Abstract
Introduction
Establishing a systematic multidisciplinary approach in the treatment of prosthetic joint infections (PJI) of the hip and analyzing its effect on clinical decision-making.
Patients and methods
Forty-six patients diagnosed with PJI of the hip were included in the retrospective study. The treatment plan was either established by a single-discipline approach (n = 20) or by a weekly multidisciplinary infections conference (n = 26) consisting of at least an orthopedic surgeon, microbiologist and pathologist. Recorded data included the length of hospital stay, number and type of surgeries, medical complications, recovered organisms as well as the number of applied antibiotics.
Results
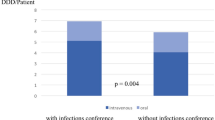
Patients discussed in the multidisciplinary infections conference showed a significantly shorter in-hospital stay (29 vs 62 days; p < 0.05), a significant reduction in surgeries (1.8 vs 5.1; p < 0.05) and a smaller number of antibiotics required (2.8 vs 4.2; p < 0.05). No significant difference could be found comparing inpatient complications between the two groups. Staphylococcus aureus and coagulase-negative staphylococci were the most frequently recovered organisms in both patient groups.
Conclusion
This study demonstrates the successful implementation of a weekly infections conference as an instrument to introduce a multidisciplinary approach to PJI of the hip. Implementation of these conferences significantly improves the treatment plan compared to a single-discipline approach, which we therefore highly recommend for other institutions. Multidiscipline may even affect clinical outcome which needs to be further investigated.
Similar content being viewed by others
References
Wright FC, De Vito C, Langer B et al (2007) Multidisciplinary cancer conferences: a systematic review and development of practice standards. Eur J Cancer Oxf Engl 1990 43:1002–1010. https://doi.org/10.1016/j.ejca.2007.01.025
Pillay B, Wootten AC, Crowe H et al (2016) The impact of multidisciplinary team meetings on patient assessment, management and outcomes in oncology settings: a systematic review of the literature. Cancer Treat Rev 42:56–72. https://doi.org/10.1016/j.ctrv.2015.11.007
Newman EA, Guest AB, Helvie MA et al (2006) Changes in surgical management resulting from case review at a breast cancer multidisciplinary tumor board. Cancer 107:2346–2351. https://doi.org/10.1002/cncr.22266
Foster TJ, Bouchard-Fortier A, Olivotto IA, Quan ML (2016) Effect of multidisciplinary case conferences on physician decision making: breast diagnostic rounds. Cureus 8:e895. https://doi.org/10.7759/cureus.895
El Saghir NS, Keating NL, Carlson RW et al (2014) Tumor boards: optimizing the structure and improving efficiency of multidisciplinary management of patients with cancer worldwide. Am Soc Clin Oncol Educ Book Am Soc Clin Oncol Meet. https://doi.org/10.14694/EdBook_AM.2014.34.e461
Sundi D, Cohen JE, Cole AP et al (2015) Establishment of a new prostate cancer multidisciplinary clinic: format and initial experience. Prostate 75:191–199. https://doi.org/10.1002/pros.22904
Kelly SL, Jackson JE, Hickey BE et al (2013) Multidisciplinary clinic care improves adherence to best practice in head and neck cancer. Am J Otolaryngol 34:57–60. https://doi.org/10.1016/j.amjoto.2012.08.010
Guren E, Figved W, Frihagen F et al (2017) Prosthetic joint infection-a devastating complication of hemiarthroplasty for hip fracture. Acta Orthop 88:383–389. https://doi.org/10.1080/17453674.2017.1301009
Tande AJ, Patel R (2014) Prosthetic joint infection. Clin Microbiol Rev 27:302–345. https://doi.org/10.1128/CMR.00111-13
Ridgeway S, Wilson J, Charlet A et al (2005) Infection of the surgical site after arthroplasty of the hip. J Bone Jt Surg Br 87:844–850. https://doi.org/10.1302/0301-620X.87B6.15121
Merrer J, Girou E, Lortat-Jacob A et al (2007) Surgical site infection after surgery to repair femoral neck fracture: a French multicenter retrospective study. Infect Control Hosp Epidemiol 28:1169–1174. https://doi.org/10.1086/520745
Tande AJ, Gomez-Urena EO, Berbari EF, Osmon DR (2017) Management of prosthetic joint infection. Infect Dis Clin N Am 31:237–252. https://doi.org/10.1016/j.idc.2017.01.009
Strange S, Whitehouse MR, Beswick AD et al (2016) One-stage or two-stage revision surgery for prosthetic hip joint infection—the INFORM trial: a study protocol for a randomised controlled trial. Trials 17:90. https://doi.org/10.1186/s13063-016-1213-8
Kapadia BH, Berg RA, Daley JA et al (2016) Periprosthetic joint infection. Lancet Lond Engl 387:386–394. https://doi.org/10.1016/S0140-6736(14)61798-0
Moore AJ, Whitehouse MR, Gooberman-Hill R et al (2017) A UK national survey of care pathways and support offered to patients receiving revision surgery for prosthetic joint infection in the highest volume NHS orthopaedic centres. Musculoskelet Care 15:379–385. https://doi.org/10.1002/msc.1186
Kini SG, Gabr A, Das R et al (2016) Two-stage revision for periprosthetic hip and knee joint infections. Open Orthop J 10:579–588. https://doi.org/10.2174/1874325001610010579
Parvizi J, Zmistowski B, Berbari EF et al (2011) New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop 469:2992–2994. https://doi.org/10.1007/s11999-011-2102-9
Parvizi J, Gehrke T, International Consensus Group on Periprosthetic Joint Infection (2014) Definition of periprosthetic joint infection. J Arthroplasty 29:1331. https://doi.org/10.1016/j.arth.2014.03.009
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Brauer DG, Strand MS, Sanford DE et al (2017) Utility of a multidisciplinary tumor board in the management of pancreatic and upper gastrointestinal diseases: an observational study. HPB 19:133–139. https://doi.org/10.1016/j.hpb.2016.11.002
Keating NL, Landrum MB, Lamont EB et al (2013) Tumor boards and the quality of cancer care. JNCI J Natl Cancer Inst 105:113–121. https://doi.org/10.1093/jnci/djs502
Lutterbach J, Pagenstecher A, Spreer J et al (2005) The brain tumor board: lessons to be learned from an interdisciplinary conference. Onkologie 28:22–26. https://doi.org/10.1159/000082124
Greer HO, Frederick PJ, Falls NM et al (2010) Impact of a weekly multidisciplinary tumor board conference on the management of women with gynecologic malignancies. Int J Gynecol Cancer Off J Int Gynecol Cancer Soc 20:1321–1325. https://doi.org/10.1111/IGC.0b013e3181f5871e
Lesslie M, Parikh JR (2017) Implementing a multidisciplinary tumor board in the community practice setting. Diagnostics. https://doi.org/10.3390/diagnostics7040055
Zimmerli W, Trampuz A, Ochsner PE (2004) Prosthetic-joint infections. N Engl J Med 351:1645–1654. https://doi.org/10.1056/NEJMra040181
Lamagni T (2014) Epidemiology and burden of prosthetic joint infections. J Antimicrob Chemother 69:i5–i10. https://doi.org/10.1093/jac/dku247
Lee HD, Prashant K, Shon WY (2015) Management of periprosthetic hip joint infection. Hip Pelvis 27:63–71. https://doi.org/10.5371/hp.2015.27.2.63
Pulido L, Ghanem E, Joshi A et al (2008) Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop 466:1710–1715. https://doi.org/10.1007/s11999-008-0209-4
Hernández-Vaquero D, Fernández-Fairen M, Torres A et al (2013) Treatment of periprosthetic infections: an economic analysis. Sci World J 2013:. https://doi.org/10.1155/2013/821650
Kurtz SM, Lau E, Watson H et al (2012) Economic burden of periprosthetic joint infection in the United States. J Arthroplasty 27:61–65.e1. https://doi.org/10.1016/j.arth.2012.02.022
Acknowledgements
This study was conducted at the Department of Trauma-, Hand-, and Reconstructive Surgery, University Medical Center Hamburg-Eppendorf. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. This study was supported by the Damp Foundation (Project 2013-19).
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
D. Ntalos, J. Berger-Groch, H. Rohde, L. G. Grossterlinden, A. Both, A. Luebke, M. J. Hartel and T. O. Klatte declare that they have no conflict of interest.
Human/animal rights statement
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Ntalos, D., Berger-Groch, J., Rohde, H. et al. Implementation of a multidisciplinary infections conference affects the treatment plan in prosthetic joint infections of the hip: a retrospective study. Arch Orthop Trauma Surg 139, 467–473 (2019). https://doi.org/10.1007/s00402-018-3079-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3079-6