Abstract
Purpose
Low-grade inflammation and a diet high in salt are both established risk factors for cardiovascular disease. High potassium (K+) intake was found to counter increase in blood pressure due to high salt intake and may potentially also have protective anti-inflammatory effects. To better understand these interactions under normal physiological conditions, we investigated the relationships between 22 inflammatory mediators with 24-h urinary K+ in young healthy adults stratified by low, medium and high salt intake (salt tertiles). We stratified by ethnicity due to potential salt sensitivity in black populations.
Methods
In 991 healthy black (N = 457) and white (N = 534) adults, aged 20–30 years, with complete data for 24-h urinary sodium and K+, we analysed blood samples for 22 inflammatory mediators.
Results
We found no differences in inflammatory mediators between low-, mid- and high-sodium tertiles in either the black or white groups. In multivariable-adjusted regression analyses in white adults, we found only in the lowest salt tertile that K+ associated negatively with pro-inflammatory mediators, namely interferon gamma, interleukin (IL) -7, IL-12, IL-17A, IL-23 and tumour necrosis factor alpha (all p ≤ 0.046). In the black population, we found no independent associations between K+ and any inflammatory mediator.
Conclusion
In healthy white adults, 24-h urinary K+ associated independently and negatively with specific pro-inflammatory mediators, but only in those with a daily salt intake less than 6.31 g, suggesting K+ to play a protective, anti-inflammatory role in a low-sodium environment. No similar associations were found in young healthy black adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammation is involved in the development of cardiovascular disease [1,2,3]. Additionally, a diet high in salt (Na+) is another well-known risk factor for cardiovascular diseases, including hypertension [4]. It was recently reported that Na+ intake modulates the release of pro-inflammatory mediators [5,6,7]. These two cardiovascular risk factors may, therefore, be mechanistically involved. Interstitial Na+ rapidly achieves an equilibrium with plasma, and excess Na+ is then excreted by the kidneys [8]. However, osmotically inactive Na+ can also be stored in tissues, such as the skin, which in turn leads to changes in immune cell function and increased inflammation [9].
A diet high in potassium (K+) intake was shown to counter the usual increase in blood pressure in response to high salt intake [10, 11]. This finding suggests that a high K+ intake may have protective cardiovascular effects [12, 13]. As inflammation and a diet high in Na+ and low in K+ may be additive risk factors for the development of cardiovascular disease, a better understanding is required to establish the potential impact of K+ on cardiovascular health. As high K+ intake has a beneficial effect on blood pressure [14], as well as cardiovascular events and mortality [13], an additional mechanism of K+ may be its anti-inflammatory properties [15]. This notion is supported by a study indicating that K+ supplementation inhibited interleukin (IL) -17A production in human T lymphocytes that were induced by a salt load [5]. However, there is limited evidence on the role of K+ in the regulation of other inflammatory mediators, such as C-reactive protein (CRP), IL-6, and IL-23.
When examining Na+ and K+ handling, an essential factor to account for is black ethnicity. Black individuals have higher levels of sodium retention than their white counterparts [16]. Previous studies also reported a greater proportion of salt sensitivity in black populations [16]. The cardiovascular risk in black populations may be further increased based on their more pro-inflammatory profile when compared to white adults [17].
To better understand these potential mechanisms involved in the development of cardiovascular disease, we performed a hypothesis-generating work by investigating whether a detailed range of 22 pro- and anti-inflammatory mediators are associated with 24-h urinary K+ in young black and white adults. We specifically focussed on those with low, medium and high salt intake.
Methodology
Study population
This study forms part of the African prospective study on the early detection and identification of cardiovascular disease and hypertension (African-PREDICT) [18]. We recruited young black and white men and women, between the ages of 20 and 30 years. African-PREDICT included apparently healthy individuals who were HIV-uninfected; had a screening office brachial blood pressure of < 140 mmHg systolic and < 90 mmHg diastolic; had no self-reported previous diagnosis or used any medication for a chronic disease; and, if female, were not currently pregnant or lactating. We analysed data of participants who were included in the baseline phase of the African-PREDICT study (n = 1202). This study is a sub-cohort of a previously published larger cohort [17]. Participants on anti-inflammatory medication and with missing biochemical data (Na+, K+, and multiple inflammatory mediators) were additionally excluded resulting in a total of 991 participants. The exclusion of individuals with missing urine data (Na+ and K+) allowed for investigation of a more specific research question.
Questionnaires, anthropometry and physical activity measurements
Self-reported data with regard to demographic and lifestyle information were collected using a questionnaire. A 24-h dietary recall questionnaire was administered by a trained dietitian or nutritionist on the study day and on two subsequent days. The average daily energy intake was then calculated. Socio-economic status was calculated using a point system that was adapted from Kuppuswamy’s Socio-economic Status Scale [19] for a South African environment. Height, weight and waist circumference were measured using standard methods [18]. Body mass index (BMI) was calculated using weight (kg)/height (m)2. A compact, chest-worn accelerometric device (Actiheart4 CamNtech Ltd and CamNtech Inc, UK) was used to objectively measure physical activity over a maximum period of 7 days.
Ambulatory blood pressure
Participants were also fitted with a validated 24-h brachial ambulatory blood pressure monitor (Card(X)plore® CE120, Meditech, Budapest, Hungary). The apparatus was programmed to record every 30 min during the day (06h00 to 22h00) and every hour during the night (22h00 to 06h00) [20]. Participants had a mean successful recording rate of 88%.
24-h urine collection
Participants were instructed to collect a 24-h urine sample on a day that was convenient for them and the date was noted. The first urine of the day was to be discarded and entire urine passed thereafter was collected in the provided container, including the first urine of the following morning (day 2). The start and finish time were recorded. The protocol for 24-h urine collection followed the Pan American Health Organisation/World Health Organisation (PAHO/WHO) protocol for population-level Na+ determination in 24-h urine samples [21]. Incomplete urine collections were defined as a volume less than 300 mL per 24 h and/or a 24-h creatinine excretion of < 4 mmol or > 25 mmol in women and < 6 mmol or > 30 mmol in men [22].
Biological sampling and biochemical analyses
Participants fasted overnight for at least 8 h prior to attending the day of research measurements. Blood samples were collected from the median cubital vein. The samples were prepared according to the standardised protocol of the African-PREDICT study and stored at − 80 °C until analysis [18].
Urinary Na+, K+ and chloride were measured by means of ion-selective electrode potentiometry on the Cobas Integra® 400 plus (Roche, Basel, Switzerland), and creatinine concentrations were measured using the Creatinine Jaffé Gen.2 reagent (Roche, Basel, Switzerland). Daily urinary Na+ and K+ excretion (mmol/day) were calculated by multiplying the Na+, K+ and creatinine concentrations (mmol/L) of the 24-h urine by the total 24-h volume of urine (in litres). Daily salt intake was estimated from the 24-h urinary Na+ excretion by converting Na+ in mmol to mg: Na+ (mmol) × 23 = Na+ (mg) [23] and then applying the conversion: 1 g salt (NaCl) = 390 mg Na+ [23].
A MILLIPEX Map Human High Sensitivity T-Cell Magnetic Bead Panel (EMD Millipore, Merck, MO, USA) was used to analyse 21 cytokines. This multiplex panel was analysed using Luminex xMAP technology on the Luminex 200™ analyser.
Serum samples were analysed for high-sensitivity CRP, total cholesterol, low- and high-density lipoprotein cholesterol, glucose and γ-glutamyltransferase (GGT) (Cobas Integra® 400plus, Roche, Basel, Switzerland). Serum creatinine concentrations were measured using the Creatinine Jaffé Gen.2 reagent (Roche, Basel, Switzerland). Estimated creatinine clearance was determined using the Cockroft–Gault formula (Men [(140 − age) × weight in kg × 1.23]/serum creatinine or women [(140 − age) × weight in kg × 1.04]/serum creatinine). Estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease-Epidemiology (CKD-EPI) formula, without race in the equation, as the correction for race is not suggested for a South African population [24, 25]. Serum cotinine was analysed using a chemiluminescence method on the Immulite (Siemens, Erlangen, Germany) apparatus.
Statistical analyses
IBM®, SPSS® version 24 (IBM Corporation, Armonk, New York) was used for data analysis. GraphPad Prism 5.03 (GraphPad Software, San Diego) was used to develop all graphs. Continuous variables were inspected for normality using Q–Q plots as well as inspection of skewness and kurtosis. Variables with non-Gaussian distributions were logarithmically transformed. To substantiate the analyses by ethnicity, we investigated the interactions of ethnicity on the relationship between Na+, K+ and the full range of pro- and anti-inflammatory mediators. Based on the interactions, we divided our groups by ethnicity (Online Resource Table S1). Pro- to anti-inflammatory ratios were calculated based on the literatures [26, 27], and new ratios were suggested based on instances where pro-inflammatory mediators were higher and anti-inflammatory mediators were lower in the black and white groups. T test and Chi-square test were used to compare the profiles of black and white participants. We further divided our groups by Na+ tertiles, reflecting low, medium and high salt intake. Partial correlations and backward stepwise multiple regression were used to determine the relationship between K+ and pro- and anti-inflammatory mediators. Partial correlations were adjusted for age, sex and waist circumference. Variables included in backward stepwise multiple regression models were: K+, age, socio-economic status, AEE, waist circumference, total cholesterol, eGFR, cotinine, GGT, glucose and sex. In sensitivity analyses, we also determined whether components of the renin–angiotensin–aldosterone system contribute to the model. Multiple regression analyses displayed the last model in which potassium remained.
Results
The general characteristics of the participants (n = 991) are shown in Table 1. The black and white groups were similar in age (24.5 years; p = 0.92) with an equal distribution in sex (p = 0.71). When viewing the detailed inflammatory mediator profile of the two groups, the black group had higher pro-to-anti-inflammatory ratios than their white counterparts (p ≤ 0.021) as was seen in a previous study in this population [17].
There were no ethnic differences for Na+ excretion (p = 0.47), but black participants had lower urine levels of K+, with 94% black and 88% white participants having K+ levels below recommended levels [28]. Black participants had higher Na+/K+ ratios (p < 0.001) than the white group.
We determined the differences in inflammatory mediator concentrations according to Na+ tertiles (Online Resource Table S2). For all inflammatory mediators, there were generally no differences.
To establish whether a relationship exists between Na+ or K+ with inflammatory mediators, we performed partially adjusted regression analyses in the total group as well as black and white groups separately (adjusted for age, sex and waist circumference as well as ethnicity in the total group) (Online Resource Table S3). These analyses yielded minimal correlations mostly with K+ as indicated in detail in Online Resource Table S3.
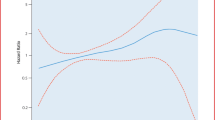
Due to previous reports indicating the importance of Na+/K+ balance [29], we then performed partial correlations between K+ and inflammatory mediators in the groups stratified by Na+ tertiles. In whites, we found several prominent results in the lowest Na+ tertile (T1). These include positive correlations between K+ and both interferon-inducible T-cell alpha chemoattractant (ITAC)/IL-5 and ITAC/IL-10. In T1, we also found negative correlations between K+ and interferon gamma (IFN-γ), IL-1β, IL-5, IL-6, IL-7, IL-8, IL-12, IL-17A, IL-21, IL-23, macrophage inflammatory protein 3-alpha (MIP-3α) and tumour necrosis factor alpha (TNF-α). Additionally, in the middle tertile (T2), K+ correlated inversely with IL-4 (Online Resource Fig. S1). In fully adjusted regression analyses (Fig. 1), these findings were confirmed where K+ associated negatively with the pro-inflammatory mediators IFN-γ, IL-7, IL-12, IL-17A, IL-23 and TNF-α, but only in the lowest Na+ tertile T1 (all p ≤ 0.046).
Multi-variable adjusted regression analyses showing the relationship between inflammatory mediators and K+ within each Na+ tertile in white adults. Each model was adjusted for: age, sex, socio-economic status, waist circumference, total cholesterol, glucose, gamma glutamyltransferase, cotinine, estimated glomerular filtration rate, activity energy expenditure. #p < 0.05
In the black population, with partial correlations, we found in the highest Na+ tertile (T3) positive correlations between K+ and both ITAC and IL-5, and negative correlations in the lowest tertile (T1) with ITAC/IL-4 and ITAC/IL-5 (all p ≤ 0.046) (Online Resource Fig. S2). However, these results lost significance in fully adjusted regression analyses (Fig. 2). We examined renin, angiotensin II and aldosterone’s impact on the model, all of which exhibited no effect (results not shown). We additionally examined the relationship between Na+ and inflammatory mediators, stratified by Na+, but found no significant correlations.
Multi-variable adjusted regression analyses showing the relationship between inflammatory mediators and K+ within each Na+ tertile in black adults. Each model was adjusted for: age sex, socio-economic status, waist circumference, total cholesterol, glucose, gamma glutamyltransferase, cotinine, estimated glomerular filtration rate, activity energy expenditure. #p < 0.05
Discussion
Low-grade systemic inflammation and Na+ are both risk factors for the development of cardiovascular disease [1,2,3,4]. It has been suggested that K+ may provide a protective anti-inflammatory effect [15]. Therefore, to better understand the possible mechanisms through which a high-salt environment may predispose one to higher cardiovascular disease risk (potentially due to the loss of the ‘protective’ anti-inflammatory role of K+), we examined the relationships between a detailed range of inflammatory mediators and 24-h urinary K+, in those with low, medium and high salt intake. When we stratified 991 young healthy black and white participants by Na+ excretion tertiles, we found negative independent relationships between urinary K+ and six pro-inflammatory mediators IFN-γ, IL-7, IL-12, IL-17A, IL-23 and TNF-α, but only in white adults and only in those within the lowest Na+ tertile (with an equivalent of 4.21 [0.63–6.31] g salt intake/day). These findings suggest that K+ may exert protective anti-inflammatory functions, but only in individuals with a low salt intake as reflected by the 24-h urinary Na+ excretion.
Previous studies have shown that a diet high in Na+ stimulates an inflammatory response [6, 8, 30]. In healthy human participants participating in the Mars520 study, Titze et al. found an increase in the pro-inflammatory mediators IL-6 and IL-23, as well as a decrease in the anti-inflammatory mediator IL-10 in those on a high-salt diet [7].
In support of our findings of several negative relationships between pro-inflammatory mediators and urinary K+, it was found that rats on a K+-supplemented diet had suppressed renal inflammation [15]. This was evident by a decrease in macrophage infiltration and nuclear factor kappa B (NF-κB), as well as a lower expression of cytokines [15]. In addition, a study involving healthy humans found K+ supplementation to have an inhibiting effect on the production of IL-17A by T lymphocytes induced by salt loading [5]. One potential mechanism through which K+ may suppress inflammation is via its anti-oxidant effect [5]. Increase in extracellular K+ leads to elevated membrane-Na+ pump activity [31]. This in turn results in hyperpolarization and ultimately a reduction in oxidase activity [31]. A second proposed mechanism is via K+ inhibiting the effects of Na+ on mitogen-activated protein kinase p38 which, when activated, leads to an immune response [5]. It has also been suggested that K+ may suppress the activation of NF-κB, which is involved in regulating genes relating to inflammation in the kidneys [15, 32, 33].
When we examined the relationship between K+ and inflammation, inverse relationships were seen with pro-inflammatory mediators, but not with anti-inflammatory mediators. This suggests a potential role of K+ in pro-inflammatory processes. What is of particular interest is that this protective association is only seen in the lowest Na+ tertile, with an average salt intake of 4.21 (0.63–6.31) g/day (or 10.7–107 mmol Na+/day). The mean intake for the second and third Na+ tertiles in the white group were 8.13 (6.31–10.0) g salt/day and 13.9 (10.0–50.1) g salt/day, respectively. These findings suggest that once Na+ intake exceeds the levels of the first Na+ tertile, or when the Na+/K+ equilibrium becomes significantly imbalanced, the protective effect of K+ may be lost. This may imply that while it is important to maintain an acceptable Na+/K+ ratio, it is also of importance to do so at the recommended levels. Our findings, thus, suggest a loss of mediation of pro-inflammatory mediators by K+ in individuals with increased Na+ intake.
As previously mentioned, it is also important to consider the role of ethnicity on the relationship between inflammatory mediators, K+ and Na+. While numerous studies have examined differences in inflammation between ethnic groups, global findings remain contradictory [34]. However, multiple studies performed in South African populations have found that black individuals display higher levels of pro-inflammatory markers and an overall more pro-inflammatory profile [17, 35,36,37]. When examining Na+, previous studies found that black adults have a predisposition for higher Na+ retention [16]. Based on previous reports, looking at salt sensitivity, black populations also have a greater response in blood pressure to Na+ [38]. Regardless, research into the role of Na+ and K+ in inflammation in any populations, but particularly black populations, is limited. While some studies have, to a limited extent, examined the role of K+ in inflammation [5, 15], to the best of our knowledge, none have examined this relationship stratified by ethnicity. This is of importance as studies have found ethnic differences in K+ excretion, with black populations being found to excrete less K+ than their white counterparts even when intake is matched [39].
Our findings were only present in the white group. Although, a previous study found that K+ supplementation protects against an increase in blood pressure in black populations in response to a salt load [10]. In our study with the focus on inflammation, this potentially protective effect on blood pressure was not seen in terms of potential anti-inflammatory effects. It is unknown whether this lack of association in the black group may be due to the effects of salt sensitivity. It should, however, be taken into account that the black group had particularly low urinary K+ levels. Only 6% of the black population had a K+ intake above the recommended minimum of 90 mmol/day [28], which may be a reason for the lack of association in this group. While protective associations are seen in the white adults, their mean K+ intake was also below the recommended daily K+ intake, albeit to a lesser extent than the black population. It would certainly be worth investigating whether an increase in K+ intake in both groups would result in greater anti-inflammatory responses. However, it is important to note that an increase in K+ levels should not be achieved by increasing calorie intake, but rather through the consumption of foods high in K+, such as fruits and vegetables [40].
A strength of our study is the absence of pre-existing chronic diseases, which gave us the opportunity to test our hypotheses in adults without an influence from pathology. Additionally, our study included a large panel of pro- and anti-inflammatory mediators which were analysed with a high-sensitivity kit. Although we included the renin–angiotensin–aldosterone system components in regression models, which yielded no contributory findings, the renin–angiotensin–aldosterone system is likely to be very important perhaps in those who have developed hypertension. In terms of limitations, the use of a single collection of 24‐h urine does not account for day‐to‐day variations in Na+ and K+ excretion.
In conclusion, in young apparently healthy white adults, we found significant negative relationships between 24-h urinary K+ and specific pro-inflammatory mediators, but only in those with a daily salt intake of less than 6.31 g. Our results suggest that K+ may play a protective, anti-inflammatory role in a low-sodium environment.
Access to Data
The study methodology has been published [18], whereas the data dictionary, statistical analysis, protocol and deidentified individual participant data will be made available upon reasonable request to the corresponding author in agreement with all co-authors.
Abbreviations
- CRP:
-
C-reactive protein
- Na+ :
-
Sodium
- K+ :
-
Potassium
- GM-CSF:
-
Granulocyte–macrophage colony-stimulating factor
- IFN-γ:
-
Interferon gamma
- IL-1 β:
-
Interleukin 1 beta
- IL-2:
-
Interleukin 2
- IL-4:
-
Interleukin 4
- IL-5:
-
Interleukin 5
- IL-6:
-
Interleukin 6
- IL-7:
-
Interleukin 7
- IL-8:
-
Interleukin 8
- IL-10:
-
Interleukin 10
- IL-12:
-
Interleukin 12
- IL-13:
-
Interleukin 13
- IL-17A:
-
Interleukin 17A
- IL-21:
-
Interleukin 21
- IL-23:
-
Interleukin 23
- ITAC:
-
Interferon-inducible T-cell alpha chemoattractant
- MIP-1α:
-
Macrophage inflammatory protein 1-alpha
- MIP-1β:
-
Macrophage inflammatory protein 1-beta
- MIP-3α:
-
Macrophage inflammatory protein 3-alpha
- NF-κB:
-
Nuclear factor kappa B
- TNFα:
-
Tumour necrosis factor alpha
References
McMaster WG, Kirabo A, Madhur MS, Harrison DG (2015) Inflammation, immunity, and hypertensive end-organ damage. Circ Res 116(6):1022–1033. https://doi.org/10.1161/CIRCRESAHA.116.303697
Harrison DG, Guzik TJ, Lob HE, Madhur MS, Marvar PJ, Thabet SR, Vinh A, Weyand CM (2011) Inflammation, immunity, and hypertension. Hypertension 57(2):132–140. https://doi.org/10.1161/HYPERTENSIONAHA.110.163576
Simons KH, de Jong A, Jukema JW, de Vries MR, Arens R, Quax PHA (2019) T cell co-stimulation and co-inhibition in cardiovascular disease: a double-edged sword. Nat Rev Cardiol 16:325–343. https://doi.org/10.1038/s41569-019-0164-7
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, Simons-Morton DG (2001) Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. New Engl J Med 344(1):3–10. https://doi.org/10.1056/NEJM200101043440101
Wen W, Wan Z, Ren K, Zhou D, Gao Q, Wu Y, Wang L, Yuan Z, Zhou J (2016) Potassium supplementation inhibits IL-17A production induced by salt loading in human T lymphocytes via p38/MAPK-SGK1 pathway. Exp Mol Pathol 100(3):370–377. https://doi.org/10.1016/j.yexmp.2016.03.009
Wilck N, Matus MG, Kearney SM, Olesen SW, Forslund K, Bartolomaeus H, Haase S, Mähler A, Balogh A, Markó L (2017) Salt-responsive gut commensal modulates T H 17 axis and disease. Nature 551(7682):585. https://doi.org/10.1038/nature24628
Yi B, Titze J, Rykova M, Feuerecker M, Vassilieva G, Nichiporuk I, Schelling G, Morukov B, Choukèr A (2015) Effects of dietary salt levels on monocytic cells and immune responses in healthy human subjects: a longitudinal study. Transl Res 166(1):103–110. https://doi.org/10.1016/j.trsl.2014.11.007
Kirabo A (2017) A new paradigm of sodium regulation in inflammation and hypertension. Am J Physiol-Reg I 313(6):706–710. https://doi.org/10.1152/ajpregu.00250.2017
Hofmeister LH, Perisic S, Titze J (2015) Tissue sodium storage: evidence for kidney-like extrarenal countercurrent systems? Pflügers Arch Eur J Physiol 467(3):551–558. https://doi.org/10.1007/s00424-014-1685-x
Luft F, Rankin L, Bloch R, Weyman A, Willis L, Murray R, Grim C, Weinberger M (1979) Cardiovascular and humoral responses to extremes of sodium intake in normal black and white men. Circulation 60(3):697–706. https://doi.org/10.1161/01.CIR.60.3.697
Morris RC Jr, Sebastian A, Forman A, Tanaka M, Schmidlin O (1999) Normotensive salt sensitivity: effects of race and dietary potassium. Hypertension 33(1):18–23. https://doi.org/10.1161/01.hyp.33.1.18
Whelton PK, He J, Louis GT (2003) Lifestyle modification for the prevention and treatment of hypertension. CRC Press, Boca Raton
O’Donnell M, Mente A, Rangarajan S, McQueen MJ, O’Leary N, Yin L, Liu X, Swaminathan S, Khatib R, Rosengren A (2019) Joint association of urinary sodium and potassium excretion with cardiovascular events and mortality: prospective cohort study. BMJ 364:772. https://doi.org/10.1136/bmj.l772
Geleijnse JM, Kok FJ, Grobbee DE (2003) Blood pressure response to changes in sodium and potassium intake: a metaregression analysis of randomised trials. J Hum Hypertens 17(7):471. https://doi.org/10.1038/sj.jhh.1001575
Wang W, Soltero L, Zhang P, Huang XR, Lan HY, Adrogue HJ (2007) Renal inflammation is modulated by potassium in chronic kidney disease: possible role of Smad7. Am J of Physiol-Renal 293(4):1123–1130. https://doi.org/10.1152/ajprenal.00104.2007
Palacios C, Wigertz K, Martin BR, Jackman L, Pratt JH, Peacock M, McCabe G, Weaver CM (2004) Sodium retention in black and white female adolescents in response to salt intake. J Clin Endocrinol Metab 89(4):1858–1863. https://doi.org/10.1210/jc.2003-031446
Crouch SH, Botha-Le Roux S, Delles C, Graham LA, Schutte AE (2020) Distinct inflammatory mediator patterns in young black and white adults: the African-predict study. Cytokine 126:154894. https://doi.org/10.1016/j.cyto.2019.154894
Schutte AE, Gona PN, Delles C, Uys AS, Burger A, Mels CM, Kruger R, Smith W, Fourie CM, Botha S (2019) The African Prospective study on the Early Detection and Identification of Cardiovascular disease and Hypertension (African-PREDICT): design, recruitment and initial examination. Eur J Prev Cardiol. https://doi.org/10.1177/2047487318822354
Patro BK, Jeyashree K, Gupta PK (2012) Kuppuswamy’s socioeconomic status scale 2010—the need for periodic revision. Indian J Rediatr 79(3):395–396. https://doi.org/10.1007/s12098-011-0517-7
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, De Simone G, Dominiczak A (2018) 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 39(33):3021–3104. https://doi.org/10.1093/eurheartj/ehy339
Campbell N, Cappuccio F, Hennis A, Barquera S, Rotter RC, Dary O, Wilks R, Ferrante D, Buscaglione R, Legowski B (2010) Protocol for population level sodium determination in 24-hour urine samples
Stolarz-Skrzypek K, Kuznetsova T, Thijs L, Tikhonoff V, Seidlerová J, Richart T, Jin Y, Olszanecka A, Malyutina S, Casiglia E (2011) Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA 305(17):1777–1785. https://doi.org/10.1001/jama.2011.574
Center for Disease Control and Prevention (2013) Sodium reduction toolkit: a global opportunity to reduce population-level sodium intake. https://www.cdc.gov/salt/sodium_toolkit.htm. Accessed 21 Sept 2019
van Deventer HE, George JA, Paiker JE, Becker PJ, Katz IJ (2008) Estimating glomerular filtration rate in black South Africans by use of the modification of diet in renal disease and Cockcroft–Gault equations. Clin Chem 54(7):1197–1202. https://doi.org/10.1373/clinchem.2007.099085
Seape T, Gounden V, van Deventer HE, Candy GP, George JA (2016) Cystatin C-and creatinine-based equations in the assessment of renal function in HIV-positive patients prior to commencing highly active antiretroviral therapy. Ann Clin Biochem 53(1):58–66. https://doi.org/10.1177/0004563215579695
Kilic T, Ural D, Ural E, Yumuk Z, Agacdiken A, Sahin T, Kahraman G, Kozdag G, Vural A, Komsuoglu B (2006) Relation between proinflammatory to anti-inflammatory cytokine ratios and long-term prognosis in patients with non-ST elevation acute coronary syndrome. Heart 92(8):1041–1046. https://doi.org/10.1136/hrt.2005.080382
Gogos CA, Drosou E, Bassaris HP, Skoutelis A (2000) Pro-versus anti-inflammatory cytokine profile in patients with severe sepsis: a marker for prognosis and future therapeutic options. J Infect Dis 181(1):176–180. https://doi.org/10.1086/315214
WHO (2012) Guideline: potassium intake for adults and children. World Health Organization, Geneva
Perez V, Chang ET (2014) Sodium-to-potassium ratio and blood pressure, hypertension, and related factors. Adv Nutr 5(6):712–741. https://doi.org/10.3945/an.114.006783
Foss JD, Kirabo A, Harrison DG (2016) Do high-salt microenvironments drive hypertensive inflammation? Am J Physiol Reg I 312(1):1–4. https://doi.org/10.1152/ajpregu.00414.2016
Kido M, Ando K, Onozato ML, Tojo A, Yoshikawa M, Ogita T, Fujita T (2008) Protective effect of dietary potassium against vascular injury in salt-sensitive hypertension. Hypertension 51(2):225–231. https://doi.org/10.1161/HYPERTENSIONAHA.107.098251
Donadelli R, Zanchi C, Morigi M, Buelli S, Batani C, Tomasoni S, Corna D, Rottoli D, Benigni A, Abbate M (2003) Protein overload induces fractalkine upregulation in proximal tubular cells through nuclear factor κB- and p38 mitogen-activated protein kinase-dependent pathways. J Am Soc Nephrol 14(10):2436–2446. https://doi.org/10.1097/01.ASN.0000089564.55411.7F
Ha H, Yu MR, Choi YJ, Kitamura M, Lee HB (2002) Role of high glucose-induced nuclear factor-κB activation in monocyte chemoattractant protein-1 expression by mesangial cells. J Am Soc Nephro 13(4):894–902
Miller M, Cappuccio F (2007) Ethnicity and inflammatory pathways-implications for vascular disease, vascular risk and therapeutic intervention. Curr Med Chem 14(13):1409–1425. https://doi.org/10.2174/092986707780831131
Schutte AE, Myburgh A, Olsen MH, Eugen-Olsen J, Schutte R (2012) Exploring soluble urokinase plasminogen activator receptor and its relationship with arterial stiffness in a bi-ethnic population: the SAfrEIC-study. Thromb Res 130(2):273–277. https://doi.org/10.1016/j.thromres.2011.10.034
Schutte A, Van Vuuren D, Van Rooyen J, Huisman H, Schutte R, Malan L, Malan N (2006) Inflammation, obesity and cardiovascular function in African and Caucasian women from South Africa: the POWIRS study. J Hum Hypertens 20(11):850. https://doi.org/10.1038/sj.jhh.1002065
Maritz M, Fourie CM, Van Rooyen JM, Moss SJ, Schutte AE (2016) Large artery stiffness is associated with gamma-glutamyltransferase in young, healthy adults: the African-PREDICT study. J Am Soc Hypertens 10(10):772–781. https://doi.org/10.1016/j.jash.2016.07.006
Weinberger MH, Miller JZ, Luft FC, Grim CE, Fineberg NS (1986) Definitions and characteristics of sodium sensitivity and blood pressure resistance. Hypertension 8(6_pt_2):II127. https://doi.org/10.1161/01.HYP.8.6_Pt_2.II127
Turban S, Miller ER, Ange B, Appel LJ (2008) Racial differences in urinary potassium excretion. J Am Soc Nephrol 19(7):1396–1402. https://doi.org/10.1681/ASN.2007101142
Anderson J, Young L, Long E (2002) Potassium and health. Food Nutr Ser Health 9:355
Acknowledgements
The authors are grateful to all individuals participating voluntarily in the study. The dedication of the support and research staff as well as students at the Hypertension Research and Training Clinic at the North-West University. Merck’s Donald Innes and Robert Hardcastle are also duly acknowledged.
Funding
The research funded in this manuscript is part of an ongoing research project financially supported by the South African Medical Research Council (SAMRC) with funds from National Treasury under its Economic Competitiveness and Support Package; the South African Research Chairs Initiative (SARChI) of the Department of Science and Technology and National Research Foundation (NRF) of South Africa (GUN 86895); SAMRC with funds received from the South African National Department of Health, GlaxoSmithKline R&D (Africa Non-Communicable Disease Open Lab grant), the UK Medical Research Council and with funds from the UK Government’s Newton Fund; as well as corporate social investment grants from Pfizer (South Africa), Boehringer-Ingelheim (South Africa), Novartis (South Africa), the Medi Clinic Hospital Group (South Africa) and in kind contributions of Roche Diagnostics (South Africa). CD is also supported by the British Heart Foundation (Centre of Research Excellence Awards RE/13/5/30177 and RE/18/6/34217).
Author information
Authors and Affiliations
Contributions
SHC, SBL and AES contributed to the conception or design. SHC, SBL, CD, LAG, AES contributed to the acquisition, analysis, or interpretation of data. SHC drafted the manuscript. SBL, CD, LAG and AES critically revised the manuscript. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding authors
Ethics declarations
Conflict of interest
Any opinion, findings, and conclusions or recommendations expressed in this material are those of the authors, and therefore, the NRF does not accept any liability in this regard. The authors declare that there is no conflict of interest.
Ethical standards
The study was approved by the Health Research Ethics Committee (HREC) of the North-West University (NWU-00058-18-A1), adheres to the 1964 Declaration of Helsinki and its later amendments and all participants in the study provided written informed consent prior to participation.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Crouch, S.H., Botha-Le Roux, S., Delles, C. et al. Inflammation and salt in young adults: the African-PREDICT study. Eur J Nutr 60, 873–882 (2021). https://doi.org/10.1007/s00394-020-02292-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-020-02292-3