Abstract
Objective
Intrauterine device (IUD) is a widely used long-acting contraceptive method; however, the side-effects related to IUD may lead to method discontinuation. The aim of this study is to evaluate the relation between the most common side-effects of IUD use; mainly dysmenorrhea, menorrhaghia, pelvic cramping and the relation of these complications with the position of the IUD device within the cavity and uterine dimensions evaluated by transvaginal ultrasonography.
Material and method
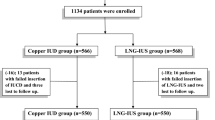
Two hundred and eighty-four patients who had Cu-T380A IUD insertion at the Family Planning Clinic of a tertiary health center were evaluated at insertion and 6 and 12 weeks after the insertion. Demographic characteristics, medical history, symptoms and findings of the gynecological examination were recorded. Transvaginal ultrasonographic measurement of the uterine dimensions, the distance between the tip of the Cu-IUD and the fundus, myometrium and endometrium were measured to evaluate the displacement of the IUD. The relationship between the symptoms and IUD displacement diagnosed by ultrasonographic examination were investigated.
Results
Two hundred and sixty-seven patients were followed-up for 12 weeks as the remaining 16 had partial or complete IUD expulsion. A statistically significantly shorter uterine length was measured in patients who complained of menorrhagia in comparison to the ones without this complaint (54.27 ± 6.11 vs 60.25 ± 10.52 mm, p = 0.02) while uterine length was similar in patients with or without dysmenorrhea at 12 weeks (59.60 ± 10.25 vs 60.33 ± 10.68 mm, p = 0.71). The distances between the tip of the IUD and the endometrium, myometrium and the uterine fundus, were statistically and significantly longer in patients who experienced pelvic cramping at 3rd month, showing a downward movement of the IUD. (Endometrium; 0.29 ± 0.72 vs 0.45 ± 0.35 mm, p = 0.02, Myometrium; 1.25 ± 1.39 vs 2.38 ± 2.26 mm p < 0.05, Fundus; 1.68 ± 2.39 vs 2.92 ± 1.78 mm, p < 0.05).
Conclusion
A shorter uterine cavity length seems to be a predictor of menorrhagia in patients with Cu-T 380A IUD. Patients experiencing pelvic cramping with IUD are more susceptible for IUD expulsion as the downward movement of IUD is more prominent in these patients.


Similar content being viewed by others
References
Darney LS, Philip D (2010) A clinical guide for contraception, 5th edn. Lippincott Williams & Wilkins, Philadelphia, pp 242–243
Winner B, Peipert JF, Zhao Q, Buckel C, Madden T, Allsworth JE, Secura GM (2012) Effectiveness of long acting reversible contraception. N Engl J Med 366(21):1998–2007
O’Brien PA, Kulier R, Helmerhorst FM, Usher-Patel M, d’Arcangues C (2008) Copper-containing, framed intrauterine devices for contraception: a systematic review of randomized controlled trials. Contraception 77(5):318–327
WHO (2015) “Intrauterine devices (IUDs)”. Medical eligibility criteria for contraceptive use, 5th edn. http://www.who.int/reproductivehealth/publications/family_planning/MEC-5/en/. Available at 15 Jan 2016
Peri N, Graham D, Levine D (2007) Imaging of intrauterine contraceptive devices. J Ultrasound Med 26(10):1389–1401
Coskun E, Cakiroglu Y, Aygun BK, Muezzinoglu B, Caliskan E (2011) Effect of copper intrauterine device on the cyclooxygenase and inducible nitric oxide synthase expression in the luteal phase endometrium. Contraception 84(6):637–641
Mutlu I, Demir A, Mutlu MF (2014) Can uterine artery Doppler parameters predict copper intrauterine device-induced side effects? Eur J Contracept Reprod Health Care 19(1):51–56
Faundes D, Perdigao A, Faundes A, Bahamondes L, Petta CA (2000) T-shaped IUDs accommodate in their position during the first 3 months after insertion. Contraception. 62(4):165–168
Warner PE, Critchley HO, Lumsden MA, Campbell-Brown M, Douglas A, Murray GD (2004) Menorrhagia I: measured blood loss, clinical features, and outcome in women with heavy periods: a survey with follow-up data. Am J Obstet Gynecol 190:1216–1223
Faundes D, Bahamondes L, Faundes A, Marchi N (1997) No relation between the intrauterine contraceptive device position evaluated by ultrasound and complaints of bleeding and pain. Contraception 56:43–47
Sivin I, Batár I (2010) State-of-the-art of non-hormonal methods of contraception: III. Intrauterine devices. Eur J Contracept Reprod Health Care 15:96–112
Petta CA, Faúndes D, Pimentel E, Diaz J, Bahamondes L (1996) The use of vaginal ultrasound to identify copper T IUDs at high risk of expulsion. Contraception 54(5):287–289
Liang H, Li L, Yuan W, Zou Y, Gao ES, Duffy JM, Wu SC (2014) Dimensions of the endometrial cavity and intrauterine device expulsion or removal for displacement: a nested case-control study. BJOG 121(8):997–1004
Shimoni N, Davis A, Westhoff C (2014) Can ultrasound predict IUD expulsion after medical abortion? Contraception 89(5):434–439
Yigit N, Kacar M, Yigit H et al (2009) The effects of copper contraceptive intrauterine device on the uterine blood flow: a prospective transvaginal Doppler study. J Clin Ultrasound 37:380–384
El-Mazny, Abou-Salem N, Elshenoufy H (2013) Three-dimensional power Doppler study of endometrial and subendometrial microvascularization in women with intrauterine device-induced menorrhagia. Fertil Steril 99(7):1912–1957
Shen O, Ben Chetrit A, Margalioth EJ, Lavie O, Rabinowitz RR (2008) Effects of a copper-medicated intrauterine device on ovarian artery, uterine artery, and intrauterine blood flow. Gynecol Obstet Invest 66(4):253–256
de Souza MA, Geber S (2006) Doppler color flow analysis of the uterine arteries before and after intrauterine device insertion: a prospective study. J Ultrasound Med 25(2):153–157
Pirhonen J, Pulkkinen M (1995) The effect of nimesulide and naproxen on the uterine and ovary arterial blood flow velocity. A Doppler study. Acta Obstet Gynecol Scand 74:549–553
Wildemeersch D (2011) Intrauterine contraceptives that do not fit well contribute to early discontinuation. Eur J Contracept Reprod Health Care 16(2):135–141
Bajka M, Badir S (2017) Fundus thickness assessment by 3D transvaginal ultrasound allows metrics-based diagnosis and treatment of congenital uterine anomalies. Ultraschall Med 38(2):183–189
Benacerraf BR, Shipp TD, Bromley B (2009) Three-dimensional ultrasound detection of abnormally located intrauterine contraceptive devices which are a source of pelvic pain and abnormal bleeding. Ultrasound Obstet Gynecol 34(1):110–115
Wildemeersch D, Jandi S, Pett A, Nolte K, Hasskamp T, Vrijens M (2014) Use of frameless intrauterine devices and systems in young nulliparous and adolescent women: results of a multicenter study. Int J Womens Health 6(6):727–734
Kaislasuo J, Heikinheimo O, Lähteenmäki P, Suhonen S (2014) Predicting painful or difficult intrauterine device insertion in nulligravid women. Obstet Gynecol 124(2 Pt 1):345–353
Kaislasuo J, Heikinheimo O, Lähteenmäki P, Suhonen S (2015) Menstrual characteristics and ultrasonographic uterine cavity measurements predict bleeding and pain in nulligravid women using intrauterine contraception. Hum Reprod 30(7):1580–1588
Jiménez MF, Vetori D, Fagundes PA, de Freitas FM, Cunha-Filho JS (2008) Subendometrial microvascularization and uterine artery blood flow in IUD-induced side effects (levonorgestrel intrauterine system and copper intrauterine device). Contraception 78(4):324–327
Sahmay S, Kaleli S, Oral E, Alper T, Unal O, Karacan I, Atasu T (1999) Effect of different types of intrauterine devices on intrauterine activity. Int J Fertil Womens Med 44(3):150–155
Goldstuck ND, Wildemeersch D (2014) Role of uterine forces in intrauterine device embedment, perforation, and expulsion. Int J Womens Health 7(6):735–744
Morales-Rosello J (2005) Spontaneous upward movement of lowly placed T-shaped IUDs. Contraception 72:430–431
Eggebroten JL, Sanders JN, Turok DK (2017) Immediate postpartum intrauterine device and implant program outcomes: a prospective analysis. Am J Obstet Gynecol 217(1):51.e1–51.e7
Eroğlu K, Akkuzu G, Vural G, Dilbaz B, Akin A, Taşkin L, Haberal A (2006) Comparison of efficacy and complications of IUD insertion in immediate postplacental/early postpartum period with interval period: 1 year follow-up. Contraception 74(5):376–381
Author information
Authors and Affiliations
Contributions
SF: Corresponding author, data curation, data collection; BD: lead supervisor, project development; EF: writing, data analysis; SD: supporting supervisor
Corresponding author
Ethics declarations
Funding
This study was not funded by any company.
Conflict of interest
Conflict of interest is declared by none of the authors.
Human and animal rights statement
This article does not contain any studies with human participants or animals performed by any of the authors.
Ethical approval
Study is approved by Ankara Etlik Zübeyde Hanım Education and Training Hospital Institutional Review Board.
Rights and permissions
About this article
Cite this article
Fadiloglu, S., Dilbaz, B., Fadiloglu, E. et al. Relationship between copper IUD complications and ultrasonographic findings. Arch Gynecol Obstet 297, 989–996 (2018). https://doi.org/10.1007/s00404-018-4711-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-4711-y