]. Preservation of oocytes and ovarian tissue cryopreservation (OTC) are two options for fertility protection in female cancer patients [8,9,10]. Multiple working groups have reported pregnancies and live births after thawing and transplantation of cryopreserved ovarian tissue, substantiating that OTC is a promising alternate method of fertility protection [11,12,13,14,15,16,17,18,19]. The large majority of OTC data are based on the slow freezing method, that is regarded as well established [20]. Vitrification of ovarian tissue is a promising alternative method with potential major advantages [21,22,23,24,25]. However, the number of reports about pregnancies and live births after retransplantation of vitrified ovarian tissue is still limited [20, 26]. The majority of centers performing OTC use the slow freezing method while the optimal protocol regarding vitrification of ovarian tissue has yet to be determined.
Methods
Ethics
Ethics committee of University Hospital Bonn approved this study (007/09) including the use of 10% of the ovarian tissue for patient related research and quality control analysis. Written, informed consent was obtained individually from each patient.
Statistics
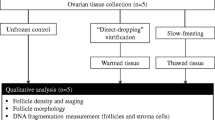
Data were analyzed with SPSS version 25 (IBM) statistical software. Wilcoxon test was used to compare parameters between related samples. Mann–Whitney U test was conducted to determine parameters between groups. Data were tested for normal distribution with Kolmogorov–Smirnov test (Fig. 1).
Ovarian tissue
Ovarian tissue was obtained from 30 patients aged 14–41 (Ø 26.7) years prior cryopreservation for fertility protection measures.
Preparation of material for vitrification
Metal cell meshes (Merck, Darmstadt) with opening sizes of 380 µm were customized to 25 × 8 mm stripes (Fig. 2A). Devices were placed in a sterilization container (Fig. 2B, Euronda Eurobox) prior autoclaving (Tuttnauer, Breda, Netherlands) under humid heat [27, 28] to sterilize the meshes prior further processing. Customized stripes were linked under validated sterile laminar air flow conditions (Kendro Hera Safe) with the caps of 1.8 ml cryovials (Thermo Scientific, Waltham, USA) to obtain thermally conductive loading devices (Fig. 2C).
Surgical retrieval and tissue preparation for cryopreservation
Ovarian tissue was surgically removed prior initiation of gonadotoxic cancer treatment or due to a disease that causes premature limitation of the ovarian reserve. Excision of ovarian tissue was performed laparoscopically in an outpatient surgery. Ovarian tissue resection was performed with sharp scissors without any electrocoagulation to protect oocytes. 30–50% (Fig. 3A) of one ovary was resected. Directly after removal, the tissue was transferred to a tube with custodiol solution (Dr. Köhler, Bensheim, Germany) at 4 °C and forwarded to the lab without deviation. A small part of the tissue was conserved in formalin solution and sent to histopathology to investigate for abnormalities, especially for cancer metastases. After ablation of the medulla (Fig. 3B), cortex was processed in stripes measuring 10 × 5 × 1 mm (Fig. 3C, D) under validated sterile laminar air flow conditions to ensure the highest level of safety and quality accompanying the manufacturing process. Cortex preparation was performed in custodiol (Dr. Köhler, Bensheim, Germany) at 4 °C. Additionally, 2 × 2 mm biopsy punches (pfm medical, Köln, Germany) were prepared for standardized viability measurement pre cryopreservation and post thawing/rapid warming. Cryopreservation was defined as exposition of prepared tissue to cryoprotective agents (CPA) and completion of cooling procedure before storing the samples in the cryobank.
Decontamination of liquid nitrogen
Liquid nitrogen was sterilized according to established protocols [29,30,31]. In brief, nitrogen was exposed to UV irradiation at 254 nm (OSRAM Germicidial Puritec, Berlin, Germany) at a distance of 20 cm for 20 min under a validated laminar flow bench.
Vitrification
Vitrification and rapid warming media was prepared according to Suzuki and colleagues with modifications [26]. In brief, tissue was equilibrated in GMOPS + (Vitrolife, Göteborg, Sweden) supplemented with 10% serum substitute supplement [SSS] (Fujifilm Irvine scientific, Santa Ana, USA) and 10% ethyleneglycol (Merck, Darmstadt, Germany) for 5 min (step 1), followed by equilibration in GMOPS + (Vitrolife, Sweden) supplemented with 10% SSS (Fujifilm Irvine scientific, Santa Ana, USA) and 20% ethyleneglycol (Merck, Darmstadt, Germany) for 5 min (step 2). Finally, samples were transferred to GMOPS + (Vitrolife, Göteborg, Sweden) supplemented with 10% SSS (Fujifilm Irvine scientific, Santa Ana, USA), 35% ethyleneglycol (Merck, Darmstadt, Germany), 5% polyvinylpyrrolidone [PVP] (Merck, Darmstadt, Germany) and 0.5 mol/L sucrose (Merck, Darmstadt, Germany) [step 3]. After 6 min and within 7 min, tissue pieces were placed on the loading device (Fig. 4A, B), surplus liquid was dabbed away with sterile cellulose material. Samples were vertically plunged in cryovials pre-filled with liquid nitrogen (Fig. 4D) in a setting prepared for high throughput, arranged on a loading grid within a customized cryo dewar vessel (Fig. 4C, Eppendorf, Hamburg, Germany). Equilibration steps 1–3 were performed in a 6-well dish (Sarstedt, Germany) with 5 ml media/well on a rocking shaker at room temperature under validated sterile laminar air flow conditions (Kendro Hera Safe, Heraeus).
Rapid warming
Cryovials were placed on a floater (Fig. 5A) in a dewar vessel filled with liquid nitrogen. Vials were opened cautiously (Fig. 5B) and metal meshes with cortex strips were submerged (Fig. 5C) rapidly in 30 ml of prewarmed (37.2 °C) GMOPS + (Vitrolife, Göteborg, Sweden) media supplemented with 0.8 mol/l sucrose (Merck, Darmstadt, Germany) and 10% SSS (Fujifilm Irvine scientific, Santa Ana, USA) for 1 min (step 1) followed by incubation in GMOPS + (Vitrolife, Göteborg, Sweden) media supplemented with 0.4 mol/l sucrose (Merck, Darmstadt, Germany) and 10% SSS (Fujifilm Irvine scientific, Santa Ana, USA) for 3 min (step 2). Finally, 2 washing steps (steps 3–4) with GMOPS + (Vitrolife, Göteborg, Sweden) supplemented with 10% SSS (Fujifilm Irvine scientific, Santa Ana, USA) for 5 min each were conducted. Warming steps 1–4 were performed under validated sterile laminar air flow conditions. Step 1 was performed in a prewarmed sterile cup (Sarstedt, Nümbrecht) at 37.2 °C on a heating plate, while steps 2–4 were conducted in a 6-well dish (Sarstedt, Nümbrecht, Germany) with 5 ml media/well on a rocking shaker (Fig. 5D) at room temperature.
Slow freezing and thawing
Cryopreservation and thawing of cortex samples were performed according to established protocols with modifications [32–37]. In brief, tissue samples were incubated in L-15 Leibovitz’s medium (Gibco Life technologies, NY, U.S.A.) supplemented with 11% human serum albumin [HSA] (Irvine Scientific, Santa Ana, USA), 10% dimethyl sulfoxide [DMSO] (CryoSure DMSO, WAK Chemie, Steinbach, Germany) and equilibrated for 35 min prior slow freezing procedure. Cortex samples were transferred to 1.8 ml vials (Nunc, Thermo Fisher Scientific, Denmark) and cryopreserved with a cooling rate of − 2 °C per min. After seeding, samples were cooled at a rate of − 0.3 °C per min to − 40 °C and at − 10 °C per min to − 140 °C. For thawing, tissue samples were brought to room temperature for 40 s and kept in a water bath for 130 s at 37.2 °C. Transfer of tissue was conducted in 15-min steps to 3 thawing solutions of decreasing sucrose concentrations based on Dulbecco’s phosphate buffered saline [DPBS] (DPBS CTS, Gibco Life technologies, NY, U.S.A.) supplemented with 11% HSA (Irvine Scientific, Santa Ana, USA) prior 2 washing intervals.
Determination of follicular viability
Calcein AM (Merck, Darmstadt, Germany) was dissolved with DMSO (Cryosure DMSO, WAK Chemie, Steinbach, Germany. Follicular viability was determined 24 h after tissue preparation and thawing/rapid warming. Prealiquoted calcein (Merck, Darmstadt, Germany) was dissolved with prewarmed DPBS CTS (Gibco Life technologies, NY, U.S.A.) and transferred to prealiquoted collagenase type 1A (Merck, Darmstadt, Germany) to obtain a viability working solution of 2 µmol/l calcein AM and 1 mg/ml collagenase type 1A. 2 × 2 mm biopsy punches were added to 500 µl of viability working solution and incubated for 90 min at 37.2 °C, protected from light. The solution was resuspended cautiously after 60 and 70 min to enable evenly bottoming of follicles prior fluorescence measurements at room temperature. Number of vital follicles was determined with fluorescence microscopy (Nikon, Ti2, Düsseldorf) as indicated in Fig. 6.
Viability staining of ovarian cortex samples after digestion with collagenase. Viable follicles can be identified by a layer of granulosa cells enclosing the oocyte emitting green fluorescence (495 nm) and by their size difference to stroma cells (A, B). Picture with tenfold (A) magnification displaying viable follicles. Zoomed in section of A with 4 viable follicles (B) at 20-fold magnification. Scalebar 100 µm
Results
In all treatment groups, follicular viability was not normally distributed. As indicated in Table 1, thawing results were statistically not significant comparing thawed slow frozen and rapid warmed vitrified samples. High follicular survival rates were obtained with both cryopreservation methods, resulting in statistically non-significant differences in comparison to fresh samples, data shown in Tables 2, 3. Cryopreservation was significantly less time consuming with vitrification compared to slow freezing as indicated in Table 4. In the fresh group and in the thawed after slow freezing group, 2 different cases with absent follicular viability were observed, while in the rapid warmed after vitrification group no samples with absence of follicular viability were detected.
Discussion
The aim of our study was to design and validate a high-throughput vitrification approach for human ovarian tissue based on the successful protocol of Suzuki and colleagues reporting two deliveries [26].
The technical advantage of the vitrification procedure is avoidance of ice crystal formation contrary to conventional freezing approaches [38,39,40]. The avoidance of ice crystal formation prevents the cellular damage, which can otherwise impair tissue integrity or even follicular survival.
Our results indicate that follicular viability rates are comparable to our standard slow freezing approach, suitable for a clinical application As a carrier system, we used cell meshes consisting of metal, linked with caps of 1.8 ml cryovials, suitable for fast loading of tissue fragments prior rapid vertical vitrification in grid embedded cryovials resulting in a high-throughput process. This is important, because in a clinical laboratory application, the amount of tissue and the numbers of tissue fragments for cryopreservation may variate substantially per patient. Processing time per each fragment is critical to minimize prolonged exposition to a high ratio of cryoprotectants in the final step of equilibration solution—resembling the vitrification process of oocytes, pronuclear (PN) stages or embryos. Additionally, the use of meshes may provide faster cooling rates compared to plastic based systems and can be sterilized by autoclavation. Our system is universally applicable for cortex stripes measuring 10 × 5 × 1 mm and for biopsy punches measuring 2 × 2 mm.
The protocol of Suzuki includes a carrier system consisting of four fine stainless needles linked with the cap of a cryogenic vial, before immersion into liquid nitrogen and insertion into cryovials after vitrification [26].
Partially, our handling approach resembles the protocol of Nikiforov, using unlinked metal meshes for carrying ovarian tissue samples with 0.28 mm wire diameter and mesh aperture of 1.31 mm for vitrification and insertion into cryovials after vitrification [41].
Our approach included metal meshes with wire diameters of 0.25 mm and opening sizes of 0.38 mm. This ensures a large contact area of the cortex tissue on a metal carrier as thin as possible, potentially influencing the thermal conductivity while the meshes were pre linked with the caps of the cryovials. This enables the use of grid embedded cryovials, pre-filled with liquid nitrogen ready for fast vertical insertion of loaded meshes into the cryovials directly during the process of vitrification. This results in a standardized, high-throughput vitrification process of ovarian cortex tissue.
One major key aspect to assess the quality of ovarian cortex tissue is follicular viability that can be evaluated with calcein, a well-described fluorescence-based live assay [42,43,44]. The incubation period of 24 h prior viability measurements of fresh, slow frozen/thawed and vitrified/rapid warmed tissue enables the tissue to express potential damage that could potentially occur with these procedures and may potentially not be observed when analyzed at an earlier stage. The different types of cell death can take minutes to hours [45] and might become visible later than directly after thawing/rapid warming.
Using 2 × 2 mm biopsy samples for evaluation of follicular viability provides valuable, but limited insights due to the fact that follicular density is unevenly [46,47,48] distributed in the human ovary potentially influencing the results. As indicated by our results, in the rapid warmed after vitrification group, no cases with absent follicular viability were observed while in the fresh and thawed after slow freezing groups 2 different samples with absence of follicular vitality were detected. To minimize these effects, a cohort of 30 patients with individual determination of follicular viability prior cryopreservation, post slow freezing and vitrification was evaluated by two experienced embryologists to mitigate researcher specific bias. In a clinical setting, preparation of at least 2 × 2 mm biopsy samples for individual quality control assessment prior and post freezing is recommended.
The design of our experimental setup is limited by the fact that the amount of tissue per patient variates substantially and our ethical vote restricts research to 10% of the amount of tissue, reflecting the limited access of researchers to ovarian tissue in a routine setting [49]. It will be interesting to investigate other tissue-specific quality markers with potential impact on implantation success like angiopoietic factors after tissue culture in a future study with a larger sample number and selected patients with larger amounts of ovarian tissue available for research purposes.
In terms of economical parameters, our results implicate that vitrification is less cost demanding regarding cryopreservation time that can have a major impact on personnel deployment planning—keeping in mind that in a busy cryobank ovarian tissue from external referrer centers scheduled for, e.g., overnight transportation [50] may occasionally arrive on the next day late in the afternoon during the week, or on saturdays, prior, e.g., a slow freezing process lasting for several hours.
Contrary to vitrification, the time consuming slow freezing cooling process must not be interrupted due to potential technical errors related with the programmable freezer unit, computer or software malfunctions and continuous nitrogen supply that could have a major impact on tissue integrity.
Additionally, slow freezing is cost intensive regarding purchasing and maintenance of equipment like controlled freezing systems with an attached nitrogen supply tank, personal computer, freezing software and requires in contrast to vitrification security of electricity during the cooling procedure.
In summary, our results indicate that rapid vertical vitrification of ovarian tissue may be equivalent to slow freezing in terms of follicular viability while offering a cost-efficient alternative to conventional slow freezing procedures. We follow the argumentation of Suzuki [26], Keros [51], Sugishita [52], Silver [53] and Nikiforov [41] that vitrification of ovarian tissue is a promising alternate approach to conventional slow freezing systems for ovarian tissue.
References
Rezazadeh Valojerdi M, Eftekhari-Yazdi P, Karimian L, Hassani F, Movaghar B (2009) Vitrification versus slow freezing gives excellent survival, post warming embryo morphology and pregnancy outcomes for human cleaved embryos. J Assist Reprod Genet 26(6):347–354
Setti PEL, Porcu E, Patrizio P, Vigiliano V, de Luca R, d’Aloja P, Spoletini R, Scaravelli G (2014) Human oocyte cryopreservation with slow freezing versus vitrification results from the National Italian registry data, 2007–2011. Fertil Steril 102(1):90–95
Glujovsky D, Riestra B, Sueldo C, Fiszbajn G, Repping S, Nodar F, Papier S, Ciapponi A (2014) Vitrification versus slow freezing for women undergoing oocyte cryopreservation. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD010047.pub2
Abdel Hafeza FF, Desai N, Abou-Settab AM, Falconea T, Goldfarb J (2010) Slow freezing, vitrification and ultra-rapid freezing of human embryos: a systematic review and meta-analysis. Reprod BioMed Online 20(2):209–222
Parmegiani L, Minasi MG, Arnone A, Casciani V, Cognigni GE, Viñoles R, Varricchio MT, Quintero LA, Greco E, Filicori M (2020) Universal warming protocol for vitrified oocytes to streamline cell exchange for transnational donation programs: a multi-center study. J Assist Reprod Genet 37(6):1379–1385. https://doi.org/10.1007/s10815-020-01798-3 (Epub 2020 May 3 PMID: 32363563)
Parmegiani L, Beilby KH, Arnone A, Bernardi S, Maccarini AM, Nardi E, Cognigni GE, Filicori MJ (2018) Testing the efficacy and efficiency of a single “universal warming protocol” for vitrified human embryos: prospective randomized controlled trial and retrospective longitudinal cohort study. Assist Reprod Genet 35(10):1887–1895. https://doi.org/10.1007/s10815-018-1276-4 (Epub 2018 Aug 3. PMID: 30074129 Free PMC article. Clinical Trial)
Parmegiani L, Tatone C, Cognigni GE, Bernardi S, Troilo E, Arnone A, Maccarini AM, Di Emidio G, Vitti M, Filicori M (2014) Rapid warming increases survival of slow-frozen sibling oocytes: a step towards a single warming procedure irrespective of the freezing protocol? Reprod Biomed Online 28(5):614–623. https://doi.org/10.1016/j.rbmo.2014.01.015 (Epub 2014 Feb 11 PMID: 24657075)
Jadoul P, Guilmain A, Squifflet J, Luyckx M, Votino R, Wyns C, Dolmans MM (2017) Efficacy of ovarian tissue cryopreservation for fertility preservation: lessons learned from 545 cases. Hum Reprod 32(5):1046–1054
Wallace WH, Kelsey TW, Anderson RA (2016) Fertility preservation in pre-pubertal girls with cancer: the role of ovarian tissue cryopreservation. Fertil Steril 105(1):6–12. https://www.fertstert.org/article/S0015-0282(15)02125-1/fulltext
Kim S, Lee Y, Lee S, Kim T (2018) Ovarian tissue cryopreservation and transplantation in patients with cancer. Obstet Gynecol Sci 61(4):431–442
Donnez J, Dolmans MM, Demylle D et al (2004) Livebirth after orthotopic transplantation of cryopreserved ovarian tissue. Lancet 364:1405–1410
Meirow D, Levron J, Eldar-Geva T et al (2005) Pregnancy after transplantation of cryopreserved ovarian tissue in a patient with ovarian failure after chemotherapy. N Engl J Med 353:318–321
Donnez J, Dolmans MM, Pellicer A et al (2015) Fertility preservation for age-related fertility decline. Lancet 385:506–507
Van der Ven H, Liebenthron J, Beckmann M et al (2016) Ninety-five orthotopic transplantations in 74 women of ovarian tissue after cytotoxic treatment in a fertility preservation network: tissue activity, pregnancy and delivery rates. Hum Reprod 31:2031–2041
Meirow D, Ra’anani H, Shapira M et al (2016) Transplantations of frozen-thawed ovarian tissue demonstrate high reproductive performance and the need to revise restrictive criteria. Fertil Steril 106:467–474
Rodriguez-Wallberg KA, Tanbo T, Tinkanen H et al (2016) Ovarian tissue cryopreservation and transplantation among alternatives for fertility preservation in the Nordic countries—compilation of 20 years of multicenter experience. Acta Obstet Gynecol Scand 95:1015–1026
Jensen AK, Macklon KT, Fedder J, Ernst E, Humaidan P, Andersen CY (2017) 86 Successful births and 9 ongoing pregnancies worldwide in women transplanted with frozen-thawed ovarian tissue: focus on birth and perinatal outcome in 40 of these children. J Assist Reprod Genet 34:325–336
Donnez J, Dolmans M-M (2017) Fertility preservation in women. N Engl J Med 377:1657–1665
Hoekman EJ, Louwe LA, Rooijers M, van der Lucette Westerlaken AJ, Klijn NF, Pilgram GSK, de Kroon CD, Carina Hilders GJM. (2019) Ovarian tissue cryopreservation: low usage rates and high live‐birth rate after transplantation. Acta Obstet Gynecol Scand 00:1–9
Anderson RA, Amant F, Braat D, D’Angelo A, de Sousa Lopes SMC, Demeestere I, Dwek S, Frith L, Lambertini M, Maslin C, Moura-Ramos M, Nogueira D, Rodriguez-Wallberg K, Vermeulen N, The ESHRE Guideline Group on Female Fertility Preservation (2020) ESHRE guideline: female fertility preservation. Hum Reprod Open 2020(4):hoaa52
Shi Q, Xie Y, Wang Y, Li S (2017) Vitrification versus slow freezing for human ovarian tissue cryopreservation: a systematic review and meta-anlaysis. Sci Rep 7:8538
Wang Y, Xiao Z, Li L, Fan W, Li SW (2008) Novel needle immersed vitrification: a practical and convenient method with potential advantages in mouse and human ovarian tissue cryopreservation. Hum Reprod 23:2256–2265
Xiao Z, Wang Y, Li L, Luo S, Li SW (2010) Needle immersed vitrification can lower the concentration of cryoprotectant in human ovarian tissue cryopreservation. Fertil Steril 94:2323–2328
Keros V et al (2009) Vitrification versus controlled-rate freezing in cryopreservation of human ovarian tissue. Hum Reprod 24:1670–1683
Fabbri R et al (2014) Good preservation of stromal cells and no apoptosis in human ovarian tissue after vitrification. Biomed Res Int 2014:673537
Suzuki N, Yoshioka N, Takae S, Sugishita Y, Tamura M, Hashimoto S, Morimoto Y, Kawamura K (2015) Successful fertility preservation following ovarian tissue vitrification in patients with primary ovarian insufficiency. Hum Reprod 30(3):608–615
Qiu Q-Q, Sun W-Q, Connor J (2011) Sterilization of biomaterials of synthetic and biological origin. In: Ducheyne P, Healy KE, Hutmacher DW, Grainger DW, Kirkpatrick CJ (eds) Comprehensive biomaterials, vol 4. Elsevier, Amsterdam, pp 127–144
Panta G, Richardson AK, Shaw IC (2019) Effectiveness of autoclaving in sterilizing reusable medical devices in healthcare facilities. J Infect Dev Ctries 13(10):858–864
Parmegiani L, Accorsi A, Cognigni GE, Bernardi S, Troilo E, Filicori M (2010) Sterilization of liquid nitrogen with ultraviolet irradiation for safe vitrification of human oocytes or embryos. Fertil Steril 94(4):1525–1528
Gerba CP, Gramos DM, Nwachuku N (2002) Comparative inactivation of enteroviruses and adenovirus 2 by UV light. Appl Env Microbiol 68:5167–5169
Srikanth B. (1995) The basic benefits of ultraviolet technology. Water Cond Purif 26–27
Gosden RG, Baird DT, Wade JC, Webb R (1994) Restoration of fertility to oophorectomized sheep by ovarian autografts stored at −196° C. Hum Reprod 9(4):597–603. https://doi.org/10.1093/oxfordjournals.humrep.a138556
Isachenko V, Isachenko E, Reinsberg J, Montag M, van der Ven K, Dorn C, Roesing B, van der Ven H (2007) Cryopreservation of human ovarian tissue: comparison of rapid and conventional freezing. Cryobiology 55:261–268
Fabbri R, Venturoli S, D’Errico A, Iannascoli C, Gabusi E, Valeri B, Seracchioli R, Grigioni WF (2003) Ovarian tissue banking and fertility preservation in cancer patients: histological and immunohistochemical evaluation. Gynecol Oncol 89:259–266
Martinez-Madrid B, Dolmans M-M, Van Langendonckt A, Defrère S, Donnez J (2004) Freeze-thawing intact human ovary with its vascular pedicle with a passive cooling device. Fertil Steril 82(5):1390–1394
Leonel ECR, Lucci CM, Amorim CA (2019) Cryopreservation of human ovarian tissue: a review. Transfus Med Hemother 46:173–181
Liebenthron J, Montag M, Reinsberg J, Köster M, Isachenko V, van der Ven K, van der Ven H, Krüssel J-S, von Wolff M (2019) Overnight ovarian tissue transportation for centralized cryobanking: a feasible option. RBMO 38(5):740–749
Amorim CA, Curaba M, Van Langendonckt A, Dolmans M-M, Donnez J (2011) Vitrification as an alternative means of cryopreserving ovarian tissue. Reprod BioMed Online 23:160–186
Fahy GM (1986) Vitrification: a new approach to organ cryopreservation. In: Meryman HT (ed) Transplantation: approaches to graft rejection. Alan R. Liss, New York, USA, pp 305–335
Liebermann J, Nawroth F, Isachenko V, Isachenko E, Rahimi G, Tucker MJ (2002) Potential importance of vitrification in reproductive medicine. Biol Reprod 67:1671–1680
Nikiforov D, Russo V, Nardinocchi D, Bernabò N, Mattioli M, Barboni B (2018) Innovative multi-protectoral approach increases survival rate after vitrification of ovarian tissue and isolated follicles with improved results in comparison with conventional method. J Ovarian Res 11(1):65. https://doi.org/10.1186/s13048-018-0437-5
Schallmoser A, Einenkel R, Färber C et al (2022) In vitro growth (IVG) of human ovarian follicles in frozen thawed ovarian cortex tissue culture supplemented with follicular fluid under hypoxic conditions. Arch Gynecol Obstet. https://doi.org/10.1007/s00404-022-06672-4
Neri S, Mariani E, Meneghetti A, Cattini L, Facchini A (2001) Calcein-acetyoxymethyl cytotoxicity assay: standardization of a method allowing additional analyses on recovered effector cells and supernatants. Clin Diagn Lab Immunol 6:1131–1135
Liebenthron J, Reinsberg J, van der Ven K, Saenger N, Kruessel J-S, Von Wolff M (2019) Serum anti-Müllerian hormone concentration and follicle density throughout reproductive life and in different diseases—implications in fertility preservation. Human Reprod 34(12):2513–2522
Saraste A, Pulkki K (2000) Morphologic and biochemical hallmarks of apoptosis. Cardiovasc Res 45(3):528–537
Schmidt KLT, Byskov AG, Nyboe Andersen A, Müller J, Yding Andersen C (2003) Density and distribution of primordial follicles in single pieces of cortex from 21 patients and in individual pieces of cortex from three entire human ovaries. Human Reprod 18(6):1158–1164
Qu J, Godin PA, Nisolle M, Donnez J (2000) Distribution and epidermal growth factor receptor expression of primordial follicles in human ovarian tissue before and after cryopreservation. Hum Reprod 15:302–310
Kohl J, Dittrich R, Siebzehnrübl E, Wildt L (2000) Determination of follicle numbers in human ovarian biopsies ± a method for estimation of outcome of ovarian cryopreservation. Fertil Steril 74(Suppl 1):212
Smitz J, Dolmans MM, Donnez J, Fortune JE, Hovatta O, Jewgenow K, Picton HM, Plancha C, Shea LD, Stouffer RL, Telfer EE, Woodruff TK, Zelinski MB (2010) Current achievements and future research directions in ovarian tissue culture, in vitro follicle development and transplantation: implications for fertility preservation. Human Reprod Update 16(4):395–414
de Vilela JMV, Dolmans M-M, Amorim CA (2021) Ovarian tissue transportation: a systematic review. Reprod Biomed Online 42(2):351–365
Keros V, Xella S, Hultenby K, Pettersson K, Sheikhi M, Volpe A, Hreinsson J, Hovatta O (2009) Vitrification versus controlled-rate freezing in cryopreservation of human ovarian tissue. Hum Reprod 24(7):1670–1683
Sugishita Y, Taylan E, Kawahara T, Shahmurzada B, Suzuki N, Oktay K (2021) Comparison of open and a novel closed vitrification system with slow freezing for human ovarian tissue cryopreservation. J Assist Reprod Genet 38:2723–2733
Silber SJ, De Rosa M, Goldsmith S, Fan Y, Castleman L, Melnick J (2018) Cryopreservation and transplantation of ovarian tissue: results from one center in the USA. J Assist Reprod Genet 35(12):2205–2213
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
AS designed the study and was involved in thawing, processing of the samples, viability tests, writing and revision of the manuscript and interpretation of the results. Approval of the ethics committee. RE was involved in viability tests, writing and revision of the manuscript and interpretation of the results. CF processing of the samples, viability tests, writing and revision of the manuscript and interpretation of the results. NE was involved in writing and revision of the manuscript and interpretation of the results. JJ was involved in writing and revision of the manuscript and interpretation of the results. NS funded the study, supervised the project, contributed to the design of the study, manuscript writing, revision and final approvement.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have not disclosed any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schallmoser, A., Einenkel, R., Färber, C. et al. The effect of high-throughput vitrification of human ovarian cortex tissue on follicular viability: a promising alternative to conventional slow freezing?. Arch Gynecol Obstet 307, 591–599 (2023). https://doi.org/10.1007/s00404-022-06797-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06797-6