Abstracts
Introduction
Adjacent segment degeneration (ASD) is a complication of lumbar spinal fusion. There are some reports on the cause of this degeneration but none concerning its prevention. We performed sublaminar wiring stabilization to prevent ASD after posterolateral lumbar spinal fusion with instrumentation. The purpose of this study was to prospectively evaluate the efficacy of this procedure.
Patients and methods
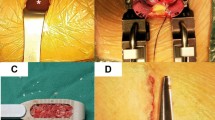
Between 2003 and 2004, 54 consecutive patients with lumbar spinal canal stenosis and multilevel instability of the lumbar spine underwent posterior decompression and posterolateral fusion with instrumentation. The mean age at the time of surgery was 66.7 ± 1.3 years, and the mean follow-up period was 40.0 ± 1.1 months, with a minimum of 29 months. Twenty-seven of the patients underwent conventional sublaminar wiring stabilization at the cephalad segment adjacent to the site of fusion to prevent ASD (group A), and the other 27 patients did not (group B). Some items were assessed, including clinical outcome using Japanese Orthopaedic Association (JOA) score, sagittal global lumbar alignment, and segmental motion in flexion–extension radiographs of the cephalad vertebral body adjacent to the site of fusion.
Results
There were no significant differences in JOA scores between two groups, but 2 patients in group B underwent subsequent surgery due to ASD. Sagittal lumbar alignment did not change in group A but was significantly decreased in group B. With respect to segmental motion in flexion–extension radiographs, group A showed a significant decrease from 6.9° before surgery to 3.4° after surgery, on the other hand group B showed a significant increase from 5.6° before surgery to 8.4° after surgery.
Conclusions
In this study, it was suggested that sublaminar wiring stabilization significantly reduces the range of motion of the adjacent segment and preserves sagittal lumbar alignment, which lead to prevention of ASD. The clinical outcome of the subsequent surgeries is relatively poor, so it is important to prevent ASD by any prevention such as sublaminar wiring stabilization.

Similar content being viewed by others
References
Aota Y, Kumano K, Hirabayashi S (1995) Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord 8:464–473
Brechbuhler D, Markwalder TM, Braun M (1998) Surgical results after soft system stabilization of the lumbar spine in degenerative disc disease—long-term results. Acta Neurochir Wien 140:521–525
Chen CS, Feng CK, Cheng CK et al (2005) Biomechanical analysis of the disc adjacent to posterolateral fusion with laminectomy in lumbar spine. J Spinal Disord Tech 18:58–65
Chosa E, Goto K, Totoribe K et al (2004) Analysis of the effect of lumbar spine fusion on the superior adjacent intervertebral disk in the presence of disk degeneration, using the three-dimensional finite element method. J Spinal Disord Tech 17:134–139
Chou WY, Hsu CJ, Chang WN et al (2002) Adjacent segment degeneration after lumbar spinal posterolateral fusion with instrumentation in elderly patients. Arch Orthop Trauma Surg 122:39–43
Eck JC, Humphreys SC, Hodges SD (1999) Adjacent-segment degeneration after lumbar fusion: a review of clinical, biomechanical, and radiologic studies. Am J Orthop 28:336–340
Etebar S, Cahill DW (1999) Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg 90:163–169
Ghiselli G, Wang JC, Bhatia NN et al (2004) Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am 86:1497–1503
Goto K, Tajima N, Chosa E et al (2003) Effects of lumbar spinal fusion on the other lumbar intervertebral levels (three-dimensional finite element analysis). J Orthop Sci 8:577–584
Hadlow SV, Fagan AB, Hillier TM et al (1998) The Graf ligamentoplasty procedure: comparison with posterolateral fusion in the management of low back pain. Spine 23:1172–1179
Hashimoto T, Oha F, Shigenobu K et al (2001) Mid-term clinical results of Graf stabilization for lumbar degenerative pathologies: a minimum 2-year follow-up. Spine J 1:283–289
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4:190S–194S
Hirabayashi K, Watanabe K, Wakano K et al (1983) Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine 8:693–699
Javedan SP, Dickman CA (1999) Cause of adjacent-segment disease after spinal fusion. Lancet 354:530–531
Kanayama M, Hashimoto T, Shigenobu K et al (2001) Adjacent-segment morbidity after Graf ligamentoplasty compared with posterolateral lumbar fusion. J Neurosurg 95:5–10
Kumar MN, Baklanov A, Chopin D (2001) Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J 10:314–319
Lai PL, Chen LH, Niu CC et al (2004) Effect of postoperative lumbar sagittal alignment on the development of adjacent instability. J Spinal Disord Tech 17:353–357
Lee CK (1988) Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine 13:375–377
Nagata H, Schendel MJ, Transfeldt EE et al (1993) The effects of immobilization of long segments of the spine on the adjacent and distal facet force and lumbosacral motion. Spine 18:2471–2479
Niosi CA, Oxland TR (2004) Degenerative mechanics of the lumbar spine. Spine J 4:202S–208S
Ogawa H, Nishimoto H, Hosoe H et al (2007) Clinical outcome after segmental wire fixation and bone grafting for repair of the defects in multiple level lumbar spondylolysis. J Spinal Disord Tech 20:521–525
Park P, Garton HJ, Gala VC et al (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine 29:1938–1944
Phillips FM, Reuben J, Wetzel FT (2002) Intervertebral disc degeneration adjacent to a lumbar fusion. An experimental rabbit model. J Bone Joint Surg Br 84:289–294
Strauss PJ, Novotny JE, Wilder DG et al (1994) Multidirectional stability of the Graf system. Spine 19:965–972
Whitecloud TS 3rd, Davis JM, Olive PM (1994) Operative treatment of the degenerated segment adjacent to a lumbar fusion. Spine 19:531–536
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ogawa, H., Hori, H., Oshita, H. et al. Sublaminar wiring stabilization to prevent adjacent segment degeneration after lumbar spinal fusion. Arch Orthop Trauma Surg 129, 873–878 (2009). https://doi.org/10.1007/s00402-008-0725-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-008-0725-4