Abstract
Objective
To evaluate the effects of letrozole and cabergoline in a rat model of ovarian hyperstimulation syndrome (OHSS).
Study design
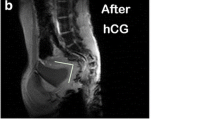
In this prospective, controlled experimental study, the 28 female Wistar rats were divided into four subgroups (one non-stimulated control and three OHSS-positive groups: placebo, letrozole, and cabergoline). To induce OHSS, rats were injected with 10 IU of pregnant mare serum gonadotropin from day 29 to day 32 of life, followed by subcutaneous injection of 30 IU hCG on day 33. Letrozole rats received with a single dose of 0.1 mg/kg letrozole via oral gavage, on the hCG day. Cabergoline rats received with a single dose of 100 µg/kg cabergoline via oral gavage, on the hCG day. All animals were compared in terms of body weight, vascular permeability (VP), ovarian diameter, ovarian tissue VEGF expression (assessed via immunohistochemical staining), and blood pigment epithelium-derived growth factor (PEDF) levels.
Results
The OHSS-positive placebo group (group 2) exhibited the highest VP, ovarian diameter, extent of VEGF staining, and lowest PEDF level, as expected. No significant difference was evident between the letrozole and cabergoline groups in terms of any of body weight; VP; PEDF level; ovarian diameter; or the staining intensity of, or percentage staining for, VEGF in ovarian tissues.
Conclusions
Letrozole and cabergoline were equally effective to prevent OHSS, reducing the ovarian diameter, VP, and PEDF and VEGF levels to similar extents.

Similar content being viewed by others
References
Klemetti R, Sevon T, Gissler M, Hemminki M (2005) Complications of IVF and ovulation induction. Hum Reprod 20(12):3293–3300
Stewart JA, Hamilton PJ, Murdoch AP (1997) Thromboembolic disease associated with ovarian stimulation and assisted conception techniques. Hum Reprod 12(10):2167–2173
McClure N, Healy DL, Rogers PA et al (1994) Vascular endothelial growth factor as capillary permeability agent in ovarian hyperstimulation syndrome. Lancet 344:235–236
Pietrowski D, Szabo L, Sator M et al (2012) Ovarian hyperstimulation syndrome is correlated with a reduction of soluble VEGF receptor protein level and a higher amount of VEGF-A. Hum Reprod 27:196–199
Carizza C, Abdelmassih V, Abdelmassih S et al (2008) Cabergoline reduces the early onset of ovarian hyperstimulation syndrome: a prospective randomized study. Reprod Biomed Online 17:751–755
Liu X, Chen HH, Zhang LW (2013) Potential therapeutic effects of pigment epithelium-derived factor for treatment of diabetic retinopathy. Int J Ophthalmol 6(2):221–227
Liu H, Ren JG, Cooper WL, Hawkins CE, Cowan MR, Tong PY (2004) Identification of the antivasopermeability effect of pigment epithelium-derived factor and its active site. Proc Natl Acad Sci USA 101(17):6605–6610
Yamagishi S, Ueda S, Matsui T, Nakamura K, Imaizumi T, Takeuchi M, Okuda S (2007) Pigment epithelium-derived factor (PEDF) prevents advanced glycation end products (AGEs)-elicited endothelial nitric oxide synthase (eNOS) reduction through its anti-oxidative properties. Protein Pept Lett 14(8):832–835
Yamagishi S, Matsui T, Nakamura K, Yoshida T, Shimizu K, Takegami Y, Shimizu T, Inoue H, Imaizumi T (2006) Pigment-epithelium-derived factor (PEDF) inhibits angiotensin-II-induced vascular endothelial growth factor (VEGF) expression in MOLT-3 T cells through anti-oxidative properties. Microvasc Res 71(3):222–226
Saylan A, Arioz DT, Koken T et al (2010) Prevention of ovarian hyperstimulation syndrome in a rat model: efficacy comparison between cabergoline and meloxicam. Acta Obstet Gynecol Scand 89:692–699
Tong XM, Zhang SY, Song T et al (2008) Effects of gonadotropin-releasing hormone antagonists on the expression of vascular endothelial growth factor and its receptors in a rat model of ovarian hyperstimulation syndrome. Chin Med J (Engl) 121:2434–2439
Gomez R, Gonzalez-Izquierdo M, Zimmermann RC et al (2006) Low-dose dopamine agonist administration blocks vascular endothelial growth factor (VEGF)-mediated vascular hyperpermeability with-out altering VEGF receptor 2-dependent luteal angiogenesis in a rat ovarian hyperstimulation model. Endocrinology 147:5400–5411
Alvarez C, Marti-Bonmati L, Novella-Maestre E et al (2007) Dopamine agonist capergoline reduces hemoconcentration and ascites in hyperstimulated women undergoing assisted reproduction. J Clin Endocrinol Metab 92:2931–2937
Quintana R, Kopcow L, Marconi G et al (2008) Inhibition of cyclooxygenase-2 (COX-2) by meloxicam decreases the incidence of ovarian hyperstimulation syndrome in a rat model. Fertil Steril 90:1511–1516
Hong T, Cheng S (2006) Aromatase inhibitors: structural features and biochemical characterization. Ann N Y Acad Sci 1089:237–251
Delvigne A (2009) Symposium: update on prediction and management of OHSS. Epidemiology of OHSS. Reprod Biomed Online 19(1):8–13 (review)
Hong Y, Chen S (2006) Aromatase inhibitors: structural features and biochemical characterization. Ann N Y Acad Sci 1089:237–251 (review)
He Qiaohua, Liang Linlin, Zhang Cuilian, Li Hangsheng, Zhaojia Ge Lu, Wang Shihong Cui (2014) Effects of different doses of letrozole on the incidence of early-onset ovarian hyperstimulation syndrome after oocyte retrieval. Syst Biol Reprod Med 60(6):355–360
Wang YQ, Yang J, Xu WM, Xie QZ, Yan WJ, Yin TL, Cheng D, Xiao ZN, Li J (2013) Luteal letrozole administration decreases serum estrogen level but not the risk of ovarian hyperstimulation syndrome. Beijing Da Xue Xue Bao 45(6):869–872
Kumar P, Sait SF, Sharma A, Kumar M (2011) Ovarian hyperstimulation syndrome. J Hum Reprod Sci 4(2):70–75
Soares SR, Gómez R, Simón C, García-Velasco JA, Pellicer A (2008) Targeting the vascular endothelial growth factor system to prevent ovarian hyperstimulation syndrome. Hum Reprod Update. 14(4):321–333
Chuderland D, Hasky N, Ben-Ami I, Kaplan-Kraicer R, Grossman H, Shalgi R (2013) A physiological approach for treating endometriosis by recombinant pigment epithelium-derived factor (PEDF). Hum Reprod 28(6):1626–1634
Busso CE, Garcia-Velasco J, Gomez R et al (2009) Symposium: update on prediction and management of OHSS. Prevention of OHSS–dopamine agonists. Reprod Biomed Online 19:43–51
Amir H, Yaniv D, Hasson J, Amit A, Gordon D, Azem F (2015) Cabergoline for reducing ovarian hyperstimulation syndrome in assisted reproductive technology treatment cycles. A prospective randomized controlled trial. J Reprod Med 60(1–2):48–54
Kasum M, Vrčić H, Stanić P, Ježek D, Orešković S, Beketić-Orešković L, Pekez M (2014) Dopamine agonists in prevention of ovarian hyperstimulation syndrome. Gynecol Endocrinol 5:1–5
Papanikolaou EG, Polyzos NP, Humaidan P, Pados G, Bosch E, Tournaye H, Tarlatzis B (2011) Aromatase inhibitors in stimulated IVF cycles. Reprod Biol Endocrinol 21(9):85
Garcia-Velasco JA, Quea G, Piro M et al (2009) Letrozle administration during the luteal phase after ovarian stimulation impacts corpus luteum function: a randomized, placebo-controlled trial. Fertil Steril 92:222–225
Ceyhan ST, Onguru O, Fidan U, Ide T, Yaman H, Kilic S, Baser I (2011) Comparison of aromatase inhibitor (letrozole) and immunomodulators (infliximab and etanercept) on the regression of endometriotic implants in a rat model. Eur J Obstet Gynecol Reprod Biol 154(1):100–104
Ferrero H, García-Pascual CM, Morales C, Simón C, Gaytán F, Pellicer A, Gómez R (2014) Dopamine receptor 2 activation inhibits ovarian vascular endothelial growth factor secretion in an ovarian hyperstimulation syndrome (OHSS) animal model: implications for treatment of OHSS with dopamine receptor 2 agonists. Fertil Steril 102(5):1468–1476
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Şahin, N., Apaydın, N., Töz, E. et al. Comparison of the effects of letrozole and cabergoline on vascular permeability, ovarian diameter, ovarian tissue VEGF levels, and blood PEDF levels, in a rat model of ovarian hyperstimulation syndrome. Arch Gynecol Obstet 293, 1101–1106 (2016). https://doi.org/10.1007/s00404-015-3987-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3987-4