Abstract
Purpose
Epilepsy is one of the most common neurological diseases during pregnancy. However, the influence of epilepsy on fetal growth is not understood. Thus, this study conducted a meta-analysis to determine the influence of epilepsy during pregnancy on fetal growth restriction (FGR).
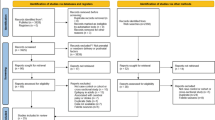
Methods
BIOSIS, Medline, Embase, and PubMed databases were searched between January 2000 and January 2016. Without imposing language or regional restrictions, referenced articles were selected.
Results
Final analysis included 684 citations from 11 studies. Estimated risk of FGR was 1.28-fold higher in epileptic pregnant women than in non-epileptic women [95% confidence interval (95% CI) 1.09–1.50, p < 0.05]. Given the course of previous studies, hierarchical analysis of pregnant women who use antiepileptic drugs (AEDs) was conducted. Results show that FGR rate is significantly increased even if AEDs were taken [odds ratio 1.26, 95% CI 1.13–1.41, p < 0.05].
Conclusions
Although modest bias cannot be avoided, our meta-analysis indicated that epilepsy participates in fetal development as an unfavorable factor, and AEDs seemed to be useless in decreasing the occurrence rate of FGR.



Similar content being viewed by others
References
Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, Engel J Jr, Forsgren L, French JA, Glynn M, Hesdorffer DC, Lee BI, Mathern GW, Moshe SL, Perucca E, Scheffer IE, Tomson T, Watanabe M, Wiebe S (2014) ILAE official report: a practical clinical definition of epilepsy. Epilepsia 55(4):475–482. doi:10.1111/epi.12550
Scheffer IE, Berkovic S, Capovilla G, Connolly MB, French J, Guilhoto L, Hirsch E, Jain S, Mathern GW, Moshe SL, Nordli DR, Perucca E, Tomson T, Wiebe S, Zhang YH, Zuberi SM (2017) ILAE classification of the epilepsies: position paper of the ILAE Commission for Classification and Terminology. Epilepsia 58(4):512–521. doi:10.1111/epi.13709
Barroso FVL, Araujo Júnior E, Guazelli CAF, Santana EFM, Rolo LC, Martins MdG, Moron AF (2015) Perinatal outcomes from the use of antiepileptic drugs during pregnancy: a case–control study. J Matern-Fetal Neonatal Med 28(12):1445–1450. doi:10.3109/14767058.2014.955006
Najafi MR, Sonbolestan F, Sonbolestan SA, Zare M, Mehvari J, Meshkati SN (2012) The course and outcome of pregnancy and neonatal situation in epileptic women. Adv Biomed Res 1:4. doi:10.4103/2277-9175.94426
Brosh K, Matok I, Sheiner E, Koren G, Wiznitzer A, Gorodischer R, Levy A (2011) Teratogenic determinants of first-trimester exposure to antiepileptic medications. J Popul Ther Clin Pharmacol 18:e89–e98
Borthen I, Eide MG, Veiby G, Daltveit AK, Gilhus NE (2009) Complications during pregnancy in women with epilepsy: population-based cohort study. BJOG: Int J Obstet Gynaecol 116(13):1736–1742. doi:10.1111/j.1471-0528.2009.02354.x
Hauser WA, Annegers JF, Kurland LT (1993) Incidence of epilepsy and unprovoked seizures in Rochester, Minnesota: 1935–1984. Epilepsia 34(3):453
Edey S, Moran N, Nashef L (2014) SUDEP and epilepsy-related mortality in pregnancy. Epilepsia 55(7):e72–e74. doi:10.1111/epi.12621
Veiby G, Daltveit AK, Engelsen BA, Gilhus NE (2009) Pregnancy, delivery, and outcome for the child in maternal epilepsy. Epilepsia 50(9):2130–2139
Lin HL, Chen YH, Lin HC, Lin HC (2009) No increase in adverse pregnancy outcomes for women receiving antiepileptic drugs. J Neurol 256(10):1742–1749. doi:10.1007/s00415-009-5222-3
Nardozza LM, Caetano AC, Zamarian AC, Mazzola JB, Silva CP, Marcal VM, Lobo TF, Peixoto AB, Araujo Junior E (2017) Fetal growth restriction: current knowledge. Arch Gynecol Obstet 295(5):1061–1077. doi:10.1007/s00404-017-4341-9
Stanley JL, Andersson IJ, Hirt CJ, Moore L, Dilworth MR, Chade AR, Sibley CP, Davidge ST, Baker PN (2012) Effect of the anti-oxidant tempol on fetal growth in a mouse model of fetal growth restriction. Biol Reprod 87(1):25, 21–28. doi:10.1095/biolreprod.111.096198
Hvas CL, Henriksen TB, Ostergaard JR, Dam M (2005) Epilepsy and pregnancy: effect of antiepileptic drugs and lifestyle on birthweight. BJOG: Int J Obstet Gynaecol 107(7):896–902
Wells G, Shea B, O’Connell D (2000) Proceedings of the third symposium on systematic reviews beyond the basics. SBOD. Improving quality and impact; The Newcastle–Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analysis, Oxford, 3–5 July
Kilic D, Pedersen H, Kjaersgaard MI, Parner ET, Vestergaard M, Sorensen MJ, Olsen J, Bech BH, Christensen J, Pedersen LH (2014) Birth outcomes after prenatal exposure to antiepileptic drugs—a population-based study. Epilepsia 55(11):1714–1721. doi:10.1111/epi.12758
Farmen AH, Grundt J, Tomson T, Nakken KO, Nakling J, Mowinchel P, Lossius M (2015) Intrauterine growth retardation in foetuses of women with epilepsy. Seizure 28:76–80. doi:10.1016/j.seizure.2015.02.026
Katz O, Levy A, Wiznitzer A, Sheiner E (2006) Pregnancy and perinatal outcome in epileptic women: a population-based study. J Matern-Fetal Neonatal Med 19(1):21–25. doi:10.1080/14767050500434096
McPherson JA, Harper LM, Odibo AO, Roehl KA, Cahill AG (2013) Maternal seizure disorder and risk of adverse pregnancy outcomes. Am J Obstet Gynecol 208(5):378 e371–378 e375. doi:10.1016/j.ajog.2013.01.048
Jadhav SV, Jadhav VK (2013) Comparative study of obstetric outcome in epileptic and non-epileptic pregnant women. Indian Med Gaz 147(9):352–357
Venturella A, Harper L, Odibo A, Roehl K, Cahill A (2012) 320: maternal seizure disorder is not associated with adverse pregnancy outcomes. Am J Obstet Gynecol 206(1):S152
Viinikainen K, Heinonen S, Kai E, Kälviäinen R (2006) Community-based, prospective, controlled study of obstetric and neonatal outcome of 179 pregnancies in women with epilepsy. Epilepsia 47(1):186–192
Chen YH, Chiou HY, Lin HC, Lin HL (2009) Affect of seizures during gestation on pregnancy outcomes in women with epilepsy. Arch Neurol 66(8):979–984
Veiby G, Daltveit AK, Engelsen BA, Gilhus NE (2014) Fetal growth restriction and birth defects with newer and older antiepileptic drugs during pregnancy. J Neurol 261(3):579–588
Viale L, Allotey J, Cheong-See F, Arroyo-Manzano D, McCorry D, Bagary M, Mignini L, Khan KS, Zamora J, Thangaratinam S (2015) Epilepsy in pregnancy and reproductive outcomes: a systematic review and meta-analysis. Lancet 386(10006):1845–1852. doi:10.1016/s0140-6736(15)00045-8
Crawford P (1997) Epilepsy and pregnancy: good management reduces the risks. Prof Care Mother Child 7(1):17–18
Lainé-Cessac P, Le JS, Rosenau L, Gamelin L, Allain P, Grosieux P (1995) Uncontrolled retrospective study of 75 pregnancies in women treated for epilepsy. Journal De Gynécologie Obstétrique Et Biologie De La Reproduction 24(5):537
Perucca E (2005) Birth defects after prenatal exposure to antiepileptic drugs. Lancet Neurol 4(11):781–786
Tomson T, Ohman I, Vitols S (1997) Lamotrigine in pregnancy and lactation: a case report. Epilepsia 38(9):1039–1041
Ohman I, Vitols S, Tomson T (2000) Lamotrigine in pregnancy: pharmacokinetics during delivery, in the neonate, and during lactation. Epilepsia 41(6):709–713
Rambeck B, Kurlemann G, Stodieck SR, May TW, Jürgens U (1997) Concentrations of lamotrigine in a mother on lamotrigine treatment and her newborn child. Eur J Clin Pharmacol 51(6):481
Bülau P, Paar WD, Unruh GEV (1988) Pharmacokinetics of oxcarbazepine and 10-hydroxy-carbazepine in the newborn child of an oxcarbazepine-treated mother. Eur J Clin Pharmacol 34(3):311–313
Ishizaki T, Yokochi K, Chiba K, Tabuchi T, Wagatsuma T (1981) Placental transfer of anticonvulsants (phenobarbital, phenytoin, valproic acid) and the elimination from neonates. Pediatr Pharmacol 1(4):291–303
Nau H, Rating D, Koch S, Häuser I, Helge H (1981) Valproic acid and its metabolites: placental transfer, neonatal pharmacokinetics, transfer via mother’s milk and clinical status in neonates of epileptic mothers. J Pharmacol Exp Ther 219(3):768
Pacifici GM, Nottoli R (1995) Placental transfer of drugs administered to the mother. Clin Pharmacokinet 28(3):235–269
Arvela P (1995) Carbamazepine and its metabolites in human perfused placenta and in maternal and cord blood. Epilepsia 36(3):241–248
Myllynen P, Pienimäki P, Jouppila P, Vähäkangas K (2001) Transplacental passage of oxcarbazepine and its metabolites in vivo. Epilepsia 42(11):1482
Pienimäki P, Lampela E, Hakkola J, Arvela P, Raunio H, Vähäkangas K (1997) Pharmacokinetics of oxcarbazepine and carbamazepine in human placenta. Epilepsia 38(3):309–316
Bech BH, Kjaersgaard MIS, Pedersen HS, Howards PP, Sørensen MJ, Olsen J, Parner ET, Pedersen LH, Vestergaard M, Christensen J (2014) Use of antiepileptic drugs during pregnancy and risk of spontaneous abortion and stillbirth: population based cohort study. BMJ Clin Res 349:g5159
Simon R, Altman DG (1994) Statistical aspects of prognostic factor studies in oncology. Br J Cancer 69(6):979–985
Author information
Authors and Affiliations
Contributions
HLP, BP: Project development, manuscript editing. DJC: Data collection, manuscript writing. XD: Data collection. LSH, HLP: Data analysis.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Chen, D., Hou, L., Duan, X. et al. Effect of epilepsy in pregnancy on fetal growth restriction: a systematic review and meta-analysis. Arch Gynecol Obstet 296, 421–427 (2017). https://doi.org/10.1007/s00404-017-4404-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4404-y