Abstract
Purpose
To explore whether muscle strength, the insulin-like growth factor axis (IGF-axis), height, and body composition were associated with serum 25-hydroxyvitamin D [25(OH)D] and affected by winter vitamin D supplementation in healthy children, and furthermore to explore potential sex differences.
Methods
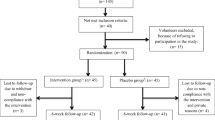
We performed a double-blind, placebo-controlled, dose–response winter trial at 55ºN. A total of 117 children aged 4–8 years were randomly assigned to either placebo, 10, or 20 µg/day of vitamin D3 for 20 weeks. At baseline and endpoint, we measured muscle strength with handgrip dynamometer, fat mass index (FMI), fat free mass index (FFMI), height, plasma IGF-1, IGF-binding protein 3 (IGFBP-3), and serum 25(OH)D.
Results
At baseline, serum 25(OH)D was positively associated with muscle strength, FFMI, and IGFBP-3 in girls only (all p < 0.01). At endpoint, baseline-adjusted muscle strength, FMI and FFMI did not differ between intervention groups. However, baseline-adjusted IGF-1 and IGFBP-3 were higher after 20 µg/day compared to placebo (p = 0.043 and p = 0.006, respectively) and IGFBP-3 was also higher after 20 µg/day compared to 10 µg/day (p = 0.011). Children tended to be taller after 20 µg/day compared to placebo (p = 0.064). No sex interactions were seen at endpoint.
Conclusions
Avoiding the winter-related decline in serum 25(OH)D may influence IGF-1 and IGFBP-3 in children. Larger trials are required to confirm these effects, and the long-term implication for linear growth.

Similar content being viewed by others
Abbreviations
- BIA :
-
Bioelectrical impedance analysis
- BMI :
-
Body mass index
- CV :
-
Coefficient of variation
- FFM :
-
Fat free mass
- FFMI :
-
Fat free mass index
- FM :
-
Fat mass
- FMI :
-
Fat mass index
- ICC :
-
Intraclass correlation coefficient
- IGF-1 :
-
Insulin-like growth factor 1
- IGFBP-3 :
-
IGF-binding protein-3
- LC-MS/MS :
-
Liquid chromatography tandem mass spectrometry
- ODIN :
-
Food-based solutions for optimal vitamin D nutrition and health through the life cycle
- VDR :
-
Vitamin D receptor
- 1,25(OH) 2 D :
-
1,25-dihydroxyvitamin D
- 25(OH)D :
-
25-hydroxyvitamin D
References
Webb AR, Kline L, Holick MF (1988) Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in boston and edmonton will not promote vitamin D3 synthesis in human skin. J Clin Endocrinol Metab 67:373–378. https://doi.org/10.1210/jcem-67-2-373
Mortensen C, Damsgaard CT, Hauger H et al (2016) Estimation of the dietary requirement for vitamin D in white children aged 4–8 y: a randomized, controlled, dose-response trial. Am J Clin Nutr 104:1310–1317. https://doi.org/10.3945/ajcn.116.136697
Institute of Medicine Food and Nutrition Board (2011) Dietary reference intakes for calcium and vitamin D. National Academies Press, Washington, DC
Nordisk Ministerråd (2014) Nordic Nutrition Recommendations 2012, integrating nutrition and physical activity, 5th edn, 1. oplag. Nordic Council of Ministers
Shaw NJ, Mughal MZ (2013) Vitamin D and child health: part 2 (extraskeletal and other aspects). Arch Dis Child 98:368–372. https://doi.org/10.1136/archdischild-2012-302585
Glerup H, Mikkelsen K, Poulsen L et al (2014) Hypovitaminosis D myopathy without biochemical signs of osteomalacic bone involvement. Calcif Tissue Int 66:419–424. https://doi.org/10.1007/s002230010085
Ceglia L (2008) Vitamin D and skeletal muscle tissue and function. Mol Aspects Med 29:407–414. https://doi.org/10.1016/j.mam.2008.07.002
Ward KA, Das G, Berry JL et al (2009) Vitamin D status and muscle function in post-menarchal adolescent girls. J Clin Endocrinol Metab 94:559–563. https://doi.org/10.1210/jc.2008-1284
Valtueña J, Gracia-Marco L, Huybrechts I et al (2013) Cardiorespiratory fitness in males, and upper limbs muscular strength in females, are positively related with 25-hydroxyvitamin D plasma concentrations in European adolescents: the HELENA study. QJM 106:809–821. https://doi.org/10.1093/qjmed/hct089
Foo LH, Zhang Q, Zhu K et al (2009) Low vitamin D status has an adverse influence on bone Mass, bone turnover, and muscle strength in Chinese adolescent girls. J Nutr 139:1002–1007. https://doi.org/10.3945/jn.108.102053
Carson EL, Pourshahidi LK, Hill TR et al (2015) Vitamin D, muscle function, and cardiorespiratory fitness in adolescents from the young hearts study. J Clin Endocrinol Metab 100:4621–4628. https://doi.org/10.1210/jc.2015-2956
El-Hajj Fuleihan G, Nabulsi M, Tamim H et al (2006) Effect of vitamin D replacement on musculoskeletal parameters in school children: a randomized controlled trial. J Clin Endocrinol Metab 91:405–412. https://doi.org/10.1210/jc.2005-1436
Ward KA, Das G, Roberts SA et al (2010) A randomized, controlled trial of vitamin D Supplementation upon musculoskeletal health in postmenarchal females. J Clin Endocrinol Metab 95:4643–4651. https://doi.org/10.1210/jc.2009-2725
McCarthy EK, Kiely M (2015) Vitamin D and muscle strength throughout the life course: a review of epidemiological and intervention studies. J Hum Nutr Diet 28:636–645. https://doi.org/10.1111/jhn.12268
Hazell TJ, DeGuire JR, Weiler HA (2012) Vitamin D: an overview of its role in skeletal muscle physiology in children and adolescents. Nutr Rev 70:520–533. https://doi.org/10.1111/j.1753-4887.2012.00510.x
Ameri P, Giusti A, Boschetti M et al (2013) Interactions between vitamin D and IGF-I: from physiology to clinical practice. Clin Endocrinol (Oxf) 79:457–463. https://doi.org/10.1111/cen.12268
Soliman AT, Al Khalaf F, AlHemaidi N et al (2008) Linear growth in relation to the circulating concentrations of insulin-like growth factor I, parathyroid hormone, and 25-hydroxy vitamin D in children with nutritional rickets before and after treatment: endocrine adaptation to vitamin D deficiency. Metabolism 57:95–102. https://doi.org/10.1016/j.metabol.2007.08.011
Bereket A, Cesur Y, Özkan B et al (2010) Circulating insulin-like growth factor binding protein-4 (IGFBP-4) is not regulated by parathyroid hormone and vitamin D in vivo: evidence from children with rickets. J Clin Res Pediatr Endocrinol 2:17–20
Hamilton B (2010) Vitamin D and human skeletal muscle. Scand J Med Sci Sports 20:182–190. https://doi.org/10.1111/j.1600-0838.2009.01016.x
Closa-Monasterolo R, Ferré N, Luque V et al (2011) Sex differences in the endocrine system in response to protein intake early in life. Am J Clin Nutr 94:1920S–1927S. https://doi.org/10.3945/ajcn.110.001123
Damsgaard CT, Harsløf LBS, Andersen AD et al (2016) Fish oil supplementation from 9 to 18 months of age affects the insulin-like growth factor axis in a sex-specific manner in Danish infants. Br J Nutr 115:782–790. https://doi.org/10.1017/S0007114515004973
Earthman CP, Beckman LM, Masodkar K, Sibley SD (2012) The link between obesity and low circulating 25-hydroxyvitamin D concentrations: considerations and implications. Int J Obes 36:387–396. https://doi.org/10.1038/ijo.2011.119
World Medical Association (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310:2191–2194. https://doi.org/10.1001/jama.2013.281053
Newman DG, Pearn J, Barnes A et al (1984) Norms for hand grip strength. Arch Dis Child 59:453–459. https://doi.org/10.1136/adc.59.5.453
Scientist WA, van den BHM, Epidemiologist, Scientist WA van den BHM, et al (2006) Validity and reproducibility of the Jamar dynamometer in children aged 4–11 years. Disabil Rehabil 28:1303–1309. https://doi.org/10.1080/09638280600631047
Molenaar HM (Ties), Selles RW, Zuidam JM et al (2009) Growth diagrams for grip strength in children. Clin Orthop Relat Res 468:217. https://doi.org/10.1007/s11999-009-0881-z
Hager-Ross C, Rosblad B (2002) Norms for grip strength in children aged 4–16 years. Acta Paediatr 91:617–625
World Health Organization Application tools WHO AnthroPlus software. In: WHO. http://www.who.int/growthref/tools/en/. Accessed 4 Jan 2016
Talma H, Chinapaw MJM, Bakker B et al (2013) Bioelectrical impedance analysis to estimate body composition in children and adolescents: a systematic review and evidence appraisal of validity, responsiveness, reliability and measurement error. Obes Rev 14:895–905. https://doi.org/10.1111/obr.12061
Andersen LB, Schnohr P, Schroll M, Hein HO (2000) All-cause mortality associated with physical activity during leisure time, work, sports, and cycling to work. Arch Intern Med 160:1621–1628. https://doi.org/10.1001/archinte.160.11.1621
Kiely M, Collins A, Lucey AJ et al (2016) Development, validation and implementation of a quantitative food frequency questionnaire to assess habitual vitamin D intake. J Hum Nutr Diet 1–10. https://doi.org/10.1111/jhn.12348
Aksglaede L, Sørensen K, Petersen JH et al (2009) Recent Decline in Age at Breast Development: The Copenhagen Puberty Study. Pediatrics 123:e932–e939. https://doi.org/10.1542/peds.2008-2491
Sørensen K, Aksglaede L, Petersen JH, Juul A (2010) Recent changes in pubertal timing in healthy danish boys: associations with body mass index. J Clin Endocrinol Metab 95:263–270. https://doi.org/10.1210/jc.2009-1478
Van den Beld WA, Van der Sanden GAC, Janssen AJWM. et al (2011) Comparison of 3 instruments to measure muscle strength in children: A prospective study. Eur J Paediatr Neurol 15:512–518. https://doi.org/10.1016/j.ejpn.2011.05.006
Beaudart C, Buckinx F, Rabenda V et al (2014) The effects of vitamin D on skeletal muscle strength, muscle mass, and muscle power: a systematic review and meta-analysis of randomized controlled trials. J Clin Endocrinol Metab 99:4336–4345. https://doi.org/10.1210/jc.2014-1742
Juul A, Dalgaard P, Blum WF et al (1995) Serum levels of insulin-like growth factor (IGF)-binding protein-3 (IGFBP-3) in healthy infants, children, and adolescents: the relation to IGF-I, IGF-II, IGFBP-1, IGFBP-2, age, sex, body mass index, and pubertal maturation. J Clin Endocrinol Metab 80:2534–2542. https://doi.org/10.1210/jcem.80.8.7543116
Ameri P, Giusti A, Boschetti M et al (2013) Vitamin D increases circulating IGF1 in adults: potential implication for the treatment of GH deficiency. Eur J Endocrinol 169:767–772. https://doi.org/10.1530/EJE-13-0510
Bogazzi F, Rossi G, Lombardi M et al (2010) Vitamin D status may contribute to serum insulin-like growth factor I concentrations in healthy subjects. J Endocrinol Invest 34:e200–e203. https://doi.org/10.3275/7228
Kremer R, Campbell PP, Reinhardt T, Gilsanz V (2009) Vitamin D status and its relationship to body fat, final height, and peak bone mass in young women. J Clin Endocrinol Metab 94:67–73. https://doi.org/10.1210/jc.2008-1575
Foo LH, Zhang Q, Zhu K et al (2009) Relationship between vitamin D status, body composition and physical exercise of adolescent girls in Beijing. Osteoporos Int 20:417–425. https://doi.org/10.1007/s00198-008-0667-2
Drincic AT, Armas LAG, Van Diest EE, Heaney RP (2012) Volumetric dilution, rather than sequestration best explains the low vitamin D status of obesity. Obes Silver Spring Md 20:1444–1448. https://doi.org/10.1038/oby.2011.404
Vimaleswaran KS, Berry DJ, Lu C et al (2013) Causal relationship between obesity and vitamin D status: bi-directional Mendelian randomization analysis of multiple cohorts. PLoS Med 10:e1001383
Arneson WL, Arneson DL (2013) Current methods for routine clinical laboratory testing of vitamin D levels. Lab Med 44:e38–e42. https://doi.org/10.1309/LMONQZQ27TIN7XFS
Acknowledgements
We thank all the participating children and their parents.
Funding
This project was funded by the European Commission (FP7/2007–2013) under Grant Agreement 613977 for the ODIN Integrated Project [Food-based solutions for optimal vitamin D nutrition and health through the life cycle http://www.odin-vitd.eu/].
Author information
Authors and Affiliations
Contributions
CTD and CMø: Designed the study; CMo, CTD, HH, and CMø: Conducted the research; CMo: Performed the statistical analyses and drafted the manuscript; CTD, CMø, HH, and MK: Assisted in the manuscript preparation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
This study involving humans was approved by the Committees on Biomedical Research Ethics for the Capital Region of Denmark (H-3-2014-022), and has, therefore, been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We obtained informed written consent from all parents. Any details that may have disclosed the identity of the participants were omitted. The study was registered at http://www.clinicaltrials.gov as NCT02145195.
Rights and permissions
About this article
Cite this article
Mortensen, C., Mølgaard, C., Hauger, H. et al. Winter vitamin D3 supplementation does not increase muscle strength, but modulates the IGF-axis in young children. Eur J Nutr 58, 1183–1192 (2019). https://doi.org/10.1007/s00394-018-1637-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-018-1637-x