Abstract
Purpose
To evaluate the efficacy of intrauterine inflated Cook Cervical Ripening Balloon (ICRB) in postpartum hemorrhage (PPH) management and fertility preserving for placenta accreta spectrum disorders with placenta previa (previa PAS).
Methods
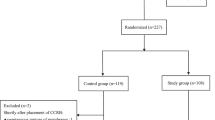
At a tertiary referral center, 74 patients suffering with previa PAS were entered into this retrospective cohort study from January, 2016 to December, 2020, and were confirmed intraoperatively that abnormal invasive placenta reaches the cervical internal ostium and the upper part of the cervical canal. In control group (n = 39), the combination of infrarenal abdominal aorta balloon occlusion (IAABO) and longitudinal parallel compression suture to lower uterine segment were performed. In study group (n = 35), in addition to the aforementioned surgical techniques, ICRB was implemented at the cervical internal ostium and the outside of the cervix simultaneously.
Results
Use of ICRB significantly reduced the rate of peripartum hysterectomy (2.9% vs 30.4%, p = 0.001), and associated with a reduction in surgical time and duration of IAABO (mean 172.7 min vs 206.6 min, p = 0.017; median 30 min vs 40 min, p < 0.001). Use of ICRB significantly reduced the estimated amount of blood loss (median 2500 ml vs 4000 ml, p < 0.001), amounts of packed red blood cells and fresh–frozen plasma transfusion (median 6 U vs 13.5 U, p < 0.001; median 450 ml vs 1200 ml, p < 0.001), postoperative hospital stay and the incidence of oligomenorrhea postoperatively (median 5 days vs 6 days, p = 0.009; 13.8% vs 61.1% p = 0.001). No significant difference was observed between both the groups regarding the use of cryo and PLT, injury of urinary system, relaparotomy, admission to the ICU, postpartum hematocele in uterine cavity, and postoperative complications (including incidence rate of DVT, incidence rate of femoral thrombosis, puerperal morbidity, intrauterine infection, surgical site infection, and deep tissue infection).
Conclusion
ICRB was a simple, effective procedure for PPH management and fertility preserving in some previa PAS cases in which abnormal invasive placenta reaches the cervical internal ostium and the upper part of the cervical canal, in tandem with IAABO and compression suture.




Similar content being viewed by others
References
Jauniaux E, Chantraine F, Silver RM et al (2018) FIGO consensus guidelines on placenta accreta spectrum disorders: epidemiology. Int J Gynaecol Obstet 140(3):265–273
Zeng C, Yang M, Ding Y et al (2018) Placenta accreta spectrum disorder trends in the context of the universal two-child policy in China and the risk of hysterectomy. Int J Gynaecol Obstet 140(3):312–318
Li HT, Hellerstein S, Zhou YB et al (2020) Trends in cesarean delivery rates in China, 2008–2018. JAMA 323(1):89–91
Jauniaux E, Burton GJ (2018) Pathophysiology of placenta accreta spectrum disorders: a review of current findings. Clin Obstet Gynecol 61:743–754
Jauniaux E, Collins SL, Burton GJ (2018) Placenta accreta spectrum: Pathophysiology and evidence-based anatomy for prenatal ultrasound imaging. Am J Obstet Gynecol 218:75–87
Ogawa K, Jwa SC, Morisaki N et al (2021) Risk factors and clinical outcomes for placenta accreta spectrum with or without placenta previa. Arch Gynecol Obstet. https://doi.org/10.1007/s00404-021-06189-2
Fonseca A, Ayres de Campos D (2020) Maternal morbidity and mortality due to placenta accreta spectrum disorders. Best Pract Res Clin Obstet Gynaecol 20: S1521–6934(20)30121–8.
Michelet D, Ricbourg A, Gosme C et al (2015) Emergency hysterectomy for life-threatening postpartum haemorrhage: risk factors and psychological impact. Gynecol Obstet Fertil 43:773e9
Piñas-Carrillo A, Chandraharan E (2020) Conservative surgical approach: the triple P procedure. Best Pract Res Clin Obstet Gynaecol 20:S1521–6934(20)30119-X.
Mohamed MA, Mohammed AH (2019) Parallel vertical compression sutures to control bleeding in cases of placenta previa and accreta. J Matern Fetal Neonatal Med 32(4):641–645
Chen Li, Wang X, Wang H et al (2019) Clinical evaluation of prophylactic abdominal aortic balloon occlusion in patients with placenta accreta: a systematic review and meta-analysis. BMC Pregnancy Childbirth 19(1):30
Matsubara S, Takahashi H (2018) Bakri balloon for placenta accreta spectrum disorder: an alternative to caesarean hysterectomy? J Obstet Gynaecol 38(8):1186
Pala Ş, Atilgan R, Başpınar M et al (2018) Comparison of results of Bakri balloon tamponade and caesarean hysterectomy in management of placenta accreta and increta: a retrospective study. J Obstet Gynaecol 38(2):194–199
Thabet M, Abdelhafez MS, Fyala EA (2018) Intrauterine inflated foley’s catheter balloon in the management of abnormally invasive placenta previa: a case-control study. J Obstet Gynaecol India 68(3):185–191
Barinov S, Tirskaya Y, Medyannikova I et al (2019) A new approach to fertility-preserving surgery in patients with placenta accreta. J Matern Fetal Neonatal Med 32(9):1449–1453
Soyama H, Miyamoto M, Ishibashi H et al (2019) Analysis of prophylactic Bakri balloon tamponade failure in patients with placenta previa. Taiwan J Obstet Gynecol 58(1):159–163
Chaoying Wu, Li Y, Ye W et al (2017) Cook Cervical Ripening Balloon successfully prevents excessive hemorrhage combined with ultrasound-guided suction curettage in the treatment of cesarean scar pregnancy. J Obstet Gynaecol Res 43(6):1043–1047
Jauniaux E, Bhide A, Kennedy A et al (2018) FIGO consensus guidelines on placenta accreta spectrum disorders: prenatal diagnosis and screening. Int J Gynaecol Obstet 140(3):274–280
Ishibashi H, Miyamoto M, Iwahashi H et al (2021) Criteria for placenta accreta spectrum in the International Federation of Gynaecology and Obstetrics classification, and topographic invasion area are associated with massive hemorrhage in patients with placenta previa. Acta Obstet Gynecol Scand 100(6):1019–1025
Dedes I, Ziogas V (2008) Circular isthmic-cervical sutures can be an alternative method to control peripartum haemorrhage during caesarean section for placenta praevia accreta. Arch Gynecol Obstet 278(6):555–7
Mohamed MA (2021) Lower segment folding as novel technique to control bleeding in cases of morbidly adherent placenta. J Matern Fetal Neonatal Med 34(20):3397–3401
El Gelany SA, Abdelraheim AR, Mohammed MM et al (2015) The cervix as a natural tamponade in postpartum hemorrhage caused by placenta previa and placenta previa accreta: a prospective study. BMC Pregnancy Childbirth 15:295
Pan XY, Wang YP, Zheng Z (2015) A marked increase in obstetric hysterectomy for placenta accreta. Chin. Med J Engl 128:2189e2193
Kassem GA, Alzahrani AK (2013) Maternal and neonatal outcomes of placenta previa and placenta accreta: three years of experience with a two-consultant approach. Int J Womens Health 5:803e810
Palacios-Jaraquemada JM, Fiorillo A, Hamer J et al (2020) Placenta accreta spectrum: a hysterectomy can be prevented in almost 80% of cases using a resective-reconstructive technique. J Matern Fetal Neonatal Med 26:1e8
Palacios Jaraquemada JM (2016) Abnormal invasive placentation: management and complications. In: Malvasi A, Tinelli A, Di Renzo GC (eds) Management and therapy of late pregnancy complications: third trimester and puerperium. Springer International Publishing, Berlin, pp 191–207
Ishii T, Sawada K, Koyama S (2012) Balloon tamponade during cesarean section is useful for severe post-partum hemorrhage due to placenta previa. J Obstet Gynaecol Res 38(1):102–7
Lau MS, Tee JC (2009) Use of a large Rusch hydrostatic catheter balloon to control postpartum haemorrhage resulting from a low placental implantation. Singapore Med J 50(9):e321–e323
Uygur D, Altun Ensari T, Ozgu-Erdinc AS (2014) Successful use of BT-Cath balloon tamponade in the management of postpartum haemorrhage due to placenta previa. Eur J Obstet Gynecol Reprod Biol 181:223–228
Zhu L, Lu J, Huang W et al (2021) A modified suture technique for the treatment of patients with pernicious placenta previa and placenta accreta spectrum: a case series. Ann Transl Med 9(14):1140
Wright JD, Pri-Paz S, Herzog TJ et al (2011) Predictors of massive blood loss in women with placenta accreta. Am J Obstet Gynecol 205:38.e1–6
Jauniaux E, Bunce C, Grønbeck L et al (2019) Prevalence and main outcomes of placenta accreta spectrum: a systematic review and meta-analysis. Am J Obstet Gynecol 221:208e18
Chen D, Xu J, Ye P et al (2020) Risk scoring system with MRI for intraoperative massive hemorrhage in placenta previa and accreta. J Magn Reson Imaging 51(3):947–958
Bi S, Zhang L, Wang Z et al (2021) Effect of types of placenta previa on maternal and neonatal outcomes: a 10-year retrospective cohort study. Arch Gynecol Obstet 304(1):65–72
Matsubara S, Baba Y, Takahashi H (2018) Placenta previa and hemorrhage: the placental location may be an important determinant of the bleeding amount. J Matern Fetal Neonatal Med 31(10):1390–1391
Duzyj CM, Cooper A, Mhatre M et al (2019) Placenta accreta: a spectrum of predictable risk, diagnosis, and morbidity. Am J Perinatol 36(10):1031–1038
Funding
This work was supported by National Key Research and Development Program of China (2021YFC2701504), Medical and Health Science Technology Development Plan of Shandong Province (2018WS274).
Author information
Authors and Affiliations
Contributions
YZG: manuscript writing, data collection, and data analysis; YZ: data collection; LL: data management; HYL: data analysis; S Wang: data management; YXW: manuscript writing/editing; CTZ: project development.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declared that they have no conflicts of interest to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gu, Y., Zhou, Y., Li, L. et al. Cook Cervical Ripening Balloon for placenta accreta spectrum disorders with placenta previa: a novel approach to uterus preserving. Arch Gynecol Obstet 306, 1979–1987 (2022). https://doi.org/10.1007/s00404-022-06476-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06476-6