Abstract
Background
Unsatisfactory alignment in unicompartmental knee arthroplasty (UKA) is one potential cause of postoperative failure. Patient-specific instruments (PSIs) are designed to improve the alignment of the prostheses, but the effect of PSIs on the alignment or clinical outcome is controversial and lacks validated evidence. We conducted a meta-analysis and systematic review to determine the effect of PSIs on UKA outcomes for the first time.
Materials and methods
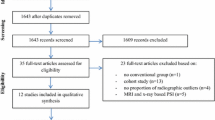
A systematic literature search in MEDLINE, EMBASE, CNKI (Chinese database) and Cochrane Central Register of Controlled Trials (up to June 2019) was performed to collect studies that compared PSIs with conventional instruments. Two reviewers independently screened all the records on the basis of inclusion and exclusion criteria. Quality assessments with Cochrane’s quality assessment tool or Newcastle–Ottawa scale (NOS) were conducted, the data were extracted, and statistical analyses were completed.
Results
Ten studies with 444 knees were included. The meta-analysis confirmed that PSIs contributed to reduced errors in the alignment of the femoral compartment in the sagittal plane (mean difference = − 2.53, CI [− 3.14, − 1.99], P < 0.01) and the tibial compartment in both the coronal (mean difference = − 0.97, CI [− 1.44, − 0.49], P < 0.01) and the sagittal plane (mean difference = − 1.29, CI [− 1.81, − 0.76], P < 0.01). One study supported that PSIs reduced outliers in inexperienced surgeons; however, all studies investigating PSIs among experienced surgeons suggested that PSIs cannot reduce the percentage of outliers. There was no significant difference in the postoperative score (mean difference = − 0.06, CI [− 0.36, 0.23], P = 0.68) or rate of complications (RR = 1.02, CI [0.15, 6.79], P = 0.99) between PSIs and conventional instruments.
Conclusion
The findings of this study suggest PSIs could not reduce the percentage of outliers in UKA patients for experts, and postoperative scores and complication rates are not improved by PSIs, compared with conventional instruments. Based on this meta-analysis and systematic review, no practical benefit to UKAs in experts was detected in PSIs. The findings of this study also suggest that PSIs improved alignment of UKA and might be beneficial to inexperienced surgeons, but it is still unclear whether this improvement is clinically significant and the evidence of inexperienced surgeons is limited. Therefore, more high-quality RCTs are need to be carried out in the future.




Similar content being viewed by others
References
Hansen EN, Ong KL, Lau E, Kurtz SM, Lonner JH (2019) Unicondylar knee arthroplasty has fewer complications but higher revision rates than total knee arthroplasty in a study of large United States databases. J Arthroplasty 34(8):1617–1625. https://doi.org/10.1016/j.arth.2019.04.004
Jones GG, Kotti M, Wiik AV, Collins R, Brevadt MJ, Strachan RK, Cobb JP (2016) Gait comparison of unicompartmental and total knee arthroplasties with healthy controls. The Bone Jt J 98-B(10 Supple B):16–21. https://doi.org/10.1302/0301-620X.98B10.BJJ.2016.0473.R1
Liddle AD, Pandit H, Judge A, Murray DW (2015) Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. The Bone Jt J 97B(6):793–801. https://doi.org/10.1302/0301-620X.97B6.35155
Dagneaux L, Bourlez J, Degeorge B, Canovas F (2017) Return to sport after total or unicompartmental knee arthroplasty: an informative guide for residents to patients. EFORT Open Rev 2(12):496–501. https://doi.org/10.1302/2058-5241.2.170037
Arirachakaran A, Choowit P, Putananon C, Muangsiri S, Kongtharvonskul J (2015) Is unicompartmental knee arthroplasty (UKA) superior to total knee arthroplasty (TKA)? A systematic review and meta-analysis of randomized controlled trial. Eur J Orthop Surg Traumatol 25(5):799–806. https://doi.org/10.1007/s00590-015-1610-9
Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD (2018) Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: a systematic review. Knee Surg Sports Traumatol Arthrosc 26(6):1811–1822. https://doi.org/10.1007/s00167-017-4817-y
Hernigou P, Deschamps G (2004) Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clin Orthop Relat Res 423:161–165. https://doi.org/10.1097/01.blo.0000128285.90459.12
Zhu GD, Guo WS, Zhang QD, Liu ZH, Cheng LM (2015) Finite element analysis of mobile-bearing unicompartmental knee arthroplasty: the influence of tibial component coronal alignment. Chin Med J 128(21):2873–2878. https://doi.org/10.4103/0366-6999.168044
Jeschke E, Gehrke T, Gunster C, Hassenpflug J, Malzahn J, Niethard FU, Schrader P, Zacher J, Halder A (2016) Five-year survival of 20,946 unicondylar knee replacements and patient risk factors for failure: an analysis of german insurance data. J Bone Jt Surg Am 98(20):1691–1698. https://doi.org/10.2106/jbjs.15.01060
Hernigou P, Deschamps G (2004) Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J B Jt Surg Am 86(3):506–511. https://doi.org/10.2106/00004623-200403000-00007
Kang KT, Son J, Kwon SK, Kwon OR, Koh YG (2018) Preservation of femoral and tibial coronal alignment to improve biomechanical effects of medial unicompartment knee arthroplasty: computational study. Bio Med Mater Eng 29(5):651–664. https://doi.org/10.3233/bme-181015
Barbadoro P, Ensini A, Leardini A, d'Amato M, Feliciangeli A, Timoncini A, Amadei F, Belvedere C, Giannini S (2014) Tibial component alignment and risk of loosening in unicompartmental knee arthroplasty: a radiographic and radiostereometric study. Knee Surg Sports Traumatol Arthrosc 22(12):3157–3162. https://doi.org/10.1007/s00167-014-3147-6
Dalton DM, Burke TP, Kelly EG, Curtin PD (2016) Quantitative analysis of technological innovation in knee arthroplasty: using patent and publication metrics to identify developments and trends. J Arthroplasty 31(6):1366–1372. https://doi.org/10.1016/j.arth.2015.12.031
Boyd JL, Kurtenbach CA, Sikka RS (2014) Patient-specific instrumentation and return to activities after unicondylar knee arthroplasty. Clin Sports Med 33(1):133–148. https://doi.org/10.1016/j.csm.2013.08.003
Jones GG, Clarke S, Jaere M, Cobb J (2018) 3D printing and unicompartmental knee arthroplasty. Efort Open Rev 3(5):248–253. https://doi.org/10.1302/2058-5241.3.180001
Hafez MA, Moholkar K (2017) Patient-specific instruments: advantages and pitfalls. SICOT J 3:66. https://doi.org/10.1051/sicotj/2017054
Liddle AD, Pandit H, Judge A, Murray DW (2016) Effect of surgical caseload on revision rate following total and unicompartmental knee replacement. J Bone Jt Surg Am 98(1):1–8. https://doi.org/10.2106/JBJS.N.00487
Hamilton WG, Ammeen D, Engh CA Jr, Engh GA (2010) Learning curve with minimally invasive unicompartmental knee arthroplasty. J Arthroplasty 25(5):735–740. https://doi.org/10.1016/j.arth.2009.05.011
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC, Grp CBM, Grp CSM (2011) The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:D5928. https://doi.org/10.1136/Bmj.D5928
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Bonett DG (2009) Meta-analytic interval estimation for standardized and unstandardized mean differences. Psychol Methods 14(3):225–238. https://doi.org/10.1037/a0016619
Alvand A, Khan T, Jenkins C, Rees JL, Jackson WF, Dodd CAF, Murray DW, Price AJ (2018) The impact of patient-specific instrumentation on unicompartmental knee arthroplasty: a prospective randomised controlled study. Knee Surg Sports Traumatol Arthrosc 26(6):1662–1670
Cai JF, Ma M, Zeng W, Luo SL, Yuan F, Zhou W, Yang S, Wang H, Yin F (2017) Accuracy of individualized custom femoral cutting guides in unicompartmental knee arthroplasty of femoral specimens. Chin J Anat Clin 22(5):373–377. https://doi.org/10.3760/cma.j.issn.2095-7041.2017.05.005[Chinese]
Fan ZQ, Nie Y, Fu DL, Liu SY, Li L, Li YF, Zhang F (2018) Cinical application of 3D printing plate in unicompartmental knee arthroplasty. Chin J Gene Prac 16(7):1085–1087 [Chinese]
Jaffry Z, Masjedi M, Clarke S, Harris S, Karia M, Andrews B, Cobb J (2014) Unicompartmental knee arthroplasties: robot vs. patient specific instrumentation. Knee 21(2):428–434
Jones GG, Logishetty K, Clarke S, Collins R, Jaere M, Harris S, Cobb JP (2018) Do patient-specific instruments (PSI) for UKA allow non-expert surgeons to achieve the same saw cut accuracy as expert surgeons? Arch Orthop Trauma Surg 138(11):1601–1608
Kerens B, Schotanus MG, Boonen B, Kort NP (2015) No radiographic difference between patient-specific guiding and conventional Oxford UKA surgery. Knee Surg Sports Traumatol Arthrosc 23(5):1324–1329. https://doi.org/10.1007/s00167-014-2849-0
Li XW, Ding J, Gan YD (2018) Application of individualized navigation template in the location of femeral and tibial prothesis in Oxford single condylar replacement. Chin J Orthop 38(3):172–178. https://doi.org/10.3760/cma.j.issn.0253-2352.2018.03.007[Chinese]
Ng CTJ, Newman S, Harris S, Clarke S, Cobb J (2017) Patient-specific instrumentation improves alignment of lateral unicompartmental knee replacements by novice surgeons. Int Orthop 41(7):1379–1385
Ollivier M, Parratte S, Lunebourg A, Viehweger E, Argenson JN (2016) The John insall award: no functional benefit after unicompartmental knee arthroplasty performed with patient-specific instrumentation: a randomized trial. Clin Orthop Relat Res 474(1):60–68
Sanz-Ruiz P, Matas-Diez JA, Carbo-Laso E, Perez-Mananes R, Vaquero-Martin J (2019) Patient-Specific instrument can improve functional and radiographic results during learning curve for Oxford unicompartmental knee arthroplasty. J Knee Surg 32(2):180–185
Heyse TJ, Lipman JD, Imhauser CW, Tucker SM, Rajak Y, Westrich GH (2014) Accuracy of individualized custom tibial cutting guides in UKA. HSS J 10(3):260–265
Leenders AM, Schotanus MGM (2018) A high rate of tibial plateau fractures after early experience with patient-specific instrumentation for unicompartmental knee arthroplasties. Knee Surg Sports Traumatol Arthrosc 26(11):3491–3498. https://doi.org/10.1007/s00167-018-4956-9
Flury A, Hasler J, Dimitriou D, Antoniadis A, Finsterwald M, Helmy N (2019) Midterm clinical and radiographic outcomes of 115 consecutive patient-specific unicompartmental knee arthroplasties. Knee 26:889–896
Seeber GH, Kolbow K, Maus U, Kluge A, Lazovic D (2016) Medial unicompartmental knee arthroplasty using patient-specific instrumentation—accuracy of preoperative planning, time saving and cost efficiency. Zeitschrift fur Orthopadie Unfallchirurgie 154(3):287–293
Liow MH, Tsai TY, Dimitriou D, Li G, Kwon YM (2016) Does 3-Dimensional in vivo component rotation affect clinical outcomes in unicompartmental knee arthroplasty? J Arthroplasty 31(10):2167–2172. https://doi.org/10.1016/j.arth.2016.03.003
Iriberri I, Aragon JF (2014) Alignment of the tibial component of the unicompartmental knee arthroplasty, assessed in the axial view by CT scan: does it influence the outcome? Knee 21(6):1269–1274. https://doi.org/10.1016/j.knee.2014.06.008
Acknowledgements
This study was funded by the National Natural Science Foundation of China Program (Nos. 81601936, 81672219), the Science and Technology Department of Sichuan Province (No. 2018HH0141), the Health Department of Sichuan Province (No. 18ZD016) and National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University (No. Z20191008).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, M., Zeng, Y., Wu, Y. et al. Patient-specific instrument for unicompartmental knee arthroplasty does not reduce the outliers in alignment or improve postoperative function: a meta-analysis and systematic review. Arch Orthop Trauma Surg 140, 1097–1107 (2020). https://doi.org/10.1007/s00402-020-03429-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03429-z