Abstract
Background and objectives
Catheter ablation of atrial fibrillation (AF) has become a well-established and widely used therapy, with pulmonary vein isolation (PVI) being the key modality of ablation. However, arrhythmia recurrences after PVI are common, with a relevant number of patients undergoing repeat ablation. Arrhythmia recurrence after PVI may vary regarding time point and mode of recurrence. While early arrhythmia recurrences of AF after PVI are mostly found to be the product of electrical reconnection of the pulmonary veins, the exact mechanisms of very late arrhythmia recurrence, occurring later than 12 months after successful PVI, remain unclear. This review provides an overview on the current evidence on time point and mechanisms of arrhythmia recurrence after PVI focussing on late arrhythmia recurrence.
Recent findings
The incidence of late arrhythmia recurrence after PVI can lie at a rate of up to 30% according to long-term follow-up studies. Mechanisms of recurrence include electrical reconnection of previously isolated pulmonary veins and development of atrial fibrosis. The use of cryoballoon ablation is likely to be more effective in reducing late arrhythmia recurrences compared to radiofrequency ablation. Novel scores such as the MB-LATER score or the APPLE score may become useful tools in predicting arrhythmia recurrence after PVI.
Results and conclusion
Late arrhythmia recurrence after PVI is common and leads to a relevant impairment of long-term success. Relevant data are currently limited and exact mechanisms of arrhythmia recurrence remain unclear. Further studies are needed to elucidate pathogenetic mechanisms of late arrhythmia recurrence after PVI in order to improve treatment strategies.
Zusammenfassung
Hintergrund und Ziel der Arbeit
Die Katheterablation von Vorhofflimmern (VHF) hat sich zu einer etablierten und weit verbreiteten Therapie entwickelt, wobei die Pulmonalvenenisolation (PVI) die wichtigste Ablationsmethode darstellt. Dennoch sind Arrhythmierezidive häufig und eine relevante Anzahl von Patienten benötigt wiederholte Ablationen. Rezidive nach PVI können hinsichtlich des Rezidivzeitpunkts und unterliegenden Mechanismus variieren. Während frühe VHF-Rezidive nach PVI meist auf die elektrische Rekonnektion der Pulmonalvenen zurückzuführen sind, bleiben die genauen Mechanismen sehr später Arrhythmierezidive, die mehr als 12 Monate nach erfolgreicher PVI auftreten, unklar. Die vorliegende Übersichtsarbeit fasst die aktuelle Studienlage zu Zeitpunkt und Mechanismen von Arrhythmierezidiven nach PVI zusammen. Der Schwerpunkt liegt dabei auf Spätrezidiven.
Ergebnisse
Die Inzidenz von späten Arrhythmierezidiven nach PVI kann laut Langzeitstudien bis zu 30 % betragen. Zu den unterliegenden Mechanismen gehören die elektrische Rekonnektion zuvor isolierter Pulmonalvenen und die Entwicklung atrialer Fibrosen. Die Kryoballonablation verringert späte Arrhythmierezidive potenziell wirksamer als die Radiofrequenzablation. Kürzlich entwickelte Scores wie der MB-LATER-Score oder der APPLE-Score könnten sich als nützliche Instrumente für die Vorhersage eines Arrhythmierezidivs nach PVI erweisen.
Schlussfolgerung
Das späte Wiederauftreten von Arrhythmien nach PVI ist ein häufiges Phänomen, das den langfristigen Therapieerfolg erheblich beeinträchtigt. Derzeit liegen nur wenige Daten zu diesem Thema vor und die genauen Mechanismen später Arrhythmierezidive sind unklar. Weitere Studien sind erforderlich, um die unterliegenden pathogenetischen Mechanismen aufzuklären und somit Behandlungsstrategien verbessern zu können.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
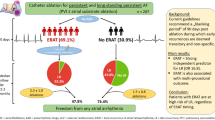
Catheter ablation has become an accepted first line therapy for paroxysmal atrial fibrillation (PAF), with pulmonary vein isolation (PVI) being the key element of ablation strategies [1, 2]. Catheter ablation of AF has been proven to be superior to antiarrhythmic drug (AAD) therapy regarding efficacy and improvement of survival in patients with heart failure [3, 4].
However, early recurrence of AF (ERAF) within the first 3 months after PVI using radiofrequency (RF) energy is a clinically relevant problem with up to 35% of patients needing repeat ablation procedures [5, 6]. Early arrhythmia recurrence within the first 3 months after PVI is mostly associated with early inflammation, incomplete scar formation and pulmonary vein reconnection [5, 7, 8].
In contrast, data on arrhythmia recurrence occurring at later than 1 year, or even after multiple years after PVI, are limited and the exact mechanisms behind late arrhythmia recurrence after PVI have not been clearly identified to date [9, 10].
The present article provides the current scientific view on the mechanisms and incidence of arrhythmia recurrence after PVI focussing on late arrhythmia recurrence.
Efficacy of AF ablation
PVI has become a routine treatment procedure in recent decades especially for patients with symptomatic PAF [4, 5].
A systematic meta-analysis from 2009 investigating 31 different studies found a single procedure success rate of 57% and a multiple procedure success rate of 71% in patients receiving radiofrequency ablation (RFA) without any anti-arrhythmic drug therapy [11].
A 5-year follow-up published in 2010, which investigated the outcome of PVI using RFA in patients with PAF, found a 46.6% success rate in patients undergoing only one ablation procedure. Success was defined as a stable sinus rhythm for 5 years after the procedure, with success rates increasing to 73.9% when additional procedures were performed. A total of 72.1% of recurrences took place within the first 12 months after the initial ablation procedure [12].
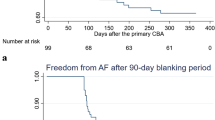
As most arrhythmia recurrences take place within the first 3 months after the initial procedure, this time period is seen as a so-called “blanking period”, in which ablation is not recommended, since up to 50% of patients can become arrhythmia-free in the long run [5].
Ablation therapy, however, is less successful in patients suffering from longstanding persistent AF, with a 20.3% success rate after a single procedure and a 45% success rate after multiple RFA procedures according to a 5-year follow up conducted in 2012 [13].
The STAR AF II Trial published in 2015 investigated different ablation strategies when treating longstanding persistent AF, addressing the higher recurrence rates when treating persistent AF compared to PAF. However, no significant difference regarding arrhythmia-free survival was found between PVI only compared to linear lesions ablation only or ablation of complex fractionated electrograms [14].
In comparison to RF energy the use of cryoballoon technology (CB) as an ablation method for PAF has shown significantly higher successful procedural outcomes with 60.3–72.8% of patients being free from arrhythmia after a single procedure has been performed [15,16,17]. Another study, however, identified that the rate of early AF recurrences still lies at about 50% after a single procedure when using CB technology [18].
Early arrhythmia recurrence
Repeat ablation procedures are mostly performed after a blanking period since early arrhythmia recurrence after PVI is often associated with inflammation and inhomogeneous scar tissue formation after ablation [5]. A blanking period of 3 months is common clinical practice today [19]. AF recurrence within that timeframe is referred to as ERAF and, despite being common, is considered a risk factor for late AF recurrences with long-term clinical impact [1, 5, 10].
Especially patients suffering from AF recurrences in the third months of the blanking period have an up to 90% chance of being symptomatic again after 1 year [19].
An arrhythmia-free period of 1 month after the ablation, on the other hand, does not necessarily guarantee long-term arrhythmia-free survival [20].
The effect of prevention of early recurrences on long-term arrhythmia-free survival has not been evaluated as yet [6, 21].
Long-term success of catheter ablation
It is well known that untreated PAF often progresses to persistent AF and ultimately results in acceptance of permanent AF. Therefore, early treatment of PAF is critical to improve long-term outcome [22, 23].
In the majority of patients suffering from PAF catheter ablation results in stable sinus rhythm as shown in long-term follow-up studies [5, 20]. However, most patients need multiple ablation procedures to restore durable sinus rhythm [24, 25]. According to one meta-analysis study, patients suffering from PAF undergoing multiple ablation procedures using RF energy have a long-term success rate of about 80%, whilst success rates for patients undergoing only one ablation procedure is around 53% [24]. Recent data suggest there are several reasons for this significant difference, with pulmonary vein reconnection probably being the most prominent one [26]. Long-term success rates are significantly lower in patients, with persistent AF resulting in only a 20–45% rate of 5‑year arrhythmia-free survival after multiple RFA [13, 27]. The ideal ablation strategy for patients with persistent AF has not yet been identified [21, 27].
Incidence of very late arrhythmia recurrence
Very late arrhythmia recurrences after PVI are commonly defined as recurrent AF occurring 12 months or later after the last procedure [5]. Most studies agree that pulmonary vein reconnection and the development of non PV triggers are the main mechanism behind these recurrences [26, 28].
A 2008 study from New York providing 28-month follow-up post RF PVI in patients suffering from PAF discovered that late recurrence of AF occurs in 8.7% of patients. The study also concluded that there was a significantly higher incidence of hypertension and dyslipidaemia in these patients [26].
Weerasooriya et al. described an arrhythmia-free survival rate of 63% in PAF patients 5 years after the last RFA, and noted a gradual increase in recurrence rates over time [29]. Another study showed that there was an increase from 27 to 39% in recurrence rates (1 and 2.5 years after ablation) in patients suffering from PAF. The recurrence rates were even higher (from 37 to 57%) in patients initially suffering from persistent AF [30].
This thesis is also underlined in the 2017 expert consensus statement on AF ablation, which states that an increase in follow-up duration also increases the likelihood of arrhythmia recurrences [5].
A study from 2016 investigated late recurrences after CB PVI and described a late arrhythmia recurrence rate of 69% in patients who already suffered from ERAF. On the other hand, there was an only 9.3% late recurrence rate in patients not having previously suffered from ERAF. This underlines the fact that the likelihood of late arrhythmia recurrence is drastically increased when ERAF had occurred [31]. A summary of all reviewed publications can be found in Table 1.
Mechanisms of early and late arrhythmia recurrence after ablation
One of the identified main causes of atrial fibrillation recurrences after PVI is electrical reconnection within the pulmonary veins [24, 32, 33]. Early recurrence within the first month of the procedure lies at around 27 and 35% [6, 34]. A recent study from Pennsylvania has found reconnection of previously isolated pulmonary vein segments in 97% of patients and identified these electrical reconnections as a trigger of recurrent atrial fibrillation [35]. Other studies additionally described that the majority of triggers of recurrent AF after PVI originated from electrically reconnected areas within the pulmonary veins rather than from newly formed trigger points [7]. The rate of pulmonary vein reconduction is 80% within the first 4 month after RFA [33]. Patients suffering from ERAF are considered to be more likely to suffer from AF in the long run [19].
Although pulmonary vein reconnection is the major issue concerning early recurrences of AF after PVI, experts believe that individual risk factors may be of importance [24, 36]. A recent study from Hamburg identified body mass index (BMI) as a main risk factor for developing AF, and a study from 2013 investigating the predicting factors of late AF recurrence identified obesity, metabolic syndrome, procedural failure and ERAF as clear independent risk factors for late recurrence [37, 38].
One study identified that patients with risk factors such as high BMI who underwent risk factor management (RFM) after their RFA had better long-term outcomes regarding AF recurrences compared to patients not receiving RFA [39].
Especially a high amount of pericardial fat can result in a less successful long-term RFA outcome in all subtypes of AF and can also lead to a higher symptom burden for patients [40, 41]. The correlation between AF recurrences and the amount of pericardial fat may be stronger than mere BMI [40].
A study from 2015 showed that the CHADS2 or CHA2DS2-VASc score, heart failure and stroke were effective in predicting the procedural outcome after RFA over 5 years for all AF subtypes [42].
Patients suffering from AF recurrence after PVI are also likely to have hyperlipidaemia, hypertension or obstructive sleep apnoea (OSA) [26, 39, 43]. OSA was identified to be the most accurate predictor of AF recurrence with only 41% arrhythmia-free patients 4–7 months after PVI compared to 63% arrhythmia-free patients without OSA [43, 44]. Atrial remodelling in patients with OSA may be causative for higher recurrence rates [45]. Therefore, treating OSA in AF patients with continuous positive airway pressure (CPAP) ventilation reduces their risk of arrhythmia recurrence after PVI [46, 47].
Furthermore, AF has been associated with genetic predispositions [48, 49]. Several Studies have identified a potential genetic predisposition regarding recurrences of AF after PVI [50, 51]. For example, patients with polymorphisms on chromosome 4q25 were at higher risk for generally developing AF as well as for developing early and late arrhythmia recurrence after PVI [52, 53].
Influence of the ablation approach on AF recurrences
In addition to predispositions and individual risk factors the ablation approach can also influence short- and long-term outcome [5]. For example, experts believed that using the technique of an atrial line in the repeat RF PVI might decrease the likelihood of developing PAF recurrences. A study from Munich, Germany, however, has proved this theory wrong, showing instead that there is no significant difference regarding AF recurrences when using an atrial line + PVI versus using a standard RF PVI [54].
As PV reconnection is a major cause of ERAF, detecting reconnected trigger points as early as possible can be very effective in improving procedural success [24]. This rate of early reconnection of the PV can be reduced by incorporating a waiting period of 1 h after the initial procedure. Implementing this waiting period into clinical practice could help detect early reconnections, thus reducing the rate of AF recurrences [55, 56].
The increasingly used CB for PVI might also influence the rate of early and late AF recurrences [5]. The fire and ice trial has already identified CB-based PVI as equally effective compared to RF-based PVI in patients with PAF [16]. According to a 2014 study up to 50% of patients with PAF receiving CB ablation suffered from ERAF. In the study early reablation was strongly associated with a lower incidence of late AF recurrences, with only 3.3.% of patients developing a late recurrence after a repeat ablation and 55.6% developing recurrences without receiving reablation [18].
The more recently developed cryoballoon 2 has shown even better procedural outcomes, with 83.6% of PAF patients being free from AF recurrences after a single PVI was performed [57, 58]. Additionally, the rate of PV reconnection appears to be significantly lower when using CB compared to RFA [59].
Prediction of arrhythmia recurrences
For better prediction of arrhythmia recurrence, predictive scores have become an important tool. A new score from 2017 is the APPLE Score. It includes several factors such as age > 65 years, persistent AF, impaired estimated glomerular filtration rate (< 60 ml/min/1.73 m2), left atrium diameter ≥ 43 mm and an ejection fraction < 50%, with each factor counting for one point. A study from Leipzig, Germany, has shown that this scoring system is a superior predictor of AF recurrences after repeat ablation compared to scores such as CHADS2 and CHA2DS2-VASc [60]. Another promising new score is the MB-LATER Score (male, bundle branch block, left atrium ≥ 47 mm, type of AF [paroxysmal, persistent or long-standing persistent AF], and ERAF). One study that compared different scores focused entirely on predicting AF recurrences after PVI and used the area under the curve (AUC) as an indicator for the predictive value of the scores. The study showed that the MB-LATER Score provided a more accurate prediction of very late AF recurrence (AUC 0.782) than other scoring systems (including the APPLE score [AUC 0.716]) [61].
A more recent study from Leipzig, however, disagreed with these findings, stating that while other scoring systems are useful, early recurrence of AF remains the clearest and most precise indicator of late arrhythmia recurrence. The authors concluded that an accurate AF recurrence prediction score that can be fully implemented into clinical practice has not yet been found [62].
Conclusion
PVI has become an accepted treatment for PAF. However, recurrences especially within the first 3 months post ablation may occur, with most patients needing more than one ablation to maintain stable sinus rhythm. The mechanism of electrical reconnection of the pulmonary veins is the main reason for early and late AF recurrences. However, individual risk factors like BMI and obesity definitely may affect likelihood of arrhythmia recurrence also after PVI. CB-based PVI might be beneficial in order to reduce early and late arrhythmia recurrence rates after PVI. However, long-term follow-up studies focusing on late AF recurrences after CB ablation are limited.
Several scoring systems, such as the MB LATER Score, have been developed to predict AF recurrences but need further evaluation in larger studies before routine clinical use. All in all, studies investigating late arrhythmia recurrences after PVI are sparse and more studies need to be conducted in future for a better understanding and effective management.
References
Cosedis Nielsen J, Johannessen A, Raatikainen P et al (2012) Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl J Med 367:1587–1595
Kuck K‑H, Hoffmann BA, Ernst S et al (2016) Impact of complete versus incomplete circumferential lines around the pulmonary veins during catheter ablation of paroxysmal atrial fibrillation: results from the gap-atrial fibrillation—German atrial fibrillation competence network 1 trial. Circ Arrhythm Electrophysiol 9:e3337
Marrouche NF, Brachmann J, Andresen D et al (2018) Catheter ablation for atrial fibrillation with heart failure. N Engl J Med 378:417–427
Biase LD, Mohanty P, Mohanty S et al (2016) Ablation versus amiodarone for treatment of persistent atrial fibrillation in patients with congestive heart failure and an implanted device. Circulation 133:1637–1644
Calkins H, Hindricks G, Cappato R et al (2017) 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace 20:e1–e160
Oral H, Knight BP, Özaydın M et al (2002) Clinical significance of early recurrences of atrial fibrillation after pulmonary vein isolation. J Am Coll Cardiol 40:100–104
Gerstenfeld EP, Callans DJ, Dixit S, Zado E, Marchlinski FE (2003) Incidence and location of focal atrial fibrillation triggers in patients undergoing repeat pulmonary vein isolation. J Cardiovasc Electrophysiol 14:685–690
Issac TT, Dokainish H, Lakkis NM (2007) Role of inflammation in initiation and perpetuation of atrial fibrillation: a systematic review of the published data. J Am Coll Cardiol 50:2021–2028
Fisher JD, Spinelli MA, Mookherjee D, Krumerman AK, Palma EC (2006) Atrial fibrillation ablation: reaching the mainstream. Pacing Clin Electro 29:523–537
Narayan SM, Baykaner T, Clopton P et al (2014) Ablation of rotor and focal sources reduces late recurrence of atrial fibrillation compared with trigger ablation alone: extended follow-up of the confirm trial (conventional ablation for atrial fibrillation with or without focal impulse and rotor modulation). J Am Coll Cardiol 63:1761–1768
Calkins H, Reynolds MR, Spector P et al (2009) Treatment of atrial fibrillation with antiarrhythmic drugs or radiofrequency ablation. Circ Arrhythm Electrophysiol 2:349–361
Ouyang F, Tilz R, Chun J et al (2010) Long-term results of catheter ablation in paroxysmal atrial fibrillation: lessons from a 5-year follow-up. Circulation 122:2368–2377
Tilz RR, Rillig A, Thum A‑M et al (2012) Catheter ablation of long-standing persistent atrial fibrillation: 5‑year outcomes of the Hamburg sequential ablation strategy. J Am Coll Cardiol 60:1921–1929
Verma A, C‑y J, Betts TR et al (2015) Approaches to catheter ablation for persistent atrial fibrillation. N Engl J Med 372:1812–1822
Andrade JG, Khairy P, Guerra PG et al (2011) Efficacy and safety of cryoballoon ablation for atrial fibrillation: a systematic review of published studies. Heart Rhythm 8:1444–1451
Kuck K‑H, Brugada J, Fürnkranz A et al (2016) Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med 374:2235–2245
Klein G, Oswald H, Gardiwal A et al (2008) Efficacy of pulmonary vein isolation by cryoballoon ablation in patients with paroxysmal atrial fibrillation. Heart Rhythm 5:802–806
Andrade JG, Khairy P, Macle L et al (2014) Incidence and significance of early recurrences of atrial fibrillation after cryoballoon ablation: insights from the multicenter sustained treatment of paroxysmal atrial fibrillation (stop Af) trial. Circ Arrhythm Electrophysiol 7:69–75
Willems S, Khairy P, Andrade JG et al (2016) Redefining the blanking period after catheter ablation for paroxysmal atrial fibrillation: insights from the ADVICE (adenosine following pulmonary vein isolation to target dormant conduction elimination) trial. Circ Arrhythm Electrophysiol 9:e3909
Gaita F, Caponi D, Scaglione M et al (2008) Long-term clinical results of 2 different ablation strategies in patients with paroxysmal and persistent atrial fibrillation. Circ Arrhythm Electrophysiol 1:269–275
Willems S, Klemm H, Rostock T et al (2006) Substrate modification combined with pulmonary vein isolation improves outcome of catheter ablation in patients with persistent atrial fibrillation: a prospective randomized comparison. Eur Heart J 27:2871–2878
de Vos CB, Pisters R, Nieuwlaat R et al (2010) Progression from paroxysmal to persistent atrial fibrillation. Clinical correlates and prognosis. J Am Coll Cardiol 55:725–731
Kerr CR, Humphries KH, Talajic M et al (2005) Progression to chronic atrial fibrillation after the initial diagnosis of paroxysmal atrial fibrillation: results from the Canadian registry of atrial fibrillation. Am Heart J 149:489–496
Ganesan AN, Shipp NJ, Brooks AG et al (2013) Long-term outcomes of catheter ablation of atrial fibrillation: a systematic review and meta-analysis. J Am Heart Assoc 2:e4549
Pratola C, Baldo E, Notarstefano P, Toselli T, Ferrari R (2008) Radiofrequency atrial fibrillation ablation based on pathophysiology: a diversified protocol with long-term follow-up. J Cardiovasc Med 9:68–75
Shah AN, Mittal S, Sichrovsky TC et al (2008) Long-term outcome following successful pulmonary vein isolation: pattern and prediction of very late recurrence. J Cardiovasc Electrophysiol 19:661–667
Brooks AG, Stiles MK, Laborderie J et al (2010) Outcomes of long-standing persistent atrial fibrillation ablation: a systematic review. Heart Rhythm 7:835–846
Mainigi SK, Sauer WH, Cooper JM et al (2007) Incidence and predictors of very late recurrence of atrial fibrillation after ablation. J Cardiovasc Electrophysiol 18:69–74
Weerasooriya R, Khairy P, Litalien J et al (2011) Catheter ablation for atrial fibrillation. Are results maintained at 5 years of follow-up? J Am Coll Cardiol 57:160–166
Wokhlu A, Hodge D, Monahan KH et al (2010) Long-term outcome of atrial fibrillation ablation: impact and predictors of very late recurrence. J Cardiovasc Electrophysiol 21:1071–1078
Mugnai G, de Asmundis C, Hünük B et al (2016) Second-generation cryoballoon ablation for paroxysmal atrial fibrillation: predictive role of atrial arrhythmias occurring in the blanking period on the incidence of late recurrences. Heart Rhythm 13:845–851
Maurer T, Kuck K‑H (2017) The quest for durable lesions in catheter ablation of atrial fibrillation—technological advances in radiofrequency catheters and balloon devices. Expert Rev Med Devices 14:621–631
Cappato R, Negroni S, Pecora D et al (2003) Prospective assessment of late conduction recurrence across radiofrequency lesions producing electrical disconnection at the pulmonary vein ostium in patients with atrial fibrillation. Circulation 108:1599–1604
Deftereos S, Giannopoulos G, Kossyvakis C et al (2012) Colchicine for prevention of early atrial fibrillation recurrence after pulmonary vein isolation: a randomized controlled study. J Am Coll Cardiol 60:1790–1796
Callans DJ, Gerstenfeld EP, Dixit S et al (2004) Efficacy of repeat pulmonary vein isolation procedures in patients with recurrent atrial fibrillation. J Cardiovasc Electrophysiol 15:1050–1055
Balk EM, Garlitski AC, Alsheikh-Ali AA, Terasawa T, Chung M, Ip S (2010) Predictors of atrial fibrillation recurrence after radiofrequency catheter ablation: a systematic review. J Cardiovasc Electrophysiol 21:1208–1216
Cai L, Yin Y, Ling Z et al (2013) Predictors of late recurrence of atrial fibrillation after catheter ablation. Int J Cardiol 164:82–87
Magnussen C, Niiranen TJ, Ojeda FM et al (2017) Sex differences and similarities in atrial fibrillation epidemiology, risk factors, and mortality in community cohorts. Circulation 136:1588–1597
Pathak RK, Middeldorp ME, Lau DH et al (2014) Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation. The ARREST-AF cohort study. J Am Coll Cardiol 64:2222–2231
Wong CX, Abed HS, Molaee P et al (2011) Pericardial fat is associated with atrial fibrillation severity and ablation outcome. J Am Coll Cardiol 57:1745–1751
Thanassoulis G, Massaro JM, O’donnell CJ et al (2010) Pericardial fat is associated with prevalent atrial fibrillation: the Framingham heart study. Circ Arrhythm Electrophysiol 3:345–350
Jacobs V, May HT, Bair TL et al (2015) The impact of risk score (CHADS2 versus CHA2DS2-VASc) on long-term outcomes after atrial fibrillation ablation. Heart Rhythm 12:681–686
Jongnarangsin K, Chugh A, Good E et al (2008) Body mass index, obstructive sleep apnea, and outcomes of catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol 19:668–672
Ng CY, Liu T, Shehata M, Stevens S, Chugh SS, Wang X (2011) Meta-analysis of obstructive sleep apnea as predictor of atrial fibrillation recurrence after catheter ablation. Am J Cardiol 108:47–51
Dimitri H, Ng M, Brooks AG et al (2012) Atrial remodeling in obstructive sleep apnea: implications for atrial fibrillation. Heart Rhythm 9:321–327
Kanagala R, Murali NS, Friedman PA et al (2003) Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation 107:2589–2594
Fein AS, Shvilkin A, Shah D et al (2013) Treatment of obstructive sleep apnea reduces the risk of atrial fibrillation recurrence after catheter ablation. J Am Coll Cardiol 62:300–305
Feghaly J, Zakka P, London B, MacRae CA, Refaat MM (2018) Genetics of atrial fibrillation. J Am Heart Assoc 7:e9884
Brugada R, Tapscott T, Czernuszewicz GZ et al (1997) Identification of a genetic locus for familial atrial fibrillation. N Engl J Med 336:905–911
Gudbjartsson DF, Arnar DO, Helgadottir A et al (2007) Variants conferring risk of atrial fibrillation on chromosome 4q25. Nature 448:353
Wu H, Xu J, Chen S et al (2017) Association of SCN10A polymorphisms with the recurrence of atrial fibrillation after catheter ablation in a Chinese Han population. Sci Rep 7:44003
Husser D, Adams V, Piorkowski C, Hindricks G, Bollmann A (2010) Chromosome 4q25 variants and atrial fibrillation recurrence after catheter ablation. J Am Coll Cardiol 55:747–753
Kääb S, Beckmann BM, Steinbeck G et al (2009) Large scale replication and meta-analysis of variants on chromosome 4q25 associated with atrial fibrillation. Eur Heart J 30:813–819
Fichtner S, Sparn K, Reents T et al (2015) Recurrence of paroxysmal atrial fibrillation after pulmonary vein isolation: is repeat pulmonary vein isolation enough? A prospective, randomized trial. Europace 17:1371–1375
Cheema A, Dong J, Dalal D et al (2007) Incidence and time course of early recovery of pulmonary vein conduction after catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol 18:387–391
Solimene F, Schillaci V, Shopova G et al (2019) Safety and efficacy of atrial fibrillation ablation guided by ablation index module. J Interv Card Electrophysiol 54:9–15
Kuck K‑H, Metzner A, Ouyang F et al (2016) Cryoballoon or radiofrequency ablation for symptomatic paroxysmal atrial fibrillation: reintervention, rehospitalization, and quality-of-life outcomes in the fire and ice trial. Eur Heart J 37:2858–2865
Fürnkranz A, Bordignon S, Dugo D et al (2014) Improved 1‑year clinical success rate of pulmonary vein isolation with the second-generation cryoballoon in patients with paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol 25:840–844
Kuck K‑H, Albenque J‑P, Chun KRJ et al (2019) Repeat ablation for atrial fibrillation recurrence post cryoballoon or radiofrequency ablation in the fire and ice trial. Circ Arrhythm Electrophysiol 12:e7247
Kornej J, Hindricks G, Shoemaker MB et al (2015) The Apple score: a novel and simple score for the prediction of rhythm outcomes after catheter ablation of atrial fibrillation. Clin Res Cardiol 104:871–876
Mujović N, Marinković M, Marković N, Shantsila A, Lip GY, Potpara TS (2017) Prediction of very late arrhythmia recurrence after radiofrequency catheter ablation of atrial fibrillation: the MB-LATER clinical score. Sci Rep 7:40828
Kornej J, Schumacher K, Dinov B et al (2018) Prediction of electro-anatomical substrate and arrhythmia recurrences using Apple, DR-Flash and MB-Later scores in patients with atrial fibrillation undergoing catheter ablation. Sci Rep 8:12686
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
N. Erhard, A. Metzner and T. Fink declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Additional information

Scan QR code & read article online
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Erhard, N., Metzner, A. & Fink, T. Late arrhythmia recurrence after atrial fibrillation ablation: incidence, mechanisms and clinical implications. Herzschr Elektrophys 33, 71–76 (2022). https://doi.org/10.1007/s00399-021-00836-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00399-021-00836-6
Keywords
- Atrial fibrillation
- Catheter ablation
- Pulmonary vein isolation
- Late recurrences
- Atrial fibrosis
- Arrhythmia recurrence