Abstract
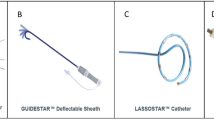
Electrical isolation of pulmonary veins is the cornerstone of catheter ablation for patients with symptomatic atrial fibrillation. However, uncertainty surrounds the choice of energy source in pulmonary vein isolation (PVI). Various alternative techniques such as the Pulmonary Vein Ablation Catheter (PVAC®, Medtronic Inc., Minneapolis, MN, USA) have been developed to facilitate PVI. This over-the-wire multielectrode catheter is delivering duty-cycled bipolar and unipolar radiofrequency (RF) energy at relatively low power.
PVI with this “one-shot” PVACatheter can shorten the procedure duration and lower fluoroscopy time compared to irrigated RF. It enables mapping and ablation with the same array, but fails to show signals during RF energy delivery. The effectiveness of PVAC is comparable to other technologies in randomized studies. The overall complication rate of PVAC PVI is comparable to irrigated RF and possibly slightly higher for cryoballoon PVI. Special attention has to be paid to an effective anticoagulation throughout the ablation procedure, avoidance of embolic events and pulmonary venous stenosis.
The novel catheter design of the PVAC Gold® array may improve safety by reducing embolic events through avoidance of electrode 1-to-10 interaction and by better tissue contact due to the 20° forward tilt. Although clinical data with this new array are lacking so far, the PVAC system has been shown to be a promising tool for PVI. However, prospective studies especially with the novel array are required to determine its true role for catheter ablation of atrial fibrillation in the future.
Zusammenfassung
Die elektrische Isolation der Pulmonalvenen (PVI) ist nach wie vor ein entscheidender Endpunkt der interventionellen Behandlung von Vorhofflimmern (AF). Daher sind einige alternative „single-shot“ Kathetertechnologien wie der „Pulmonary Vein Ablation Catheter“ (PVAC®, Medtronic Inc., Minneapolis, MN, USA) entwickelt worden. Dieser Multielektrodenkatheter wird über einen Draht eingeführt und gibt eine phasenverschobene bipolare wie unipolare relativ niedrige Radiofrequenzenergie (RF) ab.
Sowohl die Untersuchungsdauer als auch die Durchleuchtungszeit sind für dieses System kürzer verglichen mit der gekühlten RF-Energie. Dies kann durch den Vorteil des gleichzeitigen Mappings und Abladierens bedingt sein, wobei die Signale während der Impulsabgabe artefaktbedingt nicht beurteilbar sind. Auch die Effektivität des PVAC-Katheters ist in randomisierten Studien vergleichbar mit anderen Technologien. Komplikationen treten bei PVAC-Therapie etwa gleich häufig auf wie bei gekühlter RF-Ablation und sind bei Kryoballonablation sogar geringfügig höher. Dennoch sollte dem Auftreten von Thrombembolien und Pulmonalvenenstenosen sowie einer effektiven Antikoagulation besonderes Augenmerk bei PVAC-PVIs gewidmet werden.
Das neue Design des PVAC Gold® Katheters wird möglicherweise die Sicherheit verbessern, indem das Thrombembolierisiko durch die fehlende Interaktion der Elektroden 1 und 10 und durch einen besseren Gewebekontakt durch eine 20° Vorwärtsneigung der Katheterspirale verringert wird. Diesbezüglich liegen bislang allerdings noch keine klinischen Daten vor. Zusammenfassend stellt das PVAC-System eine vielversprechende Alternative zur PVI dar. Prospektive Studien mit dem neuen Katheterdesign sind erforderlich, um den zukünftigen Stellenwert des Verfahrens beurteilen zu können.



Similar content being viewed by others
References
Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, Hindricks G, Kirchhof P, Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, Vardas P, Al-Attar N, Alfieri O, Angelini A, Blomstrom-Lundqvist C, Colonna P, De Sutter J, Ernst S, Goette A, Gorenek B, Hatala R, Heidbuchel H, Heldal M, Kristensen SD, Le Heuzey JY, Mavrakis H, Mont L, Filardi PP, Ponikowski P, Prendergast B, Rutten FH, Schotten U, Van Gelder IC, Verheugt FW (2012) Focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation. Developed with the special contribution of the European heart rhythm association. Eur Heart J 33:2719–2747
Gaita F, Leclercq JF, Schumacher B, Scaglione M, Toso E, Halimi F, Schade A, Froehner S, Ziegler V, Sergi D, Cesarani F, Blandino A (2011) Incidence of silent cerebral thromboembolic lesions after atrial fibrillation ablation may change according to technology used: comparison of irrigated radiofrequency, multipolar nonirrigated catheter and cryoballoon. J Cardiovasc Electrophysiol 22:961–968
Herrera Siklody C, Deneke T, Hocini M, Lehrmann H, Shin DI, Miyazaki S, Henschke S, Fluegel P, Schiebeling-Romer J, Bansmann PM, Bourdias T, Dousset V, Haissaguerre M, Arentz T (2011) Incidence of asymptomatic intracranial embolic events after pulmonary vein isolation: comparison of different atrial fibrillation ablation technologies in a multicenter study. J Am Coll Cardiol 58:681–688
Haines DE, Stewart MT, Barka ND, Kirchhof N, Lentz LR, Reinking NM, Urban JF, Halimi F, Deneke T, Kanal E (2013) Microembolism and catheter ablation II: effects of cerebral microemboli injection in a canine model. Circ Arrhythm Electrophysiol 6:23–30
Haines DE, Stewart MT, Dahlberg S, Barka ND, Condie C, Fiedler GR, Kirchhof NA, Halimi F, Deneke T (2013) Microembolism and catheter ablation I: a comparison of irrigated radiofrequency and multielectrode-phased radiofrequency catheter ablation of pulmonary vein ostia. Circ Arrhythm Electrophysiol 6:16–22
Verma A, Debruyne P, Nardi S, Deneke T, Degreef Y, Spitzer S, Balzer JO, Boersma L (2013) Evaluation and reduction of asymptomatic cerebral embolism in ablation of atrial fibrillation, but high prevalence of chronic silent infarction: results of the ERACE trial. Circ Arrhythm Electrophysiol 6:835–842
Zellerhoff S, Ritter MA, Kochhauser S, Dittrich R, Kobe J, Milberg P, Korsukewitz C, Dechering DG, Pott C, Wasmer K, Leitz P, Guner F, Eckardt L, Mönnig G (2014) Modified phased radiofrequency ablation of atrial fibrillation reduces the number of cerebral microembolic signals. Europace 16:341–346
Wieczorek M, Hoeltgen R, Brueck M (2013) Does the number of simultaneously activated electrodes during phased RF multielectrode ablation of atrial fibrillation influence the incidence of silent cerebral microembolism? Heart Rhythm 10:953–959
Compier MG, Leong DP, Marsan NA, Delgado V, Zeppenfeld K, Schalij MJ, Trines SA (2013) Duty-cycled bipolar/unipolar radiofrequency ablation for symptomatic atrial fibrillation induces significant pulmonary vein narrowing at long-term follow-up. Europace 15:690–696
Dong J, Vasamreddy CR, Jayam V, Dalal D, Dickfeld T, Eldadah Z, Meininger G, Halperin HR, Berger R, Bluemke DA, Calkins H (2005) Incidence and predictors of pulmonary vein stenosis following catheter ablation of atrial fibrillation using the anatomic pulmonary vein ablation approach: results from paired magnetic resonance imaging. J Cardiovasc Electrophysiol 16:845–852
von Bary C, Dornia C, Kirchner G, Weber S, Fellner C, Nisenbaum D, Georgieva M, Stroszczynski C, Hamer OW (2013) Esophageal tissue injury following pulmonary vein isolation using the PVAC: assessment by endoscopy and magnetic resonance imaging. Pacing Clin Electrophysiol 36:477–485
Bittner A, Mönnig G, Zellerhoff S, Pott C, Kobe J, Dechering D, Milberg P, Wasmer K, Eckardt L (2011) Randomized study comparing duty-cycled bipolar and unipolar radiofrequency with point-by-point ablation in pulmonary vein isolation. Heart Rhythm 8:1383–1390
Bulava A, Hanis J, Sitek D, Osmera O, Karpianus D, Snorek M, Rehouskova K, Tousek F, Pesl L (2010) Catheter ablation for paroxysmal atrial fibrillation: a randomized comparison between multielectrode catheter and point-by-point ablation. Pacing Clin Electrophysiol 33:1039–1046
De Greef Y, Buysschaert I, Schwagten B, Stockman D, Tavernier R, Duytschaever M (2014) Duty-cycled multi-electrode radiofrequency vs. conventional irrigated point-by-point radiofrequency ablation for recurrent atrial fibrillation: comparative 3-year data. Europace 16:820–825
Malmborg H, Lonnerholm S, Blomstrom P, Blomstrom-Lundqvist C (2013) Ablation of atrial fibrillation with cryoballoon or duty-cycled radiofrequency pulmonary vein ablation catheter: a randomized controlled study comparing the clinical outcome and safety; the AF-COR study. Europace 15:1567–1573
Malmborg H, Christersson C, Lonnerholm S, Blomstrom-Lundqvist C (2013) Comparison of effects on coagulation and inflammatory markers using a duty-cycled bipolar and unipolar radiofrequency pulmonary vein ablation catheter vs. a cryoballoon catheter for pulmonary vein isolation. Europace 15:798–804
Ahsan SY, Flett AS, Lambiase PD, Segal OR (2010) First report of phrenic nerve injury during pulmonary vein isolation using the ablation frontiers pulmonary vein ablation catheter. J Interv Card Electrophysiol 29:187–190
Mulder AA, Wijffels MC, Wever EF, Boersma LV (2011) Pulmonary vein isolation and left atrial complex-fractionated atrial electrograms ablation for persistent atrial fibrillation with phased radio frequency energy and multi-electrode catheters: efficacy and safety during 12 months follow-up. Europace 13:1695–1702
Hummel J, Michaud G, Hoyt R, DeLurgio D, Rasekh A, Kusumoto F, Giudici M, Dan D, Tschopp D, Calkins H, Boersma L (2014) Phased RF ablation in persistent atrial fibrillation. Heart Rhythm 11:202–209
Compliances with ethical guidelines
Conflict of interest
G. Mönnig and L. Eckardt state the following: Dr. Eckardt and Dr. Mönnig have received lecture honoraria and travel grants from Astra/Zeneca, Bayer, Johnson&Johnson, Biotronik, Boehringer Ingelheim, Boston Scientific, Bristol–Myers Squibb, Medtronic, Pfizer, Sanofi Aventis, and St. Jude Medical. Dr. Eckardt has received research grants from Biotronik, St. Jude Medical, Sanofi, and Osypka. Dr Eckardt holds the Peter Osypka Professorship for experimental and clinical electrophysiology.
This article does not contain any studies with human or animal subjects.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mönnig, G., Eckardt, L. Multielectrode Pulmonary Vein Ablation Catheter (PVAC®). Herzschr Elektrophys 25, 236–240 (2014). https://doi.org/10.1007/s00399-014-0330-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00399-014-0330-x
Keywords
- Atrial fibrillation
- Pulmonary vein isolation
- Multielectrode catheter
- Pulmonary Vein Ablation Catheter
- Results and risks