Abstract
Introduction
Posterior malleolus and other articular ankle injuries are known to concomitantly occur with tibial shaft fractures, especially spiral fractures of the distal one-third diaphysis. Due to our heightened awareness of this combined injury, our department instituted a new preoperative ankle imaging protocol for all distal one-third spiral tibia shaft fractures. The purpose of this study was to evaluate the effectiveness of an imaging protocol involving radiographs, CT and magnetic resonance imaging (MRI) in a distal one-third spiral tibia fracture cohort.
Materials and methods
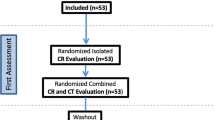
All operatively treated patients with a spiral distal one-third tibial shaft fracture from February 2012 to March 2013 underwent a standardized ankle imaging protocol. Patients had preoperative orthogonal ankle radiographs as well as a CT scan of the tibia that included the ankle. All ankle imaging was scrutinized for evidence of an ankle injury. If no ankle fracture was identified, patients would then undergo an ankle MRI.
Results
Twenty-five patients met the inclusion and exclusion criteria for this study. Concomitant osseous ankle injuries were identified by radiograph and CT in 56 % (14/25) of cases. The remaining 44 % (11/25) of patients had no evidence of a combined injury by radiograph or CT and therefore underwent an MRI. Of the MRI cohort, 64 % (7/11) were found to have an occult ankle fracture. The overall incidence of a combined injury using our protocol was 84 % (21/25). Identification of an occult injury led to a change in management for all of these patients.
Conclusions
Concomitant ipsilateral ankle and distal one-third spiral tibial shaft fractures are more common than previously reported. Utilizing a new imaging protocol, we found that the incidence of this combined injury was 84 %. Recognition of the ankle fracture component in this tibial shaft cohort can be important as it may alter the surgical plan and postoperative management.




Similar content being viewed by others
References
Böstman OM (1988) Displaced malleolar fractures associated with spiral fractures of the tibial shaft. Clin Orthop Relat Res 228:202–207
Lonner JH, Jupiter JB, Healy WL (1993) Ipsilateral tibia and ankle fractures. J Orthop Trauma 7:130–137
Stuermer EK, Stuermer KM (2008) Tibial shaft fracture and ankle joint injury. J Orthop Trauma 22:107–112
Hou Z, Zhang Q, Zhang Y et al (2009) A occult and regular combination injury: the posterior malleolar fracture associated with spiral tibial shaft fracture. J Trauma 66:1385–1390
Boraiah S, Gardner MJ, Helfet DL, Lorich DG (2008) High association of posterior malleolus fractures with spiral distal tibial fractures. Clin Orthop Relat Res 466:1692–1698
Purnell GJ, Glass ER, Altman DT et al (2011) Results of a computed tomography protocol evaluating distal third tibial shaft fractures to assess noncontiguous malleolar fractures. J Trauma 71:163–168
Schottel PC, Berkes MB, Little MTM et al (2014) Predictive radiographic markers for concomitant ipsilateral ankle injuries in tibial shaft fractures. J Orthop Trauma 28:103–107
Berkes MB, Little MTM, Lazaro LE et al (2013) Articular congruity is associated with short-term clinical outcomes of operatively treated SER IV ankle fractures. J Bone Joint Surg Am 95:1769–1775
Kukkonen J, Heikkilä JT, Kyyrönen T et al (2006) Posterior malleolar fracture is often associated with spiral tibial diaphyseal fracture: a retrospective study. J Trauma 60:1058–1060
Lauge-Hansen N (1954) Fractures of the ankle. III Genetic roentgenologic diagnosis of fractures of the ankle. Am J Roentgenol Radium Ther Nucl Med 71:456–471
Lauge-Hansen N (1950) Fractures of the ankle. II Combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg 60:957–985
Georgiadis GM, Ebraheim NA, Hoeflinger MJ (1996) Displacement of the posterior malleolus during intramedullary tibial nailing. J Trauma 41:1056–1058
Konrath G, Moed BR, Watson JT et al (1997) Intramedullary nailing of unstable diaphyseal fractures of the tibia with distal intraarticular involvement. J Orthop Trauma 11:200–205
Takao M, Ochi M, Oae K et al (2003) Diagnosis of a tear of the tibiofibular syndesmosis. The role of arthroscopy of the ankle. J Bone Joint Surg Br 85:324–329
Vogl TJ, Hochmuth K, Diebold T et al (1997) Magnetic resonance imaging in the diagnosis of acute injured distal tibiofibular syndesmosis. Invest Radiol 32:401–409
Conflict of interest
No conflicts of interest declared for all authors regarding this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Warner, S.J., Schottel, P.C., Garner, M.R. et al. Ankle injuries in distal tibial spiral shaft fractures: results from an institutional change in imaging protocol. Arch Orthop Trauma Surg 134, 1661–1666 (2014). https://doi.org/10.1007/s00402-014-2095-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-2095-4