Abstract
Purpose
To derive dietary patterns based on dietary energy density (DED), free sugars, SFA, and fiber and investigate association with odds of overweight/obesity in young adults.
Methods
Cross-sectional data from 625 young Australian adults (18–30 years) were used. Dietary patterns were derived using reduced rank regression based on dietary data from a smartphone food diary using DED, free sugars, SFA, and fiber density as response variables. Multivariable logistic regression was used to investigate associations between dietary patterns and odds of self-reported overweight/obesity (BMI ≥ 25 kg/m2).
Results
Two dietary patterns were identified (DP1 and DP2). DP-1 was positively correlated with DED, free sugars, and SFA, and inversely correlated with fiber density. It was characterized by higher sugar-sweetened beverages intake and lower vegetable intake, and associated with higher odds of overweight/obesity (OR: 1.22; 95% CI 1.05, 1.42). DP-2 was positively correlated with fiber density and free sugars, and inversely correlated with DED and SFA. It was characterized by higher sugar-sweetened beverages intake and lower non-lean red meat intake, and was not significantly associated with overweight/obesity.
Conclusion
An energy-dense dietary pattern high in free sugars and SFA and low in fiber was associated with higher odds of obesity in young adults. These findings support dietary interventions that target reductions in energy-dense foods and sugar-sweetened beverages.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diets high in energy-dense foods, such as processed meats, as well as high energy sugar-sweetened beverages have been associated with a greater risk of obesity and chronic disease [1]. Young adults often have energy-dense diets due to social norms, a preference for packaged and convenience foods, and low cooking confidence [2,3,4]. Moreover, young adults are the most at-risk age group for weight gain and developing chronic diseases in later life; by 2030, it is predicted that 80% of young Australian adults will have overweight or obesity [5]. Identification of risk factors for obesity in young adulthood will inform the design of dietary interventions to reduce the tracking of unhealthy diets and chronic disease risk into later life.
Dietary pattern methodologies, such as reduced rank regression, consider the frequency and combination of foods consumed, providing a more holistic approach to characterizing overall diets rather than focusing on single foods and nutrients [6]. Reduced rank regression is a hybrid approach that enables the creation of food-based dietary patterns that explain variation in multiple nutrient intakes known to be associated with a specific disease [7, 8], providing a policy-relevant link between nutrient and food-based guidelines [9]. With increasing consensus that energy-dense diets high in free sugars and saturated fats and low in fiber are associated with obesity risk [10], there is a need to examine these within the context of an overall dietary pattern.
Few studies have derived dietary patterns based on energy density, fat, and/or fiber intake and investigated their associations with obesity risk [11, 12]; and those that have, have focused on adolescence and demonstrated mixed results. In a cross-sectional study of 1251 Australian adolescents aged 17 years, an energy-dense dietary pattern high in total fat and low in fiber was associated with higher waist circumference, but not BMI, in girls only. [11] In contrast, a cross-sectional analysis of European and Australian adolescent samples identified a similar dietary pattern associated with BMI in boys. [13] Since autonomous eating behaviors are established in young adulthood, [14] understanding the specific foods that characterize an energy-dense diet in this age group, as well as associations with overall diet quality and obesity, will inform targeted dietary interventions and policies to improve diets and health outcomes. To our knowledge, no studies have incorporated free sugars into the creation of such dietary patterns. Free sugars include all sugars added by the manufacturer, cook, or consumer and sugars naturally present in juiced or pureed fruit and vegetables, but exclude sugars that naturally occur in dairy products and intact fruit and vegetables [15]. Free sugars, as opposed to total or added sugars, have been identified as most strongly associated with poor health outcomes, including obesity, and are a key component of World Health Organization dietary recommendations [10, 15]. With the high intake of free sugars in young adults, understanding their role as part of an overall dietary patterns will provide new insights into young adult eating behaviors. Thus, this study aimed to derive dietary patterns based on dietary energy density (DED), percentage of energy (%E) from free sugars and SFA, and fiber density in young Australian adults and to investigate their cross-sectional associations with sociodemographic characteristics, diet quality and odds of overweight/obesity.
Methods
Subjects and study design
This study used data from the Measuring Eating in everyday Life Study (MEALS), a cross-sectional study conducted between April 2015 and April 2016 to examine eating patterns in young adults [3, 16]. Participants were aged between 18 and 30 years, living in Victoria, Australia. Pregnant or lactating women were considered ineligible to participate in the study because of potential changes in their eating patterns [17]. Recruitment was conducted using social media (Facebook, Twitter), poster advertisements, and flyers. After providing written consent, participants completed an online questionnaire (via Qualtrics, an online questionnaire hosting platform) and the FoodNow real-time, food diary smartphone application (app). Participants were compensated for their time with a $25 voucher. Reporting was guided by the STROBE-nut guidelines for nutritional epidemiology (Table S1).
Study measures
Dietary intake
Participants used the FoodNow app to record all foods and beverages they consumed over four non-consecutive days (3 weekdays and 1 weekend day). To represent usual intake and to maximize our sample, participants were excluded from the present analysis if they did not complete three or four days of food diaries. Data were collected over an eight-day period to account for daily variations in food consumption. Before each eating occasion, participants were encouraged to take two images of their food and beverage items alongside a standardized business card [18]. If it was not possible to take an image, participants could bypass this step by selecting ‘No image’. Participants were then prompted to provide a text description containing information such as the type, brand, and amount of food they consumed, and had the option to provide a voice recording. The text description was mandatory, whereas the collection of images and voice recordings was optional but highly encouraged by research staff. Following each eating occasion, participants were prompted by the FoodNow app to answer a food wastage question and take an image of any leftover food items to control for over-reporting of food consumption. Participants were provided with a detailed instruction manual, frequently asked questions and a YouTube video tutorial demonstrating how to download and use the FoodNow app. These instructions also provided guidance on how to report the amount of a food or drink consumed, with a variety of possible measurement techniques. Trained nutritionists or dietitians coded the food intake data against the Food Standards Australia New Zealand AUSNUT 2011–13 food composition database and a purpose designed database was used to calculate nutrient intake from the FoodNow app [19]. The standardized business card was used as a size reference (fiducial marker) when assessing the images to assist with coding the amount of food or drink consumed. Total energy intake (kJ/day), %E from total fat, SFA, monounsaturated fat (MUFA), polyunsaturated fat (PUFA), protein, carbohydrates, total sugars and free sugars, and intake of dietary fiber (g/day), sodium (mg/day), calcium (mg/day), iron (mg/day), and vitamin C (mg/day) were estimated. These nutrients were selected to reflect the main macro- and micro-nutrients correlated with food groups used to create the dietary patterns (e.g., calcium to reflect dairy product intake and vitamin C to reflect fruit and vegetable intake). In an evaluation of the FoodNow app in a sample of 90 young adults, energy intake measured by the FoodNow app has demonstrated good agreement against objectively measured energy expenditure [18]. DED (kJ/100 g) was calculated by dividing total food energy (kJ) by total food weight (g), excluding all beverages, and multiplying by 100. The decision to exclude beverages was based on evidence that measuring DED using both food and beverages may disproportionately affect DED values and lessen the strength of associations with outcome variables [20]. Average food and nutrient intakes were estimated for each participant using the mean of the three or four days of intake from the FoodNow app.
Dietary patterns
Information on food and beverage intakes from the FoodNow app was used to estimate dietary patterns. Fifty food and beverage groups (g/day) were created based on comparable nutrient compositions and the AUSNUT 2011–13 food group classification system [19] (Table S2). Foods were categorized into the following food groups: fruit (n = 5), vegetables (n = 4), cereals (n = 8), fats and oils (n = 2), dairy (n = 7), meats and alternatives (n = 10), soups, sauces, spreads, and condiments (n = 4), snacks and confectionery (n = 5), non-alcoholic beverages (n = 2), and alcoholic beverages (n = 3).
Dietary patterns were derived using reduced rank regression. Reduced rank regression derives linear combinations (factors) of food and beverage intake data that maximize the explained variation in intermediate response variables that are hypothesized to be related to a particular health outcome [7]. The number of dietary patterns extracted depends on the number of response variables and consistent with previous application of reduced rank regression, only dietary patterns that represented more than 10% of the variation in the response variables were used in regression analyses [21]. In these analyses, four nutrients known to be associated with obesity risk were used as response variables: DED (kJ/100 g), fiber density (g/MJ), free sugars (%E), and SFA (%E). These nutrients were selected based on evidence from the World Health Organization’s report on chronic disease prevention that DED, fiber density, free sugars, and fat intakes are strongly associated with obesity risk [10, 22]. Previous research has provided evidence to support using these variables when assessing obesity risk [12, 23].
Sensitivity analyses were performed to test the robustness of the derived dietary patterns. First, usual dietary intake was derived based on three or four days of FoodNow data using the web-based statistical program Multiple Source Method [24]. Usual dietary intake was estimated by (1) including consumption frequency as a covariate using population-specific proportions of food group intake from the Australian Health Survey [25] and (2) assuming all individuals were habitual consumers. Second, new dietary patterns were created in a random 50% split sample. Tucker’s coefficient of congruence was used to assess comparability between the dietary patterns [26] derived in the full sample using average intakes, usual intakes, and a 50% split sample. A coefficient of r ≥ 0.95 was considered equal, while r in the range of 0.85 to 0.94 indicated fair similarity. The coefficient of congruence was also calculated to assess the effect of excluding energy intake misreporters on the reproducibility of the dietary patterns.
Diet quality
To determine whether dietary patterns were associated with overall diet quality, diet quality was estimated from food and beverage intake data from the FoodNow app using the Dietary Guideline Index (DGI). The DGI is a food-based diet quality index designed to reflect consumption according to the 2013 Australian Dietary Guidelines (Table S3) and is detailed elsewhere [27]. Briefly, the DGI-2013 comprises ten recommended dietary components (food variety, fruit, vegetables, total and wholegrain cereals, total and lean meat and alternatives, dairy and alternatives, and total beverage and water intake) and six discouraged dietary components (discretionary foods, SFA, added salt, extra sugar, and alcohol) [27]. As added salt was not recorded in the FoodNow app, this component of the DGI-2013 was omitted for this study. DGI-2013 component scores ranged between 0 and 10, and sub-component scores ranged between 0 and 5. Cut-offs for the components were guided by the Australian Dietary Guidelines’ age- and sex-specific recommendations. [27] Total DGI scores ranged between 0 and 120, with higher scores representing better diet quality.
Weight status
Participants were asked to self-report their weight (kg) and height (cm) in the online questionnaire [16]. Body mass index (BMI) was calculated as weight (kg)/height (m2). Overweight/obesity was classified as a binary variable using standard cut-offs of underweight/healthy weight (BMI < 25 kg/m2) and overweight/obesity (BMI ≥ 25 kg/m2). [28]
Confounders
Confounders were determined based on the existing literature and a DAGitty directed acyclic graph (Figure S1). Information on country of birth, education status, postcode, physical activity, and smoking habits were collected using the online questionnaire. Country of birth was operationalized as born in Australia or other. Education status was grouped into Year 12 or less, trade/certificate, and tertiary [29]. The Socio-Economic Indexes for Areas (SEIFA) Index for Relative Socio-economic Disadvantage was used to assess the socioeconomic status of participants [30]. Participants’ postcodes were used to assign a SEIFA score derived using low socioeconomic attribute data from the 2018 Australian Census such as low income and education and unskilled occupations. The SEIFA score was operationalized as low (most disadvantaged), medium, and high (least disadvantaged). Physical activity was collected using the International Physical Activity Questionnaire—Short Form. [31] Participants’ level of physical activity was assessed according to whether they met the Australian physical activity guidelines of at least 150 min of moderate-intensity or 75 min of vigorous-intensity physical activity per week [32]. Smoking habits were grouped as non-smoking or past/current smoker, as research suggests that the dietary behaviors of past and current smokers are similar [33]. Energy misreporting was determined by dividing energy intake (from the FoodNow app) by predicted total energy expenditure, applying age- and sex-specific equations to a BMI range, and assuming a ‘low active’ physical activity level of ≥ 1.4 and < 1.6. [34] For sensitivity analyses purposes, participants who were classified as misreporters (i.e., under-reporters and over-reporters) were identified based on the ± 1 SD (standard deviation) cut-off for energy misreporting [34].
Statistical analyses
Complete case analysis was used. Means and SD (continuous data) or percentages (categorical data) were used for descriptive statistics. Dietary patterns were treated as continuous variables in regression analyses. Dietary patterns were also categorized into tertiles for descriptive purposes and to confirm that regression analyses were consistent when treated as a continuous or categorical variable. For construct validity, linear regression was used to examine associations between dietary patterns (continuous; independent variables) and DGI, total energy and nutrient intakes (continuous; dependent variables) and were adjusted for age and sex. Multivariable linear regression was used to examine associations between dietary patterns (as continuous and tertiles; independent variables) and BMI (continuous; dependent variable). Multivariable logistic regression was used to examine associations between the dietary patterns (as continuous and tertiles; independent variables) and overweight/obesity (binary, dependent variable). These analyses were adjusted for age (continuous), sex (binary), country of birth (binary), level of education (categorical), SEIFA (categorical), physical activity (binary), smoking (binary), and energy misreporting (continuous). As sensitivity analyses, these regression analyses were run after excluding energy misreporters to determine the effect, if any, on the strength and direction of associations between dietary patterns, overweight/obesity and BMI. SAS (version 9.4; SAS Institute, Cary, NC) was used to derive the dietary patterns. Stata (version 16; StataCorp., College Station, TX, USA) was used to analyze the data. Statistical significance was set at p < 0.05.
Results
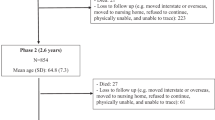
Of the 983 participants recruited into MEALS, 675 participants were included in the present analyses (mean age 24.3 [3.5 SD] years, 72% female). Most participants were born in Australia (72%), highly educated (69%), had low area-level disadvantage (61%), and met physical activity recommendations (64%). Twenty-four percent of participants had overweight or obesity. Participants were excluded if they did not complete the online questionnaire (n = 89), did not complete three or four days of dietary data (n = 85), or had missing data in the questionnaire (n = 17; Figure S2). The proportion of participants who completed 3 and 4 days of FoodNow data were 13 and 87%, respectively. Participant characteristics (age, sex) were comparable between three and four days (data not shown). Images and voice recordings were provided by 72 and 16% of the participants, respectively, with 16% providing both. Thirty percent of participants were identified as misreporting their energy intake (n = 103 under-reporting; n = 100 over-reporting). The excluded and included samples were similar concerning participants’ age, country of birth, SEIFA, and smoking status; however, more young adults in the included sample were female or tertiary educated (Table S4).
Dietary patterns
Table 1 presents the explained variation in food intakes and response variables and the correlations between dietary patterns, referred to as DP, and response variables. DP-1 was moderately positively correlated with DED (r = 0.54) and %E intake from SFA (r = 0.45) and moderately inversely correlated with fiber density (r = –0.60). It was also weakly positively correlated with %E intake from free sugars (r = 0.38). DP-2 was strongly positively correlated with %E intake from free sugars (r = 0.90). It was also weakly positively correlated with fiber density (r = 0.17) and weakly inversely correlated with %E intake from SFA (r = –0.37) and DED (r = –0.14). DP-3 and DP-4 were not further investigated, as they explained < 10% of the variation in response variables.
DP-1 was characterized by higher intakes of sugar-sweetened beverages, cakes and sweet biscuits and savory products and lower intakes of green and brassica vegetables, pome, berry, and stone fruit and other vegetables. DP-2 was characterized by higher intakes of sugar-sweetened beverages, fruit and vegetable juices and high-sugar products (e.g., chocolate spread) and lower intakes of animal-based fats, non-lean red meat and eggs (Table 2; Tables S4 and S5).
As shown in Table S7, DP-1 was associated with higher total energy intake and intake of total fat, SFA, free sugars, and sodium and lower intake of PUFA, dietary fiber, iron, and vitamin C. DP-2 was associated with higher intake of carbohydrates, total sugars, free sugars, dietary fiber, and vitamin C and lower intake of total fat, SFA, MUFA, PUFA, and protein. DP-1, but not DP-2, was associated with lower DGI.
Sensitivity analyses using Tucker’s coefficient of congruence indicated that factor loadings for dietary patterns derived when using average intakes were comparable to the factor loadings for average and usual intakes using a full and 50% split sample (r = 0.94–1.00). The coefficient of congruence also indicated similarities between the factor loadings for dietary patterns using average intakes and the sample of valid energy intake reporters (i.e., excluding energy misreporters; r = 0.91–0.94). Tables S5 and S6 provide the factor loadings for the dietary patterns derived using usual intakes, 50% split sample and in valid energy intake reporters.
Dietary patterns and demographics characteristics
Demographic characteristics of individuals across DP tertiles are provided in Table 3. Participants with a higher DP-1 score were more likely to be male, live in areas with higher area-level disadvantage, and not meet physical activity recommendations. Individuals with a higher DP-2 score were younger, female, and born in Australia.
Dietary patterns, obesity, and BMI
DP-1 was positively associated with odds of overweight/obesity (OR: 1.22; 95% CI 1.05, 1.42) and positively associated with BMI. A one-unit increase in DP-1 was associated with a 0.55 kg/m2 (SD 0.13) increase in BMI. Results were comparable when DP-1 was treated as a categorical variable (Table 4). DP-2 was not significantly associated with odds of overweight/obesity or BMI.
As sensitivity analyses to examine the robustness of these associations, we investigated whether excluding energy misreporters from the analyses influenced the relationship between dietary patterns and overweight/obesity and BMI. Associations were similar after excluding participants who had misreported their energy intake (Table S8). DP-1 remained positively associated with odds of overweight/obesity (OR: 1.23; 95% CI 1.02, 1.48) and positively associated with BMI, with a one-unit increase in DP-1 being associated with a 0.56 kg/m2 (SD 0.25) increase in BMI. The non-significant association remained between DP-2 and odds of overweight/obesity and BMI.
Discussion
This study used a real-time food diary smartphone app to identify an energy-dense dietary pattern high in free sugars and SFA and low in fiber that was associated with higher odds of overweight/obesity in young adults. The young adults who consumed this dietary pattern had a lower overall diet quality and were more likely to be male and live in areas of greater disadvantage, highlighting the need to better support these young adults to make healthier choices. Moreover, the design of dietary interventions in young adults would benefit from specifically targeting reductions in energy-dense foods high in free sugars and SFA and sugar-sweetened beverages.
The energy-dense dietary pattern identified in this study is consistent with the high intake of energy-dense foods and beverages among adolescents and young adults reported in other studies [35,36,37]. Data from the 2011–2013 Australian Health Survey indicate that the average DED of diets in Australian young adults aged 18–34 years is 740 kJ/100 g (vs. 723 kJ/100 g in our study), showing the generalizability of this pattern with the wider young adult cohort in Australia [35]. Moreover, the foods that characterized the dietary pattern in the present study were comparable with the high DED foods identified in these national data, including high intake of sweet biscuits and chocolate. The highest loading item in the dietary pattern identified in our study was sugar-sweetened beverages, which is known to be consumed most by young adult age groups [37]. Some energy-dense foods are also nutrient-dense (e.g., cheese and nuts), and the absence of these foods loading highly in this pattern suggests it is nutrient-poor dietary pattern. This is further supported by the inverse correlations with healthful nutrients, such as iron and vitamin C, which are likely attributable to low intake of lean meat and fruit and vegetables, respectively. Moreover, the inverse association with this dietary pattern and overall diet quality is consistent with our previous findings linking diet quality and obesity [38].
Research examining associations between energy-dense diets and obesity risk has shown mixed results [11, 39]. Direct comparisons with previous studies are challenging due to the lack of studies in young adults that have derived dietary patterns using reduced rank regression. A study in a nationally representative sample of US adults aged 20 years and over showed strong evidence that DED is positively associated with BMI and waist circumference [39], while two studies in adolescents that derived similar energy-dense and high-fat dietary patterns using reduced rank regression showed mixed associations with BMI. The authors of these studies postulated that mixed results may be partly due to the choice of response variables. As most research to date has focused on DED, SFA and fiber density, the present study is the first to derive dietary patterns based on free sugars intake. As free sugars intake has been implicated with greater risk of weight gain and type 2 diabetes than intake of total or added sugars [15], these findings will help inform future dietary interventions to improve diets in young adults. With high amounts of free sugars consumed globally [15], further research should determine the reproducibility of these dietary patterns in other young adult cohorts and examine their prospective associations with obesity.
Sugar-sweetened beverages were the highest positive loading item in both dietary patterns identified in this study. Previous research in MEALS has shown that sugar-sweetened beverages were consumed most often in the home and often while undertaking screen-based activities, such as watching TV [40], suggesting these may be appropriate targets for behavioral intervention to reduce intake in young adults. Only DP-1 was associated with lower diet quality and higher odds of overweight/obesity in this study, while these associations were not observed for DP-2. This difference in findings between DP-1 and DP-2 is likely attributable to the weak loadings for fruit and vegetables and wholegrain cereals in DP-2 which are high in fiber and can contribute to diets of lower energy density. In contrast, these foods were strongly inversely loaded in DP-1, as well as loading highly for SFA-rich foods, suggesting that very low intakes of fruit and vegetables and wholegrain cereals, coupled with high intakes of high-SFA and sugars foods and beverages. may be an integral component of the dietary pattern, consistent with lower diet quality, and higher odds of obesity. Regardless, these findings support a focus of interventions targeting reductions in sugar-sweetened beverages for reducing obesity risk, but also add to the wider body of literature on the adverse health outcomes associated with diets high in sugar-sweetened beverages, such as cardiovascular and oral health [41, 42].
These findings have the potential to inform food-based dietary guidelines for obesity prevention in young adults as they show the importance of considering foods and beverages as part of an overall dietary pattern. Our results reinforce recommendations to increase consumption of nutrient-dense foods high in fiber, such as vegetables, while minimizing energy-dense foods high in free sugars and SFA, such as cakes and sweet biscuits. Given the comparable strength of the factor loadings for these energy-dense foods (positively loaded) and nutrient-dense foods (inversely loaded) in the pattern, there is significant potential for developing dietary interventions that focus on swapping strategies, such as snacking on vegetables instead of cakes and sweet biscuits. In particular, a recent systematic review of dietary strategies has highlighted the benefits of individuals swapping energy-dense foods for nutrient-dense foods [43], supporting a focus on shifting this energy-dense dietary pattern toward a nutrient-dense pattern to improve overall diets and reduce obesity prevalence.
The present study has several strengths. A validated real-time food diary smartphone app was used to collect information on dietary intake. While all self-report dietary assessment methods involve measurement error [44], the FoodNow app was shown to have good agreement with objective measures of energy expenditure. Moreover, providing images as part of a dietary assessment tool was appropriate for use in this age group, as indicated by the majority of participants providing images [45]. This is consistent with research demonstrating that images can improve the accuracy of dietary assessment tools [46]. A further strength is the use of reduced rank regression to derive dietary patterns. By combining a priori and a posteriori information, this method can derive patterns of food group intake that may be more appropriate for the diseases of interest. Moreover, by examining multiple response variables, this technique can capture multiple dietary intake dimensions that reflect the underlying complexity of diet. However, this may also increase the complexity of interpretations and although sensitivity analyses demonstrated the robustness of the patterns identified, these patterns are specific to the dietary intake of the cohort and are limited in their generalizability to other cohorts. Future research should examine the reproducibility of these dietary patterns by replicating them in an independent young adult cohort.
Several limitations should be acknowledged. First, our findings are not generalizable to the wider young adult population, as the sample was predominantly female, tertiary educated, and from areas of low area-level disadvantage. Although a lack of diversity is common in research from self-selected samples in this age range [47, 48], further efforts are required to recruit diverse samples. Second, the self-report nature of the dietary and anthropometric data may be subject to misreporting biases, and future research should consider collecting data on waist circumference. Third, reverse causality cannot be discounted due to the cross-sectional study design, and although we adjusted for key confounders known to influence our associations, residual or unmeasured confounding may remain, such as sedentary behavior. Prospective research is needed to examine whether the energy-dense dietary patterns identified in this study are associated with the development of obesity in older adulthood.
This study identified an energy-dense dietary pattern high in free sugars and SFA and low in fiber that was associated with higher odds of obesity in young adults. Findings from this novel smartphone-based study offer insights into real-time methods for examining dietary patterns in young adults. These findings also inform the design of policies and interventions to improve diets in this critical age group; if intervened in young adulthood, improved diets have the potential to track into later adulthood and to improve their future health and that of their children. To improve overall dietary patterns in young adults, future research should design dietary interventions that target reductions in these energy-dense foods and sugar-sweetened beverages.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to Deakin University’s Human Research Ethics Committee procedures but are available from the senior author on reasonable request.
Code availability
NA.
Abbreviations
- BMI:
-
Body mass index
- DGI:
-
Dietary guideline index
- DP:
-
Dietary pattern
- DED:
-
Dietary energy density
- MEALS:
-
Measuring eating in everyday life study
- MUFA:
-
Monounsaturated fat
- PUFA:
-
Polyunsaturated fat
- SFA:
-
Saturated fat
- SEIFA:
-
Socio-economic index for areas
References
Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, Abdela J, Abdelalim A, Abdollahpour I, Abdulkader RS, Abebe HT, Abebe M, Abebe Z, Abejie AN, Abera SF, Abil OZ, Abraha HN, Abrham AR, Abu-Raddad LJ, Accrombessi MMK, Acharya D, Adamu AA, Adebayo OM, Adedoyin RA, Adekanmbi V, Adetokunboh OO, Adhena BM, Adib MG, Admasie A, Afshin A, Agarwal G, Agesa KM, Agrawal A, Agrawal S, Ahmadi A, Ahmadi M, Ahmed MB, Ahmed S, Aichour AN, Aichour I, Aichour MTE, Akbari ME, Akinyemi RO, Akseer N, Al-Aly Z, Al-Eyadhy A, Al-Raddadi RM, Alahdab F, Alam K, Alam T, Alebel A, Alene KA, Alijanzadeh M, Alizadeh-Navaei R, Aljunid SM, Alkerwi Aa, Alla F, Allebeck P, Alonso J, Altirkawi K, Alvis-Guzman N, Amare AT, Aminde LN, Amini E, Ammar W, Amoako YA, Anber NH, Andrei CL, Androudi S, Animut MD, Anjomshoa M, Ansari H, Ansha MG, Antonio CAT, Anwari P, Aremu O, Ärnlöv J, Arora A, Arora M, Artaman A, Aryal KK, Asayesh H, Asfaw ET, Ataro Z, Atique S, Atre SR, Ausloos M, Avokpaho EFGA, Awasthi A, Quintanilla BPA, Ayele Y, Ayer R, Azzopardi PS, Babazadeh A, Bacha U, Badali H, Badawi A, Bali AG, Ballesteros KE, Banach M, Banerjee K, Bannick MS, Banoub JAM, Barboza MA, Barker-Collo SL, Bärnighausen TW, Barquera S, Barrero LH, Bassat Q, Basu S, Baune BT, Baynes HW, Bazargan-Hejazi S, Bedi N, Beghi E, Behzadifar M, Behzadifar M, Béjot Y, Bekele BB, Belachew AB, Belay E, Belay YA, Bell ML, Bello AK, Bennett DA, Bensenor IM, Berman AE, Bernabe E, Bernstein RS, Bertolacci GJ, Beuran M, Beyranvand T, Bhalla A, Bhattarai S, Bhaumik S, Bhutta ZA, Biadgo B, Biehl MH, Bijani A, Bikbov B, Bilano V, Bililign N, Bin Sayeed MS, Bisanzio D, Biswas T, Blacker BF, Basara BB, Borschmann R, Bosetti C, Bozorgmehr K, Brady OJ, Brant LC, Brayne C, Brazinova A, Breitborde NJK, Brenner H, Briant PS, Britton G, Brugha T, Busse R, Butt ZA, Callender CSKH, Campos-Nonato IR, Campuzano Rincon JC, Cano J, Car M, Cárdenas R, Carreras G, Carrero JJ, Carter A, Carvalho F, Castañeda-Orjuela CA, Castillo Rivas J, Castle CD, Castro C, Castro F, Catalá-López F, Cerin E, Chaiah Y, Chang J-C, Charlson FJ, Chaturvedi P, Chiang PP-C, Chimed-Ochir O, Chisumpa VH, Chitheer A, Chowdhury R, Christensen H, Christopher DJ, Chung S-C, Cicuttini FM, Ciobanu LG, Cirillo M, Cohen AJ, Cooper LT, Cortesi PA, Cortinovis M, Cousin E, Cowie BC, Criqui MH, Cromwell EA, Crowe CS, Crump JA, Cunningham M, Daba AK, Dadi AF, Dandona L, Dandona R, Dang AK, Dargan PI, Daryani A, Das SK, Gupta RD, Neves JD, Dasa TT, Dash AP, Davis AC, Davis Weaver N, Davitoiu DV, Davletov K, De La Hoz FP, De Neve J-W, Degefa MG, Degenhardt L, Degfie TT, Deiparine S, Demoz GT, Demtsu BB, Denova-Gutiérrez E, Deribe K, Dervenis N, Des Jarlais DC, Dessie GA, Dey S, Dharmaratne SD, Dicker D, Dinberu MT, Ding EL, Dirac MA, Djalalinia S, Dokova K, Doku DT, Donnelly CA, Dorsey ER, Doshi PP, Douwes-Schultz D, Doyle KE, Driscoll TR, Dubey M, Dubljanin E, Duken EE, Duncan BB, Duraes AR, Ebrahimi H, Ebrahimpour S, Edessa D, Edvardsson D, Eggen AE, El Bcheraoui C, El Sayed Zaki M, El-Khatib Z, Elkout H, Ellingsen CL, Endres M, Endries AY, Er B, Erskine HE, Eshrati B, Eskandarieh S, Esmaeili R, Esteghamati A, Fakhar M, Fakhim H, Faramarzi M, Fareed M, Farhadi F, Farinha CSEs, Faro A, Farvid MS, Farzadfar F, Farzaei MH, Feigin VL, Feigl AB, Fentahun N, Fereshtehnejad S-M, Fernandes E, Fernandes JC, Ferrari AJ, Feyissa GT, Filip I, Finegold S, Fischer F, Fitzmaurice C, Foigt NA, Foreman KJ, Fornari C, Frank TD, Fukumoto T, Fuller JE, Fullman N, Fürst T, Furtado JM, Futran ND, Gallus S, Garcia-Basteiro AL, Garcia-Gordillo MA, Gardner WM, Gebre AK, Gebrehiwot TT, Gebremedhin AT, Gebremichael B, Gebremichael TG, Gelano TF, Geleijnse JM, Genova-Maleras R, Geramo YCD, Gething PW, Gezae KE, Ghadami MR, Ghadimi R, Ghasemi Falavarjani K, Ghasemi-Kasman M, Ghimire M, Gibney KB, Gill PS, Gill TK, Gillum RF, Ginawi IA, Giroud M, Giussani G, Goenka S, Goldberg EM, Goli S, Gómez-Dantés H, Gona PN, Gopalani SV, Gorman TM, Goto A, Goulart AC, Gnedovskaya EV, Grada A, Grosso G, Gugnani HC, Guimaraes ALS, Guo Y, Gupta PC, Gupta R, Gupta R, Gupta T, Gutiérrez RA, Gyawali B, Haagsma JA, Hafezi-Nejad N, Hagos TB, Hailegiyorgis TT, Hailu GB, Haj-Mirzaian A, Haj-Mirzaian A, Hamadeh RR, Hamidi S, Handal AJ, Hankey GJ, Harb HL, Harikrishnan S, Haro JM, Hasan M, Hassankhani H, Hassen HY, Havmoeller R, Hay RJ, Hay SI, He Y, Hedayatizadeh-Omran A, Hegazy MI, Heibati B, Heidari M, Hendrie D, Henok A, Henry NJ, Herteliu C, Heydarpour F, Heydarpour P, Heydarpour S, Hibstu DT, Hoek HW, Hole MK, Homaie Rad E, Hoogar P, Hosgood HD, Hosseini SM, Hosseinzadeh M, Hostiuc M, Hostiuc S, Hotez PJ, Hoy DG, Hsiao T, Hu G, Huang JJ, Husseini A, Hussen MM, Hutfless S, Idrisov B, Ilesanmi OS, Iqbal U, Irvani SSN, Irvine CMS, Islam N, Islam SMS, Islami F, Jacobsen KH, Jahangiry L, Jahanmehr N, Jain SK, Jakovljevic M, Jalu MT, James SL, Javanbakht M, Jayatilleke AU, Jeemon P, Jenkins KJ, Jha RP, Jha V, Johnson CO, Johnson SC, Jonas JB, Joshi A, Jozwiak JJ, Jungari SB, Jürisson M, Kabir Z, Kadel R, Kahsay A, Kalani R, Karami M, Karami Matin B, Karch A, Karema C, Karimi-Sari H, Kasaeian A, Kassa DH, Kassa GM, Kassa TD, Kassebaum NJ, Katikireddi SV, Kaul A, Kazemi Z, Karyani AK, Kazi DS, Kefale AT, Keiyoro PN, Kemp GR, Kengne AP, Keren A, Kesavachandran CN, Khader YS, Khafaei B, Khafaie MA, Khajavi A, Khalid N, Khalil IA, Khan EA, Khan MS, Khan MA, Khang Y-H, Khater MM, Khoja AT, Khosravi A, Khosravi MH, Khubchandani J, Kiadaliri AA, Kibret GD, Kidanemariam ZT, Kiirithio DN, Kim D, Kim Y-E, Kim YJ, Kimokoti RW, Kinfu Y, Kisa A, Kissimova-Skarbek K, Kivimäki M, Knudsen AKS, Kocarnik JM, Kochhar S, Kokubo Y, Kolola T, Kopec JA, Koul PA, Koyanagi A, Kravchenko MA, Krishan K, Kuate Defo B, Kucuk Bicer B, Kumar GA, Kumar M, Kumar P, Kutz MJ, Kuzin I, Kyu HH, Lad DP, Lad SD, Lafranconi A, Lal DK, Lalloo R, Lallukka T, Lam JO, Lami FH, Lansingh VC, Lansky S, Larson HJ, Latifi A, Lau KM-M, Lazarus JV, Lebedev G, Lee PH, Leigh J, Leili M, Leshargie CT, Li S, Li Y, Liang J, Lim L-L, Lim SS, Limenih MA, Linn S, Liu S, Liu Y, Lodha R, Lonsdale C, Lopez AD, Lorkowski S, Lotufo PA, Lozano R, Lunevicius R, Ma S, Macarayan ERK, Mackay MT, MacLachlan JH, Maddison ER, Madotto F, Magdy Abd El Razek H, Magdy Abd El Razek M, Maghavani DP, Majdan M, Majdzadeh R, Majeed A, Malekzadeh R, Malta DC, Manda A-L, Mandarano-Filho LG, Manguerra H, Mansournia MA, Mapoma CC, Marami D, Maravilla JC, Marcenes W, Marczak L, Marks A, Marks GB, Martinez G, Martins-Melo FR, Martopullo I, März W, Marzan MB, Masci JR, Massenburg BB, Mathur MR, Mathur P, Matzopoulos R, Maulik PK, Mazidi M, McAlinden C, McGrath JJ, McKee M, McMahon BJ, Mehata S, Mehndiratta MM, Mehrotra R, Mehta KM, Mehta V, Mekonnen TC, Melese A, Melku M, Memiah PTN, Memish ZA, Mendoza W, Mengistu DT, Mengistu G, Mensah GA, Mereta ST, Meretoja A, Meretoja TJ, Mestrovic T, Mezgebe HB, Miazgowski B, Miazgowski T, Millear AI, Miller TR, Miller-Petrie MK, Mini GK, Mirabi P, Mirarefin M, Mirica A, Mirrakhimov EM, Misganaw AT, Mitiku H, Moazen B, Mohammad KA, Mohammadi M, Mohammadifard N, Mohammed MA, Mohammed S, Mohan V, Mokdad AH, Molokhia M, Monasta L, Moradi G, Moradi-Lakeh M, Moradinazar M, Moraga P, Morawska L, Moreno Velásquez I, Morgado-Da-Costa J, Morrison SD, Moschos MM, Mouodi S, Mousavi SM, Muchie KF, Mueller UO, Mukhopadhyay S, Muller K, Mumford JE, Musa J, Musa KI, Mustafa G, Muthupandian S, Nachega JB, Nagel G, Naheed A, Nahvijou A, Naik G, Nair S, Najafi F, Naldi L, Nam HS, Nangia V, Nansseu JR, Nascimento BR, Natarajan G, Neamati N, Negoi I, Negoi RI, Neupane S, Newton CRJ, Ngalesoni FN, Ngunjiri JW, Nguyen AQ, Nguyen G, Nguyen HT, Nguyen HT, Nguyen LH, Nguyen M, Nguyen TH, Nichols E, Ningrum DNA, Nirayo YL, Nixon MR, Nolutshungu N, Nomura S, Norheim OF, Noroozi M, Norrving B, Noubiap JJ, Nouri HR, Nourollahpour Shiadeh M, Nowroozi MR, Nyasulu PS, Odell CM, Ofori-Asenso R, Ogbo FA, Oh I-H, Oladimeji O, Olagunju AT, Olivares PR, Olsen HE, Olusanya BO, Olusanya JO, Ong KL, Ong SKS, Oren E, Orpana HM, Ortiz A, Ortiz JR, Otstavnov SS, Øverland S, Owolabi MO, Özdemir R, P A M, Pacella R, Pakhale S, Pakhare AP, Pakpour AH, Pana A, Panda-Jonas S, Pandian JD, Parisi A, Park E-K, Parry CDH, Parsian H, Patel S, Pati S, Patton GC, Paturi VR, Paulson KR, Pereira A, Pereira DM, Perico N, Pesudovs K, Petzold M, Phillips MR, Piel FB, Pigott DM, Pillay JD, Pirsaheb M, Pishgar F, Polinder S, Postma MJ, Pourshams A, Poustchi H, Pujar A, Prakash S, Prasad N, Purcell CA, Qorbani M, Quintana H, Quistberg DA, Rade KW, Radfar A, Rafay A, Rafiei A, Rahim F, Rahimi K, Rahimi-Movaghar A, Rahman M, Rahman MHU, Rahman MA, Rai RK, Rajsic S, Ram U, Ranabhat CL, Ranjan P, Rao PC, Rawaf DL, Rawaf S, Razo-García C, Reddy KS, Reiner RC, Reitsma MB, Remuzzi G, Renzaho AMN, Resnikoff S, Rezaei S, Rezaeian S, Rezai MS, Riahi SM, Ribeiro ALP, Rios-Blancas MJ, Roba KT, Roberts NLS, Robinson SR, Roever L, Ronfani L, Roshandel G, Rostami A, Rothenbacher D, Roy A, Rubagotti E, Sachdev PS, Saddik B, Sadeghi E, Safari H, Safdarian M, Safi S, Safiri S, Sagar R, Sahebkar A, Sahraian MA, Salam N, Salama JS, Salamati P, Saldanha RDF, Saleem Z, Salimi Y, Salvi SS, Salz I, Sambala EZ, Samy AM, Sanabria J, Sanchez-Niño MD, Santomauro DF, Santos IS, Santos JV, Milicevic MMS, Sao Jose BP, Sarker AR, Sarmiento-Suárez R, Sarrafzadegan N, Sartorius B, Sarvi S, Sathian B, Satpathy M, Sawant AR, Sawhney M, Saxena S, Sayyah M, Schaeffner E, Schmidt MI, Schneider IJC, Schöttker B, Schutte AE, Schwebel DC, Schwendicke F, Scott JG, Sekerija M, Sepanlou SG, Serván-Mori E, Seyedmousavi S, Shabaninejad H, Shackelford KA, Shafieesabet A, Shahbazi M, Shaheen AA, Shaikh MA, Shams-Beyranvand M, Shamsi M, Shamsizadeh M, Sharafi K, Sharif M, Sharif-Alhoseini M, Sharma R, She J, Sheikh A, Shi P, Shiferaw MS, Shigematsu M, Shiri R, Shirkoohi R, Shiue I, Shokraneh F, Shrime MG, Si S, Siabani S, Siddiqi TJ, Sigfusdottir ID, Sigurvinsdottir R, Silberberg DH, Silva DAS, Silva JP, Silva NTD, Silveira DGA, Singh JA, Singh NP, Singh PK, Singh V, Sinha DN, Sliwa K, Smith M, Sobaih BH, Sobhani S, Sobngwi E, Soneji SS, Soofi M, Sorensen RJD, Soriano JB, Soyiri IN, Sposato LA, Sreeramareddy CT, Srinivasan V, Stanaway JD, Starodubov VI, Stathopoulou V, Stein DJ, Steiner C, Stewart LG, Stokes MA, Subart ML, Sudaryanto A, Sufiyan MaB, Sur PJ, Sutradhar I, Sykes BL, Sylaja PN, Sylte DO, Szoeke CEI, Tabarés-Seisdedos R, Tabuchi T, Tadakamadla SK, Takahashi K, Tandon N, Tassew SG, Taveira N, Tehrani-Banihashemi A, Tekalign TG, Tekle MG, Temsah M-H, Temsah O, Terkawi AS, Teshale MY, Tessema B, Tessema GA, Thankappan KR, Thirunavukkarasu S, Thomas N, Thrift AG, Thurston GD, Tilahun B, To QG, Tobe-Gai R, Tonelli M, Topor-Madry R, Torre AE, Tortajada-Girbés M, Touvier M, Tovani-Palone MR, Tran BX, Tran KB, Tripathi S, Troeger CE, Truelsen TC, Truong NT, Tsadik AG, Tsoi D, Tudor Car L, Tuzcu EM, Tyrovolas S, Ukwaja KN, Ullah I, Undurraga EA, Updike RL, Usman MS, Uthman OA, Uzun SB, Vaduganathan M, Vaezi A, Vaidya G, Valdez PR, Varavikova E, Vasankari TJ, Venketasubramanian N, Villafaina S, Violante FS, Vladimirov SK, Vlassov V, Vollset SE, Vos T, Wagner GR, Wagnew FS, Waheed Y, Wallin MT, Walson JL, Wang Y, Wang Y-P, Wassie MM, Weiderpass E, Weintraub RG, Weldegebreal F, Weldegwergs KG, Werdecker A, Werkneh AA, West TE, Westerman R, Whiteford HA, Widecka J, Wilner LB, Wilson S, Winkler AS, Wiysonge CS, Wolfe CDA, Wu S, Wu Y-C, Wyper GMA, Xavier D, Xu G, Yadgir S, Yadollahpour A, Yahyazadeh Jabbari SH, Yakob B, Yan LL, Yano Y, Yaseri M, Yasin YJ, Yentür GK, Yeshaneh A, Yimer EM, Yip P, Yirsaw BD, Yisma E, Yonemoto N, Yonga G, Yoon S-J, Yotebieng M, Younis MZ, Yousefifard M, Yu C, Zadnik V, Zaidi Z, Zaman SB, Zamani M, Zare Z, Zeleke AJ, Zenebe ZM, Zhang AL, Zhang K, Zhou M, Zodpey S, Zuhlke LJ, Naghavi M, Murray CJL (2018) Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392:1736–1788. https://doi.org/10.1016/S0140-6736(18)32203-7
Australian Bureau of Statistics (2014) Australian Health Survey: nutrition first results—foods and nutrients, 2011–12. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.007main+features22011-12. Accessed 20 Dec 2016
Sexton-Dhamu MJ, Livingstone KM, Pendergast FJ, Worsley A, McNaughton SA (2021) Individual, social–environmental and physical–environmental correlates of diet quality in young adults aged 18–30 years. Appetite. https://doi.org/10.1016/j.appet.2021.105175
Stok FM, de Vet E, de Ridder DTD, de Wit JBF (2016) The potential of peer social norms to shape food intake in adolescents and young adults: a systematic review of effects and moderators. Health Psychol Rev 10(3):326–340. https://doi.org/10.1080/17437199.2016.1155161
Hayes AJ, Lung TWC, Bauman A, Howard K (2016) Modelling obesity trends in Australia: unravelling the past and predicting the future. Int J Obes. https://doi.org/10.1038/ijo.2016.165
Schulze MB, Martínez-González MA, Fung TT, Lichtenstein AH, Forouhi NG (2018) Food based dietary patterns and chronic disease prevention. BMJ. https://doi.org/10.1136/bmj.k2396
Hoffmann K, Schulze MB, Schienkiewitz A, Nöthlings U, Boeing H (2004) Application of a new statistical method to derive dietary patterns in nutritional epidemiology. Am J Epidemiol 159(10):935–944. https://doi.org/10.1093/aje/kwh134
Livingstone KM, McNaughton S (2017) Dietary patterns by reduced rank regression are associated with obesity and hypertension in Australian adults. Br J Nutr. https://doi.org/10.1017/S0007114516004505
Kroke A (2004) Re: “Application of a new statistical method to derive dietary patterns in nutritional epidemiology.” Am J Epidemiol 160(11):1132. https://doi.org/10.1093/aje/kwh329
World Health Organization (2020) Healthy diet WHO Fact Sheet, No 394 (2015) http://www.who.int/mediacentre/factsheets/fs394/en/. Accessed 9 Mar 2020
Appannah G, Pot GK, Huang RC, Oddy WH, Beilin LJ, Mori TA, Jebb SA, Ambrosini GL (2015) Identification of a dietary pattern associated with greater cardiometabolic risk in adolescence. Nutr Metab Cardiovasc Dis 25(7):643–650. https://doi.org/10.1016/j.numecd.2015.04.007
Johnson L, Mander AP, Jones LR, Emmett PM, Jebb SA (2008) Energy-dense, low-fiber, high-fat dietary pattern is associated with increased fatness in childhood. Am J Clin Nutr 87(4):846–854. https://doi.org/10.1093/ajcn/87.4.846
Huybrechts I, Lioret S, Mouratidou T, Gunter MJ, Manios Y, Kersting M, Gottrand F, Kafatos A, De Henauw S, Cuenca-García M, Widhalm K, Gonzales-Gross M, Molnar D, Moreno LA, McNaughton SA (2017) Using reduced rank regression methods to identify dietary patterns associated with obesity: a cross-country study among European and Australian adolescents. Br J Nutr 117(2):295–305. https://doi.org/10.1017/S0007114516004669
Hebden L, Chan HN, Louie JC, Rangan A, Allman-Farinelli M (2015) You are what you choose to eat: factors influencing young adults’ food selection behaviour. J Hum Nutr Diet 28(4):401–408. https://doi.org/10.1111/jhn.12312
Mela DJ, Woolner EM (2018) Perspective: total, added, or free? what kind of sugars should we be talking about? Adv Nutr (Bethesda) 9(2):63–69. https://doi.org/10.1093/advances/nmx020
Pendergast FJ, Livingstone KM, Worsley A, McNaughton SA (2019) Examining the correlates of meal skipping in Australian young adults. Nutr J 18(1):24. https://doi.org/10.1186/s12937-019-0451-5
Illner A-K, Freisling H, Boeing H, Huybrechts I, Crispim S, Slimani N (2012) Review and evaluation of innovative technologies for measuring diet in nutritional epidemiology. Int J Epidemiol 41(4):1187–1203. https://doi.org/10.1093/ije/dys105
Pendergast FJ, Ridgers ND, Worsley A, McNaughton SA (2017) Evaluation of a smartphone food diary application using objectively measured energy expenditure. Int J Behav Nutr Phys Act 14(1):30. https://doi.org/10.1186/s12966-017-0488-9
Zealand FSAN (2013) AUSNUT 2011–13 food nutrient database. Food Standards Australia New Zealand, Canberra
Ledikwe JH, Blanck HM, Khan LK, Serdula MK, Seymour JD, Tohill BC, Rolls BJ (2005) Dietary energy density determined by eight calculation methods in a nationally representative United States population. J Nutr 135(2):273–278. https://doi.org/10.1093/jn/135.2.273
Livingstone KM, McNaughton SA (2018) Association between diet quality, dietary patterns and cardiometabolic health in Australian adults: a cross-sectional study. Nutr J 17(1):19–19. https://doi.org/10.1186/s12937-018-0326-1
World Health Organization (2003) Diet, nutrition and the prevention of chronic diseases. Joint FAO/WHO expert consultation. WHO technical report series. World Health Organization, Geneva
Sherafat-Kazemzadeh R, Egtesadi S, Mirmiran P, Gohari M, Farahani SJ, Esfahani FH, Vafa MR, Hedayati M, Azizi F (2010) Dietary patterns by reduced rank regression predicting changes in obesity indices in a cohort study: Tehran Lipid and Glucose Study. Asia Pac J Clin Nutr 19(1):22–32
Harttig U, Haubrock J, Knüppel S, Boeing H (2011) The MSM program: web-based statistics package for estimating usual dietary intake using the multiple source method. Eur J Clin Nutr 65(Suppl 1):S87-91. https://doi.org/10.1038/ejcn.2011.92
Australian Bureau of Statistics (2014) Australian Health Survey: Nutrition first results—food and nutrients, 2011–12. Australian Bureau of Statistics, Canberra
Lorenzo-Seva U, Berge JFMFT (2006) Tucker’s congruence coefficient as a meaningful index of factor similarity. Methodology 2(2):57–64. https://doi.org/10.1027/1614-2241.2.2.57
Thorpe MG, Milte CM, Crawford D, McNaughton SA (2016) A revised Australian Dietary Guideline Index and its association with key sociodemographic factors, health behaviors and body mass index in peri-retirement aged adults. Nutrients 8(3):160
World Health Organization (2020) Body mass index-BMI. World Health Organisation. https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi. Accessed 21 Sep 2020
Austalian Bureau of Statistics (2001) 1272.0—Australian standard classification of education (ASCED), 2001. Australian Bureau of Statistics. https://www.abs.gov.au/ausstats/abs@.nsf/Latestproducts/4D4A0EE3F0340BBCCA256AAF001FCA53?opendocument
Australian Bureau of Statistics (2018) Socio-economic indexes for areas. Australian Bureau of Statistics. https://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa
Craig C, Marshall A, Sjostrom M, Bauman A, Booth M, Ainsworth B, Pratt M, Ekelund U, Yngve A, Sallis J, Oja P (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exer 35(8):1381–1395. https://doi.org/10.1249/01.Mss.0000078924.61453.Fb
Australian Government Department of Health (2016) Australia’s physical activity and sedentary behaviour guidelines. http://www.health.gov.au/internet/main/publishing.nsf/content/health-pubhlth-strateg-phys-act-guidelines#apaadult. Accessed 6 Oct 2016
Worsley A, Wang W, Hunter W (2012) The relationships between eating habits, smoking and alcohol consumption, and body mass index among baby boomers. Appetite 58(1):7
Huang TT-K, Roberts SB, Howarth NC, McCrory MA (2005) Effect of screening out implausible energy intake reports on relationships between diet and BMI. Obes Res 13(7):1205–1217. https://doi.org/10.1038/oby.2005.143
Grech A, Rangan A, Allman-Farinelli M (2017) Social determinants and poor diet quality of energy-dense diets of australian young adults. Healthcare (Basel) 5(4):70. https://doi.org/10.3390/healthcare5040070
Livingstone KM, Pnosamy H, Riddell LJ, Cicerale S (2020) Demographic, behavioural and anthropometric correlates of food liking: a cross-sectional analysis of young adults. Nutrients 12(10):3078
Australian Institute of Health and Welfare (2019) Poor diet. AIHW. https://www.aihw.gov.au/reports/food-nutrition/poor-diet. Accessed 21 Sep 2020
Livingstone K, McNaughton S (2016) Diet quality is associated with obesity and hypertension in Australian adults: a cross sectional study. BMC Public Health. https://doi.org/10.1186/s12889-016-3714-5
Mendoza JA, Drewnowski A, Christakis DA (2007) Dietary energy density is associated with obesity and the metabolic syndrome in US adults. Diabetes Care 30(4):974–979. https://doi.org/10.2337/dc06-2188
McNaughton SA, Pendergast FJ, Worsley A, Leech RM (2020) Eating occasion situational factors and sugar-sweetened beverage consumption in young adults. Int J Behav Nutr Phys Act 17(1):71–71. https://doi.org/10.1186/s12966-020-00975-y
Malik VS, Li Y, Pan A, Koning LD, Schernhammer E, Willett WC, Hu FB (2019) Long-term consumption of sugar-sweetened and artificially sweetened beverages and risk of mortality in US adults. Circulation 139(18):2113–2125. https://doi.org/10.1161/CIRCULATIONAHA.118.037401
Valenzuela MJ, Waterhouse B, Aggarwal VR, Bloor K, Doran T (2020) Effect of sugar-sweetened beverages on oral health: a systematic review and meta-analysis. Eur J Public Health 31(1):122–129. https://doi.org/10.1093/eurpub/ckaa147
Grieger JA, Wycherley TP, Johnson BJ, Golley RK (2016) Discrete strategies to reduce intake of discretionary food choices: a scoping review. Int J Behav Nutr Phys Act 13(1):57. https://doi.org/10.1186/s12966-016-0380-z
Pendergast FJ, Leech RM, McNaughton SA (2017) Novel online or mobile methods to assess eating patterns. Curr Nutr Rep 6(3):212–227. https://doi.org/10.1007/s13668-017-0211-0
Kerr DA, Harray AJ, Pollard CM, Dhaliwal SS, Delp EJ, Howat PA, Pickering MR, Ahmad Z, Meng X, Pratt IS, Wright JL, Kerr KR, Boushey CJ (2016) The connecting health and technology study: a 6-month randomized controlled trial to improve nutrition behaviours using a mobile food record and text messaging support in young adults. Int J Behav Nutr Phys Act 13(1):52. https://doi.org/10.1186/s12966-016-0376-8
Boushey CJ, Spoden M, Zhu FM, Delp EJ, Kerr DA (2017) New mobile methods for dietary assessment: review of image-assisted and image-based dietary assessment methods. Proc Nutr Soc 76(3):283–294. https://doi.org/10.1017/S0029665116002913
Garcia-Meseguer MJ, Burriel FC, Garcia CV, Serrano-Urrea R (2014) Adherence to Mediterranean diet in a Spanish university population. Appetite 78:156–164. https://doi.org/10.1016/j.appet.2014.03.020
Thorpe MG, Kestin M, Riddell LJ, Keast RS, McNaughton SA (2014) Diet quality in young adults and its association with food-related behaviours. Public Health Nutr 17(8):1767–1775. https://doi.org/10.1017/s1368980013001924
Funding
MEALS was supported by an Australian Research Council Discovery Grant [DP130100713], SAM was supported by a National Health and Medical Research Council Career Development Fellowship Level 2 [ID1104636]. KML is supported by a National Health and Medical Research Council Emerging Leadership Fellowship [APP1173803]. FJP was supported by an Australian Postgraduate Award Stipend. BB is supported by an International Postgraduate Award Stipend.
Author information
Authors and Affiliations
Contributions
SAM and TW designed and led the MEALS. FJP contributed to the data collection and management of the MEALS. KML, BB and SAM designed the analysis. KML and MJS-D performed the statistical analysis for the manuscript and drafted the paper. All authors contributed to a critical review of the manuscript during the writing process. All authors approved the final version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
This study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Ethics approval was obtained for MEALS from the Deakin University Human Ethics Advisory Group (HEAG-H 11_2015).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Livingstone, K.M., Sexton-Dhamu, M.J., Pendergast, F.J. et al. Energy-dense dietary patterns high in free sugars and saturated fat and associations with obesity in young adults. Eur J Nutr 61, 1595–1607 (2022). https://doi.org/10.1007/s00394-021-02758-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02758-y