Abstract
Objective
To compare efficacy and safety of vaginal misoprostol (PGE1 analog) with dinoprostone (PGE2 analog) vaginal insert for labor induction in term pregnancies.
Study design
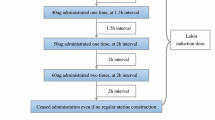
A total of 112 women with singleton pregnancies of ≥37 weeks of gestation, and low Bishop scores underwent labor induction. The subjects were randomized to receive either 50 μg misoprostol intravaginally every 4 h to a maximum of five doses or a 10 mg dinoprostone vaginal insert for a maximum of 12 h. Time interval from induction to vaginal delivery, vaginal delivery rates within 12 and 24 h, requirement of oxytocin augmentation, incidence of tachysystole and uterine hyperstimulation, mode of delivery, rate of cesarean section due to fetal distress and neonatal outcome were outcome measures. Student’s t test, Chi square test, Fischer’s exact test were used for statistical analysis.
Results
Time interval from induction to vaginal delivery was found to be significantly shorter in misoprostol group when compared to dinoprostone subjects (680 ± 329 min vs. 1070 ± 435 min, P < 0.001). Vaginal delivery rates within 12 h were found to be significantly higher with misoprostol induction [n = 37 (66%) vs. n = 25 (44.6%); P = 0.02], whereas vaginal delivery rates in 24 h did not differ significantly between groups [n = 41 (73.2%) vs. n = 36 (64.2%); P = 0.3]. More subjects required oxytocin augmentation in dinoprostone group [n = 35 (62.5%) vs. n = 20 (35.7%), P = 0.005] and cardiotocography tracings revealed early decelerations occurring more frequently with misoprostol induction (10.7 vs. 0%, P = 0.03). Tachysystole and uterine hyperstimulation, mode of delivery, rate of cesarean sections due to fetal distress and adverse neonatal outcome were not demonstrated to be significantly different between groups (P = 1, P = 0.5, P = 0.4, P = 0.22, P = 0.5).
Conclusion
Using vaginal misoprostol is an effective way of labor induction in term pregnant women with unfavorable cervices, since it is associated with a shorter duration of labor induction and higher rates of vaginal delivery within 12 h. Misoprostol and dinoprostone are equally safe, since misoprostol did not result in a rise in maternal and neonatal morbidity, namely, tachysystole, uterine hyperstimulation, cesarean section rates and admission to neonatal intensive care units as reported previously in literature.
Similar content being viewed by others
References
Dällenbach P, Boulvain M, Viardot C, Irion O (2003) Oral misoprostol or vaginal dinoprostone for labor induction: a randomized controlled trial. Am J Obstet Gynecol 188:162–167. doi:10.1067/mob.2003.108
Langenegger EJ, Odendaal HJ, Grove D (2005) Oral misoprostol versus intracervical dinoprostone for induction of labor. Int J Gynaecol Obstet 88:242–248. doi:10.1016/j.ijgo.2004.12.005
Agarwal N, Gupta A, Kriplan A, Bhatla N (2003) Six hourly vaginal misoprostol versus intracervical dinoprostone for cervical ripening and labor induction. J Obstet Gynaecol Res 29(3):147–151. doi:10.1046/j.1341-8076.2003.00091.x
Gregson S, Waterstone M, Norman I, Murrels T (2005) A randomised controlled trial comparing low dose vaginal misoprostol and dinoprostone vaginal gel for inducing labour at term. BJOG An Int J Obstet Gynaecol 112:438–444. doi:10.1111/j.1471-0528.2004.00496.x
van Gemund N, Scherjon S, le Cessie S, van Leeuwen SJH, van Roosmaln J, Kanhai HHH (2004) A randomised trial comparing low dose vaginal misoprostol and dinoprostone for labour induction. BJOG An Int J Obstet Gynaecol 111:42–49. doi:10.1046/j.1471-0528.2003.00010.x
Chang YK, Chen H, Yu MH, Liu HS (2003) Intracervical misoprostol and prostaglandin E2 for labor induction. Int J Gynaecol Obstet 80:23–28. doi:10.1016/S0020-7292(02)00333-8
Sanchez-Ramos L, Kaunitz AM, Delke I, Gaudier FL (1999) Cervical ripening and labor induction with a controlled release dinoprostone vaginal insert: a meta-analysis. Obstet Gynecol 94:878–883. doi:10.1016/S0029-7844(99)00320-8
Garry D, Figueroa R, Kalish RB, Catalano CJ, Maulik D (2003) Randomized controlled trial of vaginal misoprostol versus dinoprostone vaginal insert for labor induction. J Matern Fetal Neonatal Med 13:254–259. doi:10.1080/713605867
Sanchez-Ramos L, Kaunitz AM (2000) Misoprostol for cervical ripening and labor induction: a systematic review of the literature. Clin Obstet Gynecol 43:475–488. doi:10.1097/00003081-200009000-00008
Sanchez-Ramos L, Kaunitz AM, Wears RL, Delke I, Gaudier FL (1997) Misoprostol for cervical ripening and labor induction: a meta-analysis. Obstet Gynecol 89:633–642. doi:10.1016/S0029-7844(96)00374-2
Wing DA (1999) Labor induction with misoprostol. Am J Obstet Gynecol 181:339–345. doi:10.1016/S0002-9378(99)70558-2
Rosenberg P, Chevret S, Senat MV et al (2004) A randomized trial that compared intravaginal misoprostol and dinoprostone vaginal insert in pregnancies at high risk of fetal distress. Am J Obstet Gynecol 191:247–253. doi:10.1016/j.ajog.2003.12.038
Shetty A, Livingstone I, Acharya A, Rice P, Danielian P, Templeton A (2004) A randomised comparison of oral misoprostol and vaginal prostaglandin E2 tablets in labour induction at term. BJOG An Int J Obstet Gynaecol 111:436–440. doi:10.1111/j.1471-0528.2004.00107.x
Megalo A, Petignat P, Hahlfeld P (2004) Influence of misoprostol or prostaglandin E2 for induction of labor on the incidence of pathological CTG tracing: a randomized trial. Eur J Obstet Gynecol Reprod Biol 116:34–38. doi:10.1016/j.ejogrb.2004.01.038
American College of Obstetricians and Gynecologists (1995) Induction of labor. ACOG Technical Bulletin No.217, ACOG, Washington, DC
Garite TJ, Dildy GA, McNamara H et al (2000) A multicenter controlled trial of fetal pulse oximetry in the intrapartum management of nonreassuring fetal heart rate patterns. Am J Obstet Gynecol 183(5):1049–1058. doi:10.1067/mob.2000.110632
Sanchez-Ramos L, Kaunitz AM, Del Vale GO, Delke I, Schoeder P (1993) Labor induction with the prostaglandin E1 methyl analogue misoprostol versus oxytocin: a randomized trial. Obstet Gynecol 81:332–336
Wing DA, Jones MM, Rahall A, Goodwin TM, Paul RH (1995) A comparison of misoprostol and prostaglandin E2 gel for preinduction cervical ripening and labor induction. Am J Obstet Gynecol 172:1804–1810. doi:10.1016/0002-9378(95)91415-3
Leukomage AU, Forsyth SF, Sullivan KR, El Refaey H, Rodeck CH (2003) Dinoprostone versus misoprostol. A randomized study of nulliparous women undergoing induction of labor. Acta Obstet Gynecol Scand 82:133–137. doi:10.1034/j.1600-0412.2003.00066.x
Hughes EG, Kelly AJ, Kavanagh J (2001) Dinoprostone vaginal insert for cervical ripening and labor induction: a metaanalysis. Obstet Gynecol 97:847–855. doi:10.1016/S0029-7844(00)01216-3
Le Roux PA, Olaragun JO, Penny J, Anthony J (2002) Oral and vaginal misoprostol compared with dinoprostone for induction of labor: a randomized controlled trial. Obstet Gynecol 99:201–205. doi:10.1016/S0029-7844(01)01681-7
Buser D, Mora G, Arias F (1997) A randomized comparison between misoprostol and dinoprostone for cervical ripening and labor induction in patients with unfavorable cervices. Obstet Gynecol 89:581–585. doi:10.1016/S0029-7844(97)00015-X
Yip SK, Tse AO, Haines CJ, Chung TK (2000) Misoprostol’s effect on uterine arterial blood flow and fetal heart rate in early pregnancy. Obstet Gynecol 95:232–235. doi:10.1016/S0029-7844(99)00472-X
Chen WH, Lai HC, Tang YH, Liu HS (1999) Fetal Doppler hemodynamic changes in spontaneous versus prostaglandin induced active labor. Acta Obstet Gynecol Scand 78:599–604. doi:10.1034/j.1600-0412.1999.780707.x
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Özkan, S., Çalışkan, E., Doğer, E. et al. Comparative efficacy and safety of vaginal misoprostol versus dinoprostone vaginal insert in labor induction at term: a randomized trial. Arch Gynecol Obstet 280, 19–24 (2009). https://doi.org/10.1007/s00404-008-0843-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-008-0843-9