Abstract
Background
Hysterectomies are preformed abdominally, vaginally, laparoscopic or with robotic assistance. When choosing the route of hysterectomy, the physician should take into consideration the safest and most cost-effective route to fulfill all needs of the patient.
Methods
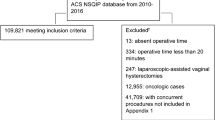
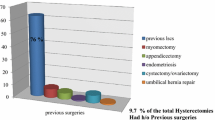
Data were collected retrospectively from 953 patients who underwent hysterectomy between 2002 and 2010 for benign indications at UKSH, Germany. Preoperative risk scores were assigned to patients. The data were statistically evaluated to investigate relationship between the occurrence of the complication and the preoperative score at the time of the hysterectomy. For the preoperative score, patients who had undergone a previous laparoscopy were assigned 1 point; those who had undergone a previous Pfannenstiel laparotomy were assigned 2 points; those who had undergone 1 cesarean delivery were assigned 3 points; those who had undergone 2 cesarean deliveries were assigned 4 points; those who had undergone 3 cesarean deliveries were assigned 5 points; and those with no previous operations were assigned 0 points. The preoperative score was recorded for 785 patients.
Results
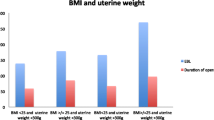
Of the 785 women with complete data, the mean preoperative score was 1.09 ± 1.51 for AH, 0.75 ± 0.96 for VH, 1.04 ± 1.30 for LSH, 1.0 ± 1.40 for LAVH, and 1.38 ± 1.52 for TLH. The prevalent scores in the VH were 0 and 1, the LASH and TLH showed a prevalence over VH in the preoperative scores 3 and 4 and AH showed a prevalence over the other methods in the preoperative score 3–8. Intraoperative complications were recorded in 28 of 953 (2.9 %) cases: 10 (35.7 %) cases of VH; 13 (46.4 %) cases of AH; 3 (10.7 %) cases of LSH; 1 (3.6 %) case of LAVH; and 1 (3.6 %) case of TLH. The intraoperative complications appeared to be more frequently with heavier uterine weight showing a significant statically correlation (P < 0,001). Major postoperative complications occurred in 17 of 953 (1.8 %) cases. Minor postoperative complications were recorded in 56 of 953 (5.9 %) hysterectomies. Operation duration, hospital stay and hemoglobin decline correlated significantly with preoperative score (P < 0.001).
Conclusion
The suggested preoperative score is apparently successful in screening out the high-risk patients, despite the low incidence of intra and postoperative complications. The usefulness of the preoperative scoring system is worthy of further development and evaluation. The AH was favored as the ‘fallback option’ with high preoperative score.
Similar content being viewed by others
References
Altgassen C, Michels W, Schneider A (2004) Learning laparoscopic-assisted hysterectomy. Obstet Gynecol 104(2):308–313
Briese V, Ulfig N, Mylonas I (2002) Die vaginale Hysterektomie. Gynäkologe 116:24
Whiteman MK, Hillis SD, Jamieson DJ, Morrow B, Podgornik MN, Brett KM et al (2008) Inpatient hysterectomy surveillance in the United States, 2000–2004. Am J Obstet Gynecol 198(1):34 e1–34 e7
Mettler L, Clevin L, Ternamian A, Puntambekar S, Schollmeyer T, Alkatout I (2013) The past, present and future of minimally invasive endoscopy in gynecology: a review and speculative outlook. Minim Invasive Ther Allied Technol 22(4):210–226
Reich H (1992) Laparoscopic hysterectomy. Surg Laparosc Endosc 2(1):85–88
Semm K (1991) Hysterektomie per laparotomiam oder per pelviskopiam. Ein neuer Weg ohne Kolpotomie durch CASH. Geburtshilfe und Frauenheilkunde 996–1003. Geburtshilfe Frauenheilkd 51(12):996–1003. doi:10.1055/s-2008-1026252
Donnez J, Nisolle M (1993) Laparoscopic supracervical (subtotal) hysterectomy (LASH). J Gynecol Surg 9(2):91–94
Brandner P, Neis KJ (1995) The significance of laparoscopically-assisted vaginal hysterectomy—LAVH. Zentralbl Gynakol 117(12):620–624
Neis KJ, Ulrich K, Zeilmann W, Brandner P (1993) Die laparoskopisch-assistierte vaginale Hysterektomie. Der Frauenarzt 1091–6. Arch Gynecol Obstet (1996) 258:55–64
Johnson N, Barlow D, Lethaby A, Tavender E, Curr E, Garry R (2006) Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 2:CD003677
Mettler L, Schollmeyer T, Alkatout I (2012) Adhesions during and after surgical procedures, their prevention and impact on women’s health. Womens Health Lond Engl 8(5):495–498
Muller A, Thiel FC, Renner SP, Winkler M, Haberle L, Beckmann MW (2010) Hysterectomy-a comparison of approaches. Deutsches Arzteblatt Int 107(20):353–359
Radosa MP, Meyberg-Solomayer G, Radosa J, Vorwergk J, Oettler K, Mothes A et al (2014) Standardised registration of surgical complications in laparoscopic-gynaecological therapeutic procedures using the clavien-dindo classification. Geburtshilfe Frauenheilkd 74(8):752–758
Canis MJ, Wattiez A, Mage G, Bruhat MA (2004) Results of eVALuate study of hysterectomy techniques: laparoscopic hysterectomy may yet have a bright future. BMJ 328(7440):642–643 author reply 3
McPherson K, Metcalfe MA, Herbert A, Maresh M, Casbard A, Hargreaves J et al (2004) Severe complications of hysterectomy: the VALUE study. BJOG Int J Obstet Gynaecol 111(7):688–694
Brummer TH, Jalkanen J, Fraser J, Heikkinen AM, Kauko M, Makinen J et al (2011) FINHYST, a prospective study of 5279 hysterectomies: complications and their risk factors. Hum Reprod 26(7):1741–1751
Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R et al (2009) Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 3:CD003677
Schindlbeck C, Klauser K, Dian D, Janni W, Friese K (2008) Comparison of total laparoscopic, vaginal and abdominal hysterectomy. Arch Gynecol Obstet 277(4):331–337
Wallwiener M, Taran FA, Rothmund R, Kasperkowiak A, Auwarter G, Ganz A et al (2013) Laparoscopic supracervical hysterectomy (LSH) versus total laparoscopic hysterectomy (TLH): an implementation study in 1,952 patients with an analysis of risk factors for conversion to laparotomy and complications, and of procedure-specific re-operations. Arch Gynecol Obstet 288(6):1329–1339
Hillis SD, Marchbanks PA, Peterson HB (1996) Uterine size and risk of complications among women undergoing abdominal hysterectomy for leiomyomas. Obstet Gynecol 87(4):539–543
Bachmann C, Abele H, Wallwiener D, Kagan KO (2014) Neonatal and maternal risk in Hermansky-Pudlak syndrome: peripartum management-brief report and review of literature. Arch Gynecol Obstet 289(6):1193–1195
Mueller A, Boosz A, Koch M, Jud S, Faschingbauer F, Schrauder M et al (2012) The Hohl instrument for optimizing total laparoscopic hysterectomy: results of more than 500 procedures in a university training center. Arch Gynecol Obstet 285(1):123–127
Ou CS, Joki J, Wells K, Zabriske V, Hamilton K, Tsuang M et al (2004) Total laparoscopic hysterectomy using multifunction grasping, coagulating, and cutting forceps. J Laparoendosc Adv Surg Tech A 14(2):67–71
Conflict of interest
We confirm that there are no instances of conflict of interest in our manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is dedicated to Dr. M. Ibrahim and PD. Dr. T. Schollmeyer who taught me that the best kind of knowledge to have is that which is learned for its own sake.
Rights and permissions
About this article
Cite this article
Elessawy, M., Schollmeyer, T., Mettler, L. et al. The incidence of complications by hysterectomy for benign disease in correlation to an assumed preoperative score. Arch Gynecol Obstet 292, 127–133 (2015). https://doi.org/10.1007/s00404-014-3594-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3594-9