Abstract
Purpose
To perform a systematic review and meta-analysis of reported estimates of adverse pregnancy outcomes among multiple births conceived with in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI).
Methods
PubMed, Google Scholar, Cochrane Libraries and Chinese databases were searched through May 2016 for cohort studies assessing adverse pregnancy outcomes associated with IVF/ICSI multiple births. Random-effects meta-analyses were used to calculate pooled estimates of adverse pregnancy outcomes and, where appropriate, heterogeneity was explored in group-specific analyses.
Results
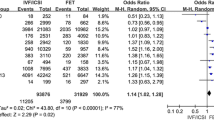
Sixty-four studies, with 60,210 IVF/ICSI multiple births and 146,737 spontaneously conceived multiple births, were selected for analysis. Among IVF/ICSI multiple births, the pooled estimates were 51.5% [95% confidence interval (CI): 48.7–54.3] for preterm birth, 12.1% (95% CI: 10.4–14.1) for very preterm birth, 49.8% (95% CI: 47.6–52.0) for low birth weight, 8.4% (95% CI: 7.1–9.9) for very low birth weight, 16.2% (95% CI: 12.9–20.1) for small for gestational age, 3.0% (95% CI: 2.5–3.7) for perinatal mortality and 4.7% (95% CI: 4.0–5.6) for congenital malformations. When the data were restricted to twins, the pooled estimates also showed a high prevalence of adverse outcomes. There was a similar prevalence of poor outcomes among multiple births conceived with IVF/ICSI and naturally (all P ≥ 0.0792). Significant differences in different continents, countries, and income groups were found.
Conclusions
The IVF/ICSI multiple pregnancies have a high prevalence of adverse pregnancy outcomes. However, population-wide prospective adverse outcomes registries covering the entire world population for IVF/ICSI pregnancies are needed to determine the exact perinatal prevalence.






Similar content being viewed by others
References
Kissin DM, Jamieson DJ, Barfield WD (2014) Monitoring health outcomes of assisted reproductive technology. N Engl J Med 371:91–93
Hansen M, Kurinczuk JJ, de Klerk N, Burton P, Bower C (2012) Assisted reproductive technology and major birth defects in Western Australia. Obstet Gynecol 120:852–863
Farhi A, Reichman B, Boyko V, Hourvitz A, Ron-El R, Lerner-Geva L (2013) Maternal and neonatal health outcomes following assisted reproduction. Reprod Biomed Online 26:454–461
Fujii M, Matsuoka R, Bergel E, van der Poel S, Okai T (2010) Perinatal risk in singleton pregnancies after in vitro fertilization. Fertil Steril 94:2113–2117
Centers for Disease Control and Prevention (2013) Assisted Reproductive Technology Fertility Clinic Success Rates Report. http://www.cdc.gov/art/reports/2013/fertility-clinic.html. Accessed 15 July 2016
Malchau SS, Loft A, Larsen EC, Aaris Henningsen AK, Rasmussen S, Andersen AN et al (2013) Perinatal outcomes in 375 children born after oocyte donation: a Danish national cohort study. Fertil Steril 99:1637–1643
European IVF-Monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE), Calhaz-Jorge C, de Geyter C, Kupka MS, de Mouzon J, Erb K et al (2016) Assisted reproductive technology in Europe, 2012: results generated from European registers by ESHRE. Hum Reprod 31:1638–1652
Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA (2012) National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med 9:e1001356
Moini A, Shiva M, Arabipoor A, Hosseini R, Chehrazi M, Sadeghi M (2012) Obstetric and neonatal outcomes of twin pregnancies conceived by assisted reproductive technology compared with twin pregnancies conceived spontaneously: a prospective follow-up study. Eur J Obstet Gynecol Reprod Biol 165:29–32
Green NS (2004) Risks of birth defects and other adverse outcomes associated with assisted reproductive technology. Pediatrics 114:256–259
Russell RB, Petrini JR, Damus K, Mattison DR, Schwarz RH (2003) The changing epidemiology of multiple births in the United States. Obstet Gynecol 101:129–135
National Vital Statistics Reports. Births: Final Data for 2012. https://www.cdc.gov/nchs/data/nvsr/nvsr62/nvsr62_09.pdf. Accessed 18 December 2016
Qin J, Wang H, Sheng X, Liang D, Tan H, Xia J (2015) Pregnancy-related complications and adverse pregnancy outcomes in multiple pregnancies resulting from assisted reproductive technology: a meta-analysis of cohort studies. Fertil Steril 103: 1492–508.e1-7
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D et al (2000) Meta-analysis of observational studies in epidemiology (MOOSE) group. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 283:2008–2012
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
The World Bank Group (2014) World Bank Income groups distribution. http://data.worldbank.org/about/country-and-lending-groups. Accessed 25 June 2016
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Wennerholm UB, Bergh C, Hamberger L, Nilsson L, Reismer E, Wennergren M et al (1996) Obstetric and perinatal outcome of pregnancies following intracytoplasmic sperm injection. Hum Reprod 11:1113–1119
Wennerholm UB, Hamberger L, Nilsson L, Wennergren M, Wikland M, Bergh C (1997) Obstetric and perinatal outcome of children conceived from cryopreserved embryos. Hum Reprod 12:1819–1825
Dhont M, De Neubourg F, Van der Elst J, De Sutter P (1997) Perinatal outcome of pregnancies after assisted reproduction: a case-control study. J Assist Reprod Genet 14:575–580
Dhont M, De Sutter P, Ruyssinck G, Martens G, Bekaert A (1999) Perinatal outcome of pregnancies after assisted reproduction: a case-control study. Am J Obstet Gynecol 181:688–695
Loft A, Petersen K, Erb K, Mikkelsen AL, Grinsted J, Hald F et al (1999) A Danish national cohort of 730 infants born after intracytoplasmic sperm injection (ICSI) 1994–1997. Hum Reprod 14:2143–2148
Wennerholm UB, Bergh C, Hamberger L, Lundin K, Nilsson L, Wikland M et al (2000) Incidence of congenital malformations in children born after ICSI. Hum Reprod 15:944–948
Koudstaal J, Bruinse HW, Helmerhorst FM, Vermeiden JP, Willemsen WN, Visser GH (2000) Obstetric outcome of twin pregnancies after in-vitro fertilization: a matched control study in four Dutch university hospitals. Hum Reprod 15:935–940
Koivurova S, Hartikainen AL, Gissler M, Hemminki E, Sovio U, Järvelin MR (2002) Neonatal outcome and congenital malformations in children born after in-vitro fertilization. Hum Reprod 17:1391–1398
Isaksson R, Gissler M, Tiitinen A (2002) Obstetric outcome among women with unexplained infertility after IVF: a matched case-control study. Hum Reprod 17:1755–1761
Hansen M, Kurinczuk JJ, Bower C, Webb S (2002) The risk of major birth defects after intracytoplasmic sperm injection and in vitro fertilization. N Engl J Med 346:725–730
Bonduelle M, Liebaers I, Deketelaere V, Derde MP, Camus M, Devroey P et al (2002) Neonatal data on a cohort of 2889 infants born after ICSI (1991–1999) and of 2995 infants born after IVF (1983–1999). Hum Reprod 17:671–694
Ludwig M, Katalinic A (2003) Pregnancy course and health of children born after ICSI depending on parameters of male factor infertility. Hum Reprod 18:351–357
Ochsenkühn R, Strowitzki T, Gurtner M, Strauss A, Schulze A, Hepp H et al (2003) Pregnancy complications, obstetric risks, and neonatal outcome in singleton and twin pregnancies after GIFT and IVF. Arch Gynecol Obstet 268:256–261
Nassar AH, Usta IM, Rechdan JB, Harb TS, Adra AM, Abu-Musa AA (2003) Pregnancy outcome in spontaneous twins versus twins who were conceived through in vitro fertilization. Am J Obstet Gynecol 189:513–518
Katalinic A, Rösch C, Ludwig M, German ICSI Follow-Up Study Group (2004) Pregnancy course and outcome after intracytoplasmic sperm injection: a controlled, prospective cohort study. Fertil Steril 81:1604–1616
Pinborg A, Loft A, Rasmussen S, Schmidt L, Langhoff-Roos J, Greisen G et al (2004) Neonatal outcome in a Danish national cohort of 3438 IVF/ICSI and 10,362 non-IVF/ICSI twins born between 1995 and 2000. Hum Reprod 19:435–441
Kuwata T, Matsubara S, Ohkuchi A, Watanabe T, Izumi A, Honma Y et al (2004) The risk of birth defects in dichorionic twins conceived by assisted reproductive technology. Twin Res 7: 223–227
Manoura A, Korakaki E, Hatzidaki E, Bikouvarakis S, Papageorgiou M, Giannakopoulou C (2004) Perinatal outcome of twin pregnancies after in vitro fertilization. Acta Obstet Gynecol Scand 83:1079–1084
Cheng LH, Cao YX (2004) Pregnancy outcomes following after assisted reproductive technologies. Chin J Pract Gynecol Obstet 20:231–232
Lin WQ, Lin JJ, Ye BL, Chen YQ, Zhao JZ, Zhou Y et al (2004) A comparison of pregnancy outcomes between in vitro fertilization and intracytoplasmic sperm injection. Chin J Obstet Gynecol 39:108–111
Zhu GJ, Le L, Liu Q, Liu YQ (2004) Maternal complications and neonatal outcomes among 605 pregnant women after IVF. Chin J Perinat Med 7:104–105
Agarwal P, Loh SK, Lim SB, Sriram B, Daniel ML, Yeo SH et al (2005) Two-year neurodevelopmental outcome in children conceived by intracytoplasmic sperm injection: prospective cohort study. BJOG 112:1376–1383
Olson CK, Keppler-Noreuil KM, Romitti PA, Budelier WT, Ryan G, Sparks AE et al (2005) In vitro fertilization is associated with an increase in major birth defects. Fertil Steril 84:1308–1315
Ombelet W, Peeraer K, De Sutter P, Gerris J, Bosmans E, Martens G et al (2005) Perinatal outcome of ICSI pregnancies compared with a matched group of natural conception pregnancies in Flanders(Belgium): a cohort study. Reprod Biomed Online 11:244–253
Klemetti R, Gissler M, Sevón T, Koivurova S, Ritvanen A, Hemminki E (2005) Children born after assisted fertilization have an increased rate of major congenital anomalies. Fertil Steril 84:1300–1307
Ho CH, Peng FS, Chen HF, Lien YR, Chen SU, Yang YS (2005) Twin pregnancies conceived by assisted reproductive technology: maternal and perinatal outcomes. Taiwan J Obstet Gynecol 44:332–337
Ai W, Liu ZP (2005) Study on the adverse outcomes in twins conceived by IVF-ET. Matern Child Health Care China 20:3119–3120
Li FL, Wu WL, Zou SH, Wu RY, Song DP (2005) Neonatal outcomes of children born after in vitro fertilization-embryo transfer. Chin J Birth Health Hered 13:83–85
Xu ZY, Ye BL, Lin JJ, Lin WQ, Lin LL (2005) Analysis of perinatal outcomes of twin pregnancies conceived by in vitro fertilization and embryo transfer(IVF-ET) and those conceived spontaneously. J Wenzhou Med Coll 35:34–36
Wu J, Cao YX (2006) The analysis on the clinical effects of the twin pregnancies after assisted reproductive technology. Acta Universitatis Medicinalis Anhui 41:341–343
Saygan-Karamürsel B, Tekşam O, Aksu T, Yurdakök M, Onderoğlu L (2006) Perinatal outcomes of spontaneous twins compared with twins conceived through intracytoplasmic sperm injection. J Perinat Med 34:132–138
Wang ZJ, Shao XG (2007) Pregnancy outcomes of twin pregnancies conceived by assisted reproductive technique and those conceived spontaneously. Prog Obstet Gynecol 16:417–419
Zuppa AA, Scorrano A, Cota F, D’Andrea V, Fracchiolla A, Romagnoli C (2007) Neonatal outcomes in triplet pregnancies: assisted reproduction versus spontaneous conception. J Perinat Med 35:339–343
Zhang LY, Yu YH, Chen HY, Su GD (2008) Maternal and neonatal outcomes of twin pregnancy following IVF-ET: comparison with twin pregnancies obtained spontaneously. Matern Child Health Care China 23:1286–1289
Long M, Shi XJ (2009) Low birth weight and birth defects among 451 infants conceived with IVF. J Guiyang Med Coll 34:323–324
Yi YH, Huang R, Wu JZ, Huang CY, Wang YF (2009) Outcomes of in vitro fertilization and embryo transfer in 1021 pregnant women. J Trop Med 9:292–294
Vasario E, Borgarello V, Bossotti C, Libanori E, Biolcati M, Arduino S et al (2010) IVF twins have similar obstetric and neonatal outcome as spontaneously conceived twins: a prospective follow-up study. Reprod Biomed Online 21:422–428
Wen SW, Leader A, White RR, Léveillé MC, Wilkie V, Zhou J et al (2010) A comprehensive assessment of outcomes in pregnancies conceived by in vitro fertilization/ intracytoplasmic sperm injection. Eur J Obstet Gynecol Reprod Biol 150:160–165
Hang F (2010) Research on the safety of assisted reproductive medicine[D]. Huazhong University of Science and Technology
Wu QF, Xu DF, Zhao Y, Xin CL (2010) Outcomes of 223 twins born after assisted reproductive techniques compared with 281 twins born after natural conception. Jiangxi Med J 46:95–97
Yang H, Choi YS, Nam KH, Kwon JY, Park YW, Kim YH (2011) Obstetric and perinatal outcomes of dichorionic twin pregnancies according to methods of conception: spontaneous versus in-vitro fertilization. Twin Res Hum Genet 14:98–103
Long XL, Zhang WH, Zhang WL, Du HZ, Wu YX (2011) Risk analysis of birth defects and low birth weight among IVF-conceived infants. Guangdong Med J 32:871–872
Fadini R, Mignini Renzini M, Guarnieri T, Dal Canto M, De Ponti E, Sutcliffe A et al (2012) Comparison of the obstetric and perinatal outcomes of children conceived from in vitro or in vivo matured oocytes in in vitro maturation treatments with births from conventional ICSI cycles. Hum Reprod 27:3601–3608
Sagot P, Bechoua S, Ferdynus C, Facy A, Flamm X, Gouyon JB et al (2012) Similarly increased congenital anomaly rates after intrauterine insemination and IVF technologies: a retrospective cohort study. Hum Reprod 27:902–909
Davies MJ, Moore VM, Willson KJ, Van Essen P, Priest K, Scott H et al (2012) Reproductive technologies and the risk of birth defects. N Engl J Med 366:1803–1813
Hu XF (2012) Twin pregnancies obtained with in vitro fertilization and embryo transfer and spontaneous pregnancy: a comparison of pregnancy outcomes. Acad J Second Mil Med Univ 33:694–695
Zeng MY, Hu LL (2012) Analysis of pregnancy outcomes in twin pregnancies conceived by assisted reproductive technology and naturally. Chin J Birth Health Hered 20:108–109
Ricciarelli E, Bruna I, Verdú V, Torrelló MJ, Herrer R, Gris JM et al (2013) Impact of assisted reproduction treatments on Spanish newborns: report of 14,119 pregnancies. J Assist Reprod Genet 30:897–905
Jiang YZ, Li CY, Xu YX (2013) Pregnancy outcomes in 620 twins conceived with IVF-ET. Ningxia Med J 35:863–864
Zheng CX, Wang XY, Lu XN (2013) Clinical outcomes analysis among twins conceived with IVF. Shaanxi Med J 42:1422–1423
Fedder J, Loft A, Parner ET, Rasmussen S, Pinborg A (2013) Neonatal outcome and congenital malformations in children born after ICSI with testicular or epididymal sperm: a controlled national cohort study. Hum Reprod 28:230–240
Poon WB, Lian WB (2013) Perinatal outcome of intrauterine insemination/clomiphene pregnancies represent an intermediate risk group compared with in vitro fertilisation/intracytoplasmic sperm injection and naturally conceived pregnancies. J Paediatr Child Health 49:733–740
Marino JL, Moore VM, Willson KJ, Rumbold A, Whitrow MJ, Giles LC et al (2014) Perinatal outcomes by mode of assisted conception and sub-fertility in an Australian data linkage cohort. PLoS One 9:e80398
Zeng Q, Li YM, Chen H (2014) Pregnancy outcome of twin pregnancies conceived by assisted reproductive technique and those conceived spontaneously. J Trop Med 14:211–213
Declercq E, Luke B, Belanoff C, Cabral H, Diop H, Gopal D et al (2015) Perinatal outcomes associated with assisted reproductive technology: the Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART). Fertil Steril 103:888–895
Heisey AS, Bell EM, Herdt-Losavio ML, Druschel C (2015) Surveillance of congenital malformations in infants conceived through assisted reproductive technology or other fertility treatments. Birth Defects Res A Clin Mol Teratol 103:119–126
Stern JE, Luke B, Tobias M, Gopal D, Hornstein MD, Diop H (2015) Adverse pregnancy and birth outcomes associated with underlying diagnosis with and without assisted reproductive technology treatment. Fertil Steril 103:1438–1445
Hou L, Zheng JL, Wang WY (2015) Clinical outcomes analysis among twin pregnancies conceived with IVF and naturally. J Pract Med 31:2343–2345
Liu Yu, Chen Lei, Yao Li (2015) Clinical analysis on twin pregnancy outcome after in vitro fertilization and embryo transfer. Anhui Med J 36:1086–1088.
Zhang Y, Dong J, Cai LB, Ma L, Qian RC, Liu JY (2015) Analysis and preventive strategies on twin pregnancy outcomes after IVF/ICSI-ET. Acta Universitatis Medicinalis Nanjing Nat Sci 35:1297–1301
Zhou J, Li B, Chen SQ, Xiao XF, Huang JL, Sun HJ et al (2016) Comparison of pregnancy outcomes between twin pregnancy conceived by IVF-ET and twin pregnancy conceived naturally. J Reprod Med 25:331–334
Shevell T, Malone FD, Vidaver J, Porter TF, Luthy DA, Comstock CH et al (2005) Assisted reproductive technology and pregnancy outcome. Obstet Gynecol 106:1039–1045
Centers for Disease Control and Prevention (CDC) (2000) Contribution of assisted reproductive technology and ovulation-inducing drugs to triplet and higher-order multiple births–United States, 1980–1997. MMWR Morb Mortal Wkly Rep 49:535–538
Gleicher N, Oleske DM, Tur-Kaspa I, Vidali A, Karande V (2000) Reducing the risk of high-order multiple pregnancy after ovarian stimulation with gonadotropins. N Engl J Med 343:2–7
Qin JB, Wang H, Sheng X, Xie Q, Gao S (2016) Assisted reproductive technology and risk of adverse obstetric outcomes in dichorionic twin pregnancies: a systematic review and meta-analysis. Fertil Steril 105:1180–1192
van der Linde D, Konings EE, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJ et al (2011) Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol 58:2241–2247
Badaruddoza, Afzal M, Akhtaruzzaman (1994) Inbreeding and congenital heart diseases in a north Indian population. Clin Genet 45:288–291
Naderi S (1979) Congenital abnormalities in newborns of consanguineous and nonconsanguineous parents. Obstet Gynecol 53:195–199
Acknowledgements
The study was carried out with the fund support of China Postdoctoral Science Foundation (2015M572248), Hunan Provincial Science and Technology Plan Project (2015RS4055), and Natural Science Foundation of Hunan Province (2016JJ4047). Authors thank editors and reviewers for their suggestions.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have stated explicitly that there are no conflicts of interest.
Funding
This study was funded by China Postdoctoral Science Foundation (2015M572248), Hunan Provincial Science and Technology Plan Project (2015RS4055), and Natural Science Foundation of Hunan Province (2016JJ4047).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Qin, JB., Sheng, XQ., Wang, H. et al. Worldwide prevalence of adverse pregnancy outcomes associated with in vitro fertilization/intracytoplasmic sperm injection among multiple births: a systematic review and meta-analysis based on cohort studies. Arch Gynecol Obstet 295, 577–597 (2017). https://doi.org/10.1007/s00404-017-4291-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4291-2