Abstract
Introduction
The present study aimed to investigate differences in survivorship between medial and lateral unicompartmental knee arthroplasty (UKA) by analyzing the data of an Italian regional registry. The hypothesis was that, according to recent literature, lateral implants have comparable survivorship with regard to the medial implants.
Materials and methods
The Register of Orthopaedic Prosthetic Implants (RIPO) of Emilia-Romagna (Italy) database was searched for all UKAs between July 1, 2000, and December 31, 2019. For both cohorts, subject demographics and reasons for revision were presented as a percentage of the total cohort. Kaplan–Meier survivorship analysis was performed using revision of any component as the endpoint and survival times of unrevised UKAs taken as the last observation date (December 31, 2019, or date of death).
Results
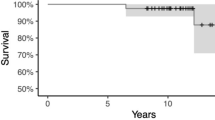
Patients living outside the region and symmetrical implants (which do not allow the compartment operated to be traced) were excluded. 5571 UKAs implanted on 5172 patients (5215 medial UKAs and 356 lateral UKAs) were included in the study. The survivorship analysis revealed 13 failures out of 356 lateral UKAs (3.7%) at a mean follow-up of 6.3 years and 495 failures out of 5215 medial UKAs (9.5%) at a mean follow-up of 6.7 years. The medial UKAs had a significantly higher risk of failure, with a Hazard Ratio of 2.6 (CI 95% 1.6–4.8; p < 0.001), adjusted for age, gender, weight, and mobility of the insert. Both the groups revealed a good survival rate, with 95.2% of lateral implants and 87.5% of medial implants still in situ at 10 years of follow-up.
Conclusions
Lateral UKA is a safe procedure showing longer survivorship than medial UKAs (95.2% and 87.5% at 10 years, respectively) in the present study.
Level of evidence
Level 3, therapeutic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unicompartimental knee arthroplasty (UKA) is a viable alternative to total knee arthroplasty (TKA) in patients with both medial or lateral isolated knee osteoarthritis [1]. UKA has several potential advantages over TKA, which include improved postoperative outcomes, a less invasive procedure, preservation of bone stock and ligamentous structures, improved proprioception, earlier return to activities, shorter hospital stay, and generally a higher patient satisfaction with fewer complications [2,3,4,5,6].
Fewer lateral UKAs are implanted each year in comparison to medial ones. This is mainly due to the higher prevalence of isolated medial knee osteoarthritis, with studies reporting that medial UKAs are performed ten times more often than lateral UKA [7]. Therefore, studies analyzing lateral UKA have smaller sample sizes and the literature provides limited information; moreover, registry studies often analyze the survival of UKA, not separating medial and lateral implants and are mainly focused on comparing UKA and TKA, regardless of laterality [8, 9].
Medial and lateral compartments should be instead considered separately, given the different anatomy, biomechanics, and weight loads [10]. The convexity of the lateral tibial plateau and the C-shaped lateral meniscus provide wider mobility to the lateral compartment than the medial side. Therefore, the lateral femoral condyle articulates with the posterior tibial plateau in deep flexion. Moreover, the femoral rollback is greater, and the screw-home mechanism is far more significant on the lateral side [11]. These differences lead to considering that UKA ideally requires different positioning and implants for medial and lateral compartments. This behavior could be appreciated in the early mobile-bearing UKA design where the flat tibial component, similar to the medial anatomy, had a higher risk of bearing dislocation when implanted laterally [12].
Medial implants were historically considered at a lower risk of failure, for the higher complexity of lateral compartment biomechanics and the scarcity of studies investigating lateral UKAs designs and positioning [13]. Only few case series analyzed differences in outcomes and survivorship between lateral and medial UKA, and no consensus exists about the topic, with some series reporting inferior survivorship for lateral implants and others highlighting worse function for medial UKAs [14]. Moreover, a recent meta-analysis by Seung-Beom Han et al. found that short- to mid-term and long-term survival did not significantly differ between medial and lateral UKAs [13].
The Register of Prosthetic Orthopedic Implants (RIPO) of Emilia-Romagna is a large regional implant registry in Italy, firstly introduced at Istituto Ortopedico Rizzoli in 1990 and later expanded to the whole Emilia-Romagna region since 2000, including more than 4 million people [15]. The present study aimed to investigate differences in survivorship between medial and lateral UKA by analyzing the data of this regional Italian registry. The hypothesis was that, according to recent literature, lateral implants have comparable survivorship to the medial implants.
Methods
The Register of Orthopaedic Prosthetic Implants (RIPO) database was searched for all UKAs between July 1, 2000, and December 31, 2019. The RIPO was established at the Istituto Ortopedico Rizzoli in Bologna and collects data related to hip, knee, and shoulder arthroplasty procedures (primary and revision surgeries) performed in the Emilia-Romagna region (Italy) since 2000.
UKAs were excluded if they were implanted in patients outside the Emilia-Romagna region to minimize bias due to loss to follow-up. For residents of the Emilia-Romagna region, any treatment received in other regions of Italy is billed back to the Emilia-Romagna region and therefore captured in the registry.
For both cohorts, subject demographics and reasons for revision were presented as a percentage of the total cohort. Patient age and weight were compared using a t-test, side operated, gender and mobility of the insert were compared using Fisher test, while indication for surgery, femur and insert material, and fixation were compared using chi-square analysis. Differences between the groups were considered statistically significant if the p value was less than 0.05. Kaplan–Meier survivorship analysis was performed using revision of any component as the endpoint and survival times of unrevised UKAs taken as the last observation date (December 31, 2019, or date of death). The Wilcoxon Test test was used to compare survivorship between the two groups. The Cox multiple regression model for analyzing survival data was considered. The proportionality hazards assumption was tested by the Schoenfeld residual method.
The statistical analysis was performed using SPSS 14.0 for Windows, version 14.0.1 (SPSS Inc, Chicago, IL, USA) and JMP, Version 12.0.1 (SAS Institute Inc., Cary, NC, 1989–2007).
Ethics approval was not necessary as the data were collected from a registry in Italy that collects data as standard practice on all patients in their region. Additionally, all data were collected and analyzed in a de-identified format that protects patient privacy.
Results
The present registry analysis collected data from 7568 UKAs performed between July 2000 and December 2019 on patients resident in the Emilia-Romagna region. Patients living outside the region were excluded to avoid the bias of possible lost follow-up. After excluding 1997 symmetrical implants which, as they could be used indiscriminately for the medial and lateral femoro-tibial compartment, did not allow the compartment operated to be traced, 5571 UKAs implanted on 5172 patients were included in the study. 5215 medial UKAs and 356 lateral UKAs were present in this cohort.
Analyzing the total number of procedures performed by year of surgery and compartment treated, from 2000 to 2019, lateral UKAs account for 6.4% and medial UKAs for 93.6% of the total, with a progressive increase in the total number of patients treated over the years.The demographics of the two groups are shown in Table 1.
Statistically significant differences were identified for knee laterality, gender, age, weight, diagnosis, and insert type. The main causes of UKA implant were primary osteoarthritis followed by axial malalignment and osteonecrosis.
The survivorship analysis revealed 13 failures out of 356 lateral UKAs (3.7%) at a mean follow-up of 6.3 years and 495 failures out of 5215 medial UKAs (9.5%) at mean follow-up of 6.7 years. The medial UKA had a significantly higher risk of failure, with a Hazard Ratio of 2.6 (CI 95% 1.6–4.8; p < 0.001), adjusted for age, gender, weight, and mobility of the insert.
The survivorship per year for each group is reported in Table 2 and graphically represented in the Kaplan–Meier diagram in Fig. 1. Both the groups revealed a good survival rate, with 95.2% of lateral implants and 87.5% of medial implants still in situ at 10 years of follow-up.
The main causes of revision were, as follows, aseptic loosening (23.1% and 38.0% for lateral and medial UKAs, respectively), pain without loosening (23.1% and 22.6%), and septic loosening (6.5% for medial UKAs). In the present cohort, no case of septic loosening was reported for the lateral UKAs. The detailed information about causes of revision was reported in Table 3.
3 patients with prior medial UKA implanted subsequently underwent lateral UKA, and two patients underwent patellofemoral implant after medial UKA; although the reoperations, these patients were not considered failures for the purposes of the study.
Discussion
The main finding of the present study was that the survival rate at 10 years of follow-up was significantly higher for lateral UKAs with respect to medial UKAs. Interestingly, the literature provides conflicting results on the topic. Articles that evaluated the survival of isolated lateral UKAs reported satisfactory results. Deroche et al. showed high survivorship at long term (mean follow-up of 17 years) for lateral UKAs, with a survival rate of 82.1% at 15 years [16]. The same author also participated in a multicenter study that showed very good overall survival rate (85.4% at 10 years among 268 lateral UKAs), considering the long follow-up period and older techniques used in the early years, such as anterior tibial tubercle osteotomies [17]. This can explain the lower results in comparison with the series presented in the current study, which showed a better survival rate of 92.7% for lateral UKAs at 13 years of follow-up. Other studies, however, show no difference among medial and lateral UKA survivorship. A recent metanalysis by Han et al. showed no significant differences in the survival of lateral UKAs compared to medial UKAs [13]. A systematic review by Van der List et. al. reported no significative difference in survivorship and revision rates, however pointing out overall lower implant survivorship in registry studies (90.5% vs 84.1% combined UKA survivorship at 10 years for cohort and registry studies respectively) [18]. According to the authors, this latter statement can be explained with cohort studies being often performed in high volume centers, whereas registry-based studies also report low-volume center outcomes. In studies comparing outcomes in high-volume centers with low-volume centers, better results can be found in the first ones [19, 20].
No recent studies can be found showing higher survivorship for medial UKAs compared to lateral UKAs. Those results could be explained by the different behavior of the lateral knee side compared to the medial. During deep flexion, the medial compartment stays relatively static on the anteroposterior (AP) plane, with 1.5 mm of translation, while the lateral side has an intrinsic instability with a greater degree of freedom and translations that can vary between 9 and 15 mm [21, 22]. Moreover, the lateral compartment is less involved in weight transmission, both during stance and walking phase [23, 24].
Historically, the reasons for worse survival of lateral UKAs were the more complex surgical technique and the poor knowledge of lateral knee osteoarthritis and kinematics, which led surgeons having limited experience in implanting lateral UKAs. The surgeon learning curve for the lateral side is steeper than the one for the medial, and, all factors considered, there is an essential difference among the same procedures performed by different surgeons. One of the factors that justify the controversies found in literature is the surgeon experience, given that the number of lateral UKAs performed plays an important factor in optimizing outcomes and survivorship.
Many authors underline, when explaining potential causes of failure of lateral UKAs, how it is important to perform a different surgical technique in comparison to the medial side [17, 18, 25], minimizing tibial cuts and internally rotating the sagittal cuts to avoid impingement between the femoral component and the tibial spine in extension [26, 27]. Moreover, the femoral component should be placed as lateral as possible to avoid unwanted translations in extension induced by the “screw-home” mechanism, and the tibial slope should be neutral to respect the normal anatomy, which again differs from the medial compartment [28].
Another factor that could influence the survivorship of lateral UKAs is the more recent design development of such implants regarding the medial side, with the latter available on the market for a more extended period. However, additional time will be needed to prove it statistically [18].
This study has some limitations, mainly because the data included in the RIPO registry are standardized but not complete, no information about the subjective outcomes are collected, and it only includes cases from the region Emilia-Romagna. However, the RIPO records UKA implants specificities differently from other registries, allowing us to discriminate, for example, from medial to lateral prostheses. Lastly, as per every registry study, one of the most valuable features is the vast number of procedures evaluated, which is very difficult to match in trials and case series.
Given actual evidence and data collected from the present large cohort, lateral UKA is a safe procedure and can be confidently proposed to patients with isolated lateral knee osteoarthritis and intact ligaments.
Conclusions
Lateral UKA is a safe procedure showing longer survivorship than medial UKAs (95,2% and 87,5% at 10 years, respectively) in the present study and can be confidently proposed to the patients with isolated lateral knee osteoarthritis and intact ligaments.
References
Johal S, Nakano N, Baxter M et al (2018) Unicompartmental knee arthroplasty: the past, current controversies, and future perspectives. J Knee Surg 31:992–998
Isaac SM, Barker KL, Danial IN et al (2007) Does arthroplasty type influence knee joint proprioception? A longitudinal prospective study comparing total and unicompartmental arthroplasty. Knee 14:212–217
Laurencin CT, Zelicof SB, Scott RD, Ewald FC (1991) Unicompartmental versus total knee arthroplasty in the same patient. A comparative study. Clin Orthop 273:151–156
Lombardi AV, Berend KR, Walter CA et al (2009) Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clin Orthop 467:1450–1457
Smith TO, Chester R, Glasgow MM, Donell ST (2012) Accelerated rehabilitation following Oxford unicompartmental knee arthroplasty: five-year results from an independent centre. Eur J Orthop Surg Traumatol 22:151–158
Walker T, Gotterbarm T, Bruckner T et al (2014) Total versus unicompartmental knee replacement for isolated lateral osteoarthritis: a matched-pairs study. Int Orthop 38:2259–2264
Fiocchi A, Condello V, Madonna V et al (2017) Medial vs lateral unicompartmental knee arthroplasty: clinical results. Acta Bio Medica Atenei Parm 88:38–44
Di Martino A, Bordini B, Barile F et al (2021) Unicompartmental knee arthroplasty has higher revisions than total knee arthroplasty at long term follow-up: a registry study on 6453 prostheses. Knee Surg Sports Traumatol Arthrosc 29:3323–3329
Wilson HA, Middleton R, Abram SGF et al (2019) Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis. The BMJ 364:l352
Kumar D, Manal KT, Rudolph KS (2013) Knee joint loading during gait in healthy controls and individuals with knee osteoarthritis. Osteoarthritis Cartilage 21:298–305
Asano T, Akagi M, Tanaka K et al (2001) In vivo three-dimensional knee kinematics using a biplanar image-matching technique. Clin Orthop 388:157–166
Gunther TV, Murray DW, Miller R et al (1996) Lateral unicompartmental arthroplasty with the Oxford meniscal knee. Knee 3:33–39
Han S-B, Lee S-S, Kim K-H et al (2020) Survival of medial versus lateral unicompartmental knee arthroplasty: a meta-analysis. PLoS One 15:e0228150
Ernstbrunner L, Imam MA, Andronic O et al (2018) Lateral unicompartmental knee replacement: a systematic review of reasons for failure. Int Orthop 42:1827–1833
R.I.P.O. Register - Aims of the Register - http://ripo.cineca.it/authzssl/Aims_of_the_register.html. Accessed 20 Jan 2022
Deroche E, Batailler C, Lording T et al (2019) High survival rate and very low wear of lateral unicompartmental arthroplasty at long term: a case series of 54 cases at a mean follow-up of 17 years. J Arthroplasty 34:1097–1104
Deroche E, Martres S, Ollivier M et al (2020) Excellent outcomes for lateral unicompartmental knee arthroplasty: multicenter 268-case series at 5 to 23 years’ follow-up. Orthop Traumatol Surg Res OTSR 106:907–913
van der List JP, McDonald LS, Pearle AD (2015) Systematic review of medial versus lateral survivorship in unicompartmental knee arthroplasty. Knee 22:454–460
Badawy M, Espehaug B, Indrekvam K et al (2014) Higher revision risk for unicompartmental knee arthroplasty in low-volume hospitals. Acta Orthop 85:342–347
Baker P, Jameson S, Critchley R et al (2013) Center and surgeon volume influence the revision rate following unicondylar knee replacement: an analysis of 23,400 medial cemented unicondylar knee replacements. J Bone Joint Surg Am 95:702–709
James EW, LaPrade CM, LaPrade RF (2015) Anatomy and biomechanics of the lateral side of the knee and surgical implications. Sports Med Arthrosc Rev 23:2–9
Scott CEH, Nutton RW, Biant LC (2013) Lateral compartment osteoarthritis of the knee. Bone Jt J 95-B:436–444. https://doi.org/10.1302/0301-620X.95B4.30536
Flandry F, Hommel G (2011) Normal anatomy and biomechanics of the knee. Sports Med Arthrosc Rev 19:82–92
Morrison JB (1970) The mechanics of the knee joint in relation to normal walking. J Biomech 3:51–61
Lustig S, Lording T, Frank F et al (2014) Progression of medial osteoarthritis and long term results of lateral unicompartmental arthroplasty: 10 to 18 year follow-up of 54 consecutive implants. Knee 21(Suppl 1):S26-32
Deschamps G, Chol C (2011) Fixed-bearing unicompartmental knee arthroplasty. Patients’ selection and operative technique. Orthop Traumatol Surg Res OTSR 97:648–661
Hernigou P, Deschamps G (2002) Patellar impingement following unicompartmental arthroplasty. J Bone Joint Surg Am 84:1132–1137
Ollivier M, Abdel MP, Parratte S, Argenson J-N (2014) Lateral unicondylar knee arthroplasty (UKA): contemporary indications, surgical technique, and results. Int Orthop 38:449–455
Funding
Open access funding provided by Alma Mater Studiorum - Università di Bologna within the CRUI-CARE Agreement. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or proprietary interests in any material discussed in this article.
Ethical approval
This is a registry study. The CE AVEC Research Ethics Committee has confirmed that no ethical approval is required.
Informed consent
Not required as this is a register study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alesi, D., Bordini, B., Fratini, S. et al. Lateral unicompartmental knee arthroplasty (UKA) showed a lower risk of failure compared to medial unicompartmental knee arthroplasty in the Register of Prosthetic Orthopedic Implants (RIPO). Arch Orthop Trauma Surg 143, 3363–3368 (2023). https://doi.org/10.1007/s00402-022-04631-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04631-x